Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2025) Volume 14, Issue 1
The Mechanisms of How Plant-Based Diets and Dietary Supplements Reduce COVID-19 Severity and Achieve Zero Mortality in High-Risk Elderly Patients
Dasaad Mulijono1,2*, Albert M Hutapea2, I Nyoman E Lister3, Mondastri K Sudaryo4 and Helwiah Umniyati52Department of Medicine, Indonesia College of Lifestyle Medicine, Tangerang, Indonesia
3Department of Biomolecular and Physiology, Prima University, Medan, Indonesia
4Department of Epidemiology, University of Indonesia, Jakarta, Indonesia
5Department of Community Nutrition, Yarsi University, Jakarta, Indonesia
Received: 22-Apr-2024, Manuscript No. JGGR-24-25539; Editor assigned: 24-Apr-2024, Pre QC No. JGGR-24-25539 (PQ); Reviewed: 08-May-2024, QC No. JGGR-24-25539; Revised: 17-Jan-2025, Manuscript No. JGGR-24-25539 (R); Published: 24-Jan-2025, DOI: 10.35248/2167-7182.2025.14.772
Abstract
The potential benefits of plant-based interventions in reducing the incidence and lessening the morbidity and mortality of COVID-19 have yet to be widely recognized. However, recent research suggests that these interventions could be effective. Our recent research publication utilized plant based diets and supplements for 3470 high-risk elderly COVID-19 patients. Our results were highly successful, as we achieved a zero mortality rate and none of our patients experienced worsening conditions or required hospitalization. This review article presents how plant based and supplement interventions can mitigate COVID-19 disease severity and avoid mortality. Our findings suggest that plant based and supplement interventions are effective and may be useful in managing corona virus patients.
Keywords
Plant-based; Supplement; COVID-19; Elderly; Severity; Mortality
Introduction
Several studies have demonstrated that a Plant Based Diet (PBD) can effectively treat chronic inflammatory diseases, such as obesity, atherosclerosis, hypertension, hyperlipidemia and hypercholesterolemia. Dietary interventions not only manage these diseases but can potentially reverse them. By reducing the consumption of foods that promote inflammation and contribute to chronic inflammatory diseases, one can further enhance the positive impact of a healthy diet. In our cardiology practice, we have observed remarkable results in patients suffering from chronic inflammation-related illnesses. These patients achieved remission with limited medication. Patients with hyperlipidemia could also meet their lipid targets according to International guidelines. We also noticed improved kidney function and successful management of glucose for Non-Insulin-Dependent Diabetes Mellitus (NIDDM) or glucose intolerance patients without the need for excessive medication or insulin. Furthermore, we witnessed a regression of coronary obstruction in numerous cardiac patients and there was a low occurrence of In-Stent Restenosis (ISR) [1].
Based on our previous successful experiences in treating our patients with chronic in-flammatory diseases using a Plant-Based Diet (PBD) and dietary supplements, we hypothe-sized that PBD could decrease the incidence and severity of SARS-CoV-2 infection and may save lives. Our clinical trial was conducted between April 2020 and July 2023, enrolling 3,470 mostly elderly COVID-19 patients, most of whom are cardiology patients with multiple comor-bidities. More than half of our study populations had been following PBD and taking dietary supplements before they contracted the coronavirus and were enrolled in our study. Even though they have comorbidities, all their clinical, laboratory and inflammatory profiles were satisfactorily controlled. Our research report is published separately. To the best of our knowledge, we are the pioneer in embarking on the PBD and providing dietary supplements to COVID-19 patients, which started at the beginning of the pandemic.
Materials and Methods
It is important to note that during the initial eighteen months of our investigation, no studies or recommendations emerged demonstrating the benefits of PBD and dietary supplementation in reducing the virus's incidence, severity and mortality. Fortunately, we observed the promising outcomes at the onset of our study. So, despite significant skepticism and opposition from our Indonesian peers towards PBD intervention, we continued our research. Later on, despite the publication of positive findings in a prestigious journal indicating the crucial role of PBD in managing the coronavirus, our research still gained minimal traction. Undertaking interventional research with close contact with COVID-19 patients when no medications or vaccines were available was also a high-risk endeavor and very challenging. Our perseverance in continuing our research is our firm belief in PBD and supplementations, supported by our extensive knowledge of PBD and supplementations, plus our positive experiences using such interventions to manage chronic inflammatory diseases for our cardiology patients. And most importantly, our ultimate goal is to save as many lives as possible, including ours.
We put forward the notion that PBD could potentially enhance Nitric Oxide (NO) availability, alter the gut microbiota, improve endothelial function, reduce inflammation, combat oxidative stress, boost mitochondrial function, extend telomeres and facilitate Caloric Restriction (CR) as a means to combat COVID-19. These mechanisms can potentially decrease the incidence, morbidity and mortality rate of COVID-19 patients. Severe inflammation and blood clotting are significant contributing factors to the high mortality rate of COVID-19 patients and PBD may help to prevent these complications. Field experts have recently validated our hypotheses, inspiring us to share our findings and publish our study [2].
Our research sets itself apart from other PBD studies in several ways, including utilizing raw PBD, carefully selecting foods to maximize their potential and paying close attention to food preparation techniques, such as avoiding high-temperature cooking of vegetables, which can negatively impact the NO content. Furthermore, we supplement our dietary intervention with vitamins, minerals and nutraceuticals to maximize antiinflammatory and antioxidant effects, minimize oxidative stress, improve NO availability and repair the endothelium. These supplements are selected based on our usual supplements used for cardiology patients to fight their chronic inflammatory diseases. However, only recently has the significance of vitamins, minerals and nutraceuticals in relation to COVID-19 been recognized. We hypothesize that by combining our dietary intervention with strategic supplementation, we can decrease the severity and fatality rates of the coronavirus to the greatest extent possible [3].
Results and Discussion
Mechanism of plant-based in decreasing incidence, morbidity and mortality of COVID-19
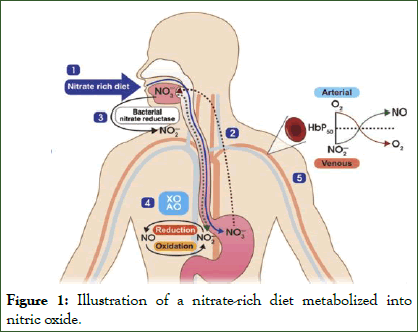
Mechanism of NO in fighting Coronavirus: NO is a naturally occurring molecule found in various cell types and organ systems and plays a crucial function in the cardiovascular. Its functions include regulating basal vascular tone, preventing platelet activation and limiting leukocyte adhesion to the endothelium. Furthermore, it significantly contributes to regulating myocardial contractility. Unfortunately, conditions like obesity, hypertension, hypercholesterolemia and NIDDM, which are commonly linked to risk factors for atherosclerosis, can lead to a decrease in NO release into the arterial wall due to synthesis dysfunction or enormous oxidative degradation. Studies on humans indicate that natural NO production reduces with age, which is relevant to the number of dis-eases that affect elderly people. It is believed that the elderly's NO deficiency may contribute to the severity and mortality of Coronavirus and the development of comorbidities. On the other hand, children and young adults (below 19 years old) have low COVID-19 mortality rates, which may be due to their high NO content. To measure our study population's NO, we used a salivary strip that has a 96% accuracy rate. We can improve our patients' NO readings by modifying their diet and lifestyle. Figure 1 illustrates the conversion of nitrate rich foods to nitric oxide [4].
Figure 1: Illustration of a nitrate-rich diet metabolized into nitric oxide.
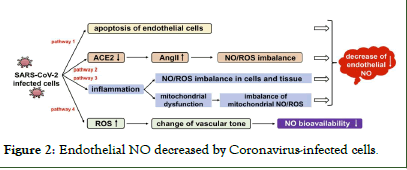
Figure 2: Endothelial NO decreased by Coronavirus-infected cells.
Figure 3: NO as a vasodilator, bronchodilator, anticoagulation, anti-inflammatory and anti-viral.
SCFAs are essential for regulating immune and inflammatory responses. By promoting mucin production and maintaining an acidic pH in the gut environment, harmful microbes are discouraged from growing. Furthermore, SCFAs maintain the integrity of the gut epithelium. So, epithelium leakage or translocation can be avoided. SCFAs are also powerful Histone Deacetylase (HDAC) inhibitors that can reduce inflammation by boosting the numbers and functions of regulatory T-, T helperand Th17 effector-cells. SCFAs can activate G Pro-Tein-Coupled Receptors (GPCRs) like GPR43 and inhibit the Nf-kB pathway, which has an anti-inflammatory effect. Recent research indicates a potential gut-lung axis, as small amounts of SCFAs are present in the lungs. The studies have also shown that SCFAs assist in creating macrophage and dendritic cell progenitors in the bone marrow. Additionally, SCFAs protect against airway inflammation and respiratory tract infections by enhancing the function of T cells [5].
Younger people may experience less severe symptoms and less risk of developing cytokine storms due to their less inflammatory response toward the coronavirus. On the other hand, the elderly are more likely to have an imbalance in their gut microbiota, so the chances of having severe inflammation and the risk of developing cytokine storms will be higher. Also, beneficial strains of microbiota like Bifidobacteria and Lactobacillus and bacteria that produce SCFAs, which help maintain intestinal barrier integrity, will be altered in the elderly. Many shreds of evidence support that gut dysbiosis is important in chronic aging related diseases. Therefore, the morbidity and mortality rates of coronavirus in elderly patients over 65 with comorbidities such as NIDDM, obesity, hyperlipidemia, hypertension and cardiovascular disorders are high.
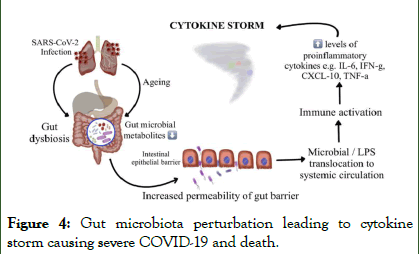
Numerous Studies reveal that immunological aging is connected with "inflammaging," a subclinical inflammatory state that relies heavily on Th1 immune responses. Children, on the other hand, exhibit more Th2 response, which leads to less production of pro-inflammatory molecules. Recent research has extensively studied and found that gut microbiota links to various chronic inflammatory diseases such as chronic respiratory diseases, inflammatory bowel disease, NIDDM, cardiovascular disease, depression and hypertension. Proving there is a strong correlation between gut microbiota disturbances and disease severity and clinical out-comes in elderly COVID-19 with chronic inflammatory illness. Multiple studies have suggested that increased cytokine and chemokine production, leading to viral hyperinflammation (cytokine storm), is mainly responsible for coronavirus mortality as illustrated in Figure 4.
Figure 4: Gut microbiota perturbation leading to cytokine storm causing severe COVID-19 and death.
Maintaining an optimized and balanced immune response is essential in preventing se-vere inflammatory reactions that could potentially be life-threatening. This can be achieved by cultivating a healthy gut microbiota. A well regulated immune response is critical for deter-mining clinical outcomes and consequences and it must be neither overly reactive nor under reactive. Consuming a nutritious diet and taking supplements can help achieve a harmonious immune response balance [6].
Research has shown that dietary carnitine, primarily found in animal protein, can negatively impact human vascular health.
Gut flora converts carnitine into Trimethylamine (TMA), which is then metabolized into Trimethylamine N-Oxide (TMAO) in the liver. Increased TMAO in the bloodstream is linked to major adverse cardiovascular events, such as stroke, myocardial infarction, congestive heart failure and mortality. In COVID-19 patients, a correlation between elevated serum TMAO and inflammation and thrombosis has been observed. Gut dysbiosis will also produce TMAO. Various molecular mechanisms, such as the Nuclear Factor Kappa (NF-kB) and the expression of Scavenger Receptors (SRs) on the surface of macrophages, will be upregulated by TMAO and lead to inflammation. TMAO can also induce the expression of pro-inflammatory cytokines such as Tumor Necrosis Factor-Alpha (TNF-α) and interleukin 1ß (IL-1ß), which increase the inflammatory response. Moreover, TMAO will reduce the expression of anti-inflammatory cytokines such as interleukin-10 (IL-10). TMAO can also enhance platelet aggregation and adhesion to collagen, which may increase the risk of thrombosis. Re-cent studies have shown that high TMAO levels may lead to Coronavirus severity.
Previous studies revealed that those who adhere to a vegan or vegetarian diet tend to have decreased levels of TMAO. Instead, consuming red meat, processed meat, egg yolks, fish and full-fat dairy products results in elevated TMAO levels.
The microorganisms that reside in our Gastrointestinal (GI) tract, from the mouth to the anus, are an essential part of our overall health. Our well-being is maintained by the gut, which is connected to various organs in our body through the gut-organ axis. Moreover, the Gut-Brain Axis (GBA) significantly influences our emotions and behavior. The gut-brain-immune system axis operates bi-directionally and can impact the progression of COVID-19, particularly when stress is involved. Several communication systems exist between the gut and brain, including the Autonomic Nervous System (ANS), the Enteric Nervous System (ENS), the immune system and neuroendocrine signaling systems, which can all impact the gut microbiota. As a result, having a healthy balance of gut microbiota may help alleviate stress levels during the pandemic.
In light of the Coronavirus pandemic, it's crucial to maintain a healthy mood and behavior to prevent cytokine storms. Several risk factors for cardiovascular disease can lead to dysbiosis, weakening the gut barrier and causing inflammation. Recent research has shown that this can increase the severity of Coronavirus symptoms. Furthermore, studies have shown a close association between gut microbiota, dietary lipid intake and atherosclerosis development, involving metabolic and inflammatory factors. A novel pathway has been identified that connects these components, with the production of TMAO being linked to reduced bile acid synthesis and inhibited reverse cholesterol transport, ultimately contributing to the development of atherosclerosis. Microbial dysbiosis and abnormal metabolite production have been associated with exacerbation of acute heart failure which can worsen the prognosis of COVID-19 patients who already suffer from both atherosclerosis and heart failure (gut-heart axis) [7].
Numerous health benefits have been associated with healthy microbial metabolites, such as anti-inflammatory, antioxidant, ant lipid, ant proliferative, anti-obesity, antihypertensive and immunomodulatory. Recent research has shown that the gut microbiota can adapt rapidly following a change in diet, whether PBD or omnivorous, with noticeable alteration appearing in three days. This information suggests that even those with unhealthy eating habits can improve their microbiota through dietary changes, which is especially relevant for new COVID-19 patients in acute settings. A shift in gut microbiota composition occurs when transitioning from PBD to an omnivorous diet, with increased bile acid-metabolizing species, which can induce an inflammatory process. On the other hand, PBD effectively combats inflammation, as it is shown in reducing chronic inflammation markers such as Fibrinogen, IL-6 and CRP. Interestingly, individuals who primarily follow PBD do not experience increased TMAO levels when occasionally consuming animal-based foods. This is postulated due to the microbiota environment established over time.
Many experts suggest that the current COVID-19 pandemic presents a rare chance to as-sess how nutritional interventions may help fight infectious diseases. With this in mind, conducting tests during the pandemic can yield valuable information. Our studies have re-vealed a significant link between consuming foods that include fresh, nutrient-rich foods like vegetables, legumes, whole grains, healthy fats (seeds, avocado and a moderate amount of oily fish) and fruits and limiting one's intake of sugary products, high-calorie empty nutrients and high salt foods, leading to a decrease in COVID-19 severity and mortality [8].
Mechanism of inflammation and endothelial dysfunction in Coronavirus: The role of chronic inflammation in developing vascular lesions cannot be overstated. This process causes endothelial dysfunction and triggers several other processes that contribute to the worsening of atherosclerosis. These processes include platelet aggregation, leucocyte adhesion, cytokine production and increased endothelial permeability. Unfortunately, atherosclerosis is often associated with acute coronary events and COVID-19 can exacerbate this situation by inducing a severe inflammatory state that may trigger similar events. It's important to note that coronary artery disease resulting from atherosclerosis, as well as heart failure, hypertension and atrial fibrillation, are all considered comorbidities for COVID-19 and they are also caused by chronic inflammation. Patients with heart conditions who contract coronavirus are at an increased risk of developing arrhythmia, acute coronary syndrome and acute heart failure, which can lead to higher mortality rates.
Eating unhealthy foods such as sugary drinks, snacks, cakes, pastries, sweets, added salt, saturated fat, trans fat, cholesterol, dairy products, processed meat, red meats, poultry and eggs can contribute to chronic inflammation. Coronavirus is classified as an acute in-flammatory disorder and it can increase inflammatory markers such as ferritin, procalcitonin, LDH, DDimer and acute phase response proteins. This virus can also trigger a cytokine storm, a severe inflammatory reaction that can be fatal. Coronavirus patients with chronic inflammation are at risk for severe inflammation regardless of their comorbidities. In that case, their body will have to work extra hard to combat the inflammation and its complications. Their chances of experiencing a cytokine storm and facing a higher mortality risk are understandably higher. Conversely, eating foods that increase Dietary Inflammatory Index (DII) is recommended to combat the inflammatory response in our coronavirus patients (Table 1).
| Foods that reduce DII | Foods that increase DII |
| Red meat (steak and hamburgers) | Plant-based proteins (beans, lentils, chickpeas, edamame, hemp seeds, tofu, tempeh and nuts) |
| Animal products (including eggs and dairy products) | Whole grains (oatmeal, buckwheat, quinoa, pigmented rice) |
| Processed meat | Starchy vegetables (sweet potatoes and beets) |
| Commercial baked goods | Seeds (flaxseeds and chia seeds) |
| White flour (bread and noodles), white rice | Green leafy vegetables (raw) |
| Deep-fried foods | Colorful vegetables (raw) |
| Sugary products | Fruits (berries, apples, grapes oranges, peaches, figs, bananas and kiwi) |
| Products with trans-fats | Spices and herbs (turmeric, ginger, cumin, peppermint, cinnamon, chili, parsley, bay leaf and basil) |
| Saturated fats (especially animal fats) | |
| Cholesterol (red meats, processed meats, eggs, fried foods and dairy products) |
Table 1: List of foods that reduce and increase DII.
Spices and herbs (turmeric, ginger, cumin, peppermint, cinnamon, chili, parsley, bay leaf and basil)
Rich polyphenols are found in vegetables and fruits and can inhibit the binding of Coronavirus spike protein to the ACE2 receptor. Thus, viral entry into host cells can be prevented and viral RNA replication and protein processing can be suppressed. Consuming red meat, refined sugar, high cholesterol, saturated and trans fats foods will promote inflammation and can expedite the binding of coronavirus to host cells.
Adopting a healthy lifestyle for an extended period can significantly improve chronic dis-ease conditions. Therefore, an individual with multiple comorbidities who embraces a healthy PBD and lifestyle may observe a normalization of most of their chronic inflammatory markers. These can decrease the risk of Coronavirus severity and mortality. Is PBD intervention a viable option for individuals with chronic comorbidities who contract COVID-19 in the acute setting? While research has indicated that PBD intervention can effectively reduce acute arthritic pain our experience with COVID-19 patients has demonstrated the same efficacy. Even though inflammatory markers may not improve, patients reported symptom relief. Thus, our study supports this hypothesis [9].
Role of oxidative stress in Coronavirus: One mechanism through which the Coronavirus causes imbalances within the body is by generating Reactive Oxygen Species (ROS) and diminishing the body's capacity to produce an tioxidants that can combat the virus. Automatically, this will induce redox stress, decreasing the body's ability to fight off the virus and increasing inflammation and cell damage. Ultimate-ly, this will damage tissues and organs in the body. A diagram illustrating this process can be found in Figure 5.
Figure 5: Redox imbalance in Coronavirus infections.
Research has shown that consuming meat products, refined sugars and fats can increase ROS levels, resulting in inflammation. However, studies indicate that incorporating PBD can potentially reduce inflammation and oxidative stress, which play a significant role in corona-virus infection. Exploring dietary changes for COVID-19 patients may be prudent as the current omnivorous or similar diets can increase oxidative stress and inflammation. Adopting PBD can help manage chronic inflammatory conditions and enhance the likelihood of surviving the COVID-19 pandemic [10].
The link between mitochondria health and COVID-19 severity and mortality: As we grow older, the powerhouses of our cells, known as mitochondria, undergo changes that cause a decline in their function. This decline is caused by ROS-inducing accumulation of oxidative damage and mutations. As a result, the volume, integrity and functionality of mitochondrial DNA (mtDNA) decrease. Moreover, the mitochondria of older adults are characterized by significant increases in ROS and decreased antioxidant defense, which lead to impaired functions. These include decreased ATP production, lowered oxidative capacity and reduced oxidative phosphorylation. Additionally, with aging, mitochondrial biogenesis will decline. This is due to inhibition of mitophagy and alterations in mitochondrial dynamics (fission and fusion). An autophagy process that eliminates defective mitochondria will also deteriorate in aging.
Acute and chronic inflammatory diseases are characterized by an excessive generation of ROS. This may cause damage to mtDNA, mitochondrial proteins and lipids. This, in turn, negatively affects normal mitochondrial function and dynamics. Inflammation is generated by various mitochondrial products called Damage-Associated Molecular Patterns (DAMPs) and is released into the cytosol or extracellular environment. Protective measures are in place to prevent mitochondria from triggering harmful inflammatory responses, such as disposing of damaged mitochondria through autophagy. However, if these mechanisms are overwhelmed or not functioning correctly, inflammatory reactions instigated by mitochondria can become problematic and contribute to developing disorders associated with autoimmunity. Further-more, inefficient inflammatory pathways can exacerbate infectious diseases and impede healing.
Atherosclerosis occurs due to the dysfunction of endothelial cells and the infiltration of lipids. Mitochondrial dysfunction can negatively impact various cells within the arterial wall, including endothelial cells, smooth muscle cells, macrophages and lymphocytes, leading to heightened ROS levels. This can cause chronic inflammation, oxidative stress and intracellular lipid deposition. Moreover, mitochondrial dysfunction plays a significant role in chronic inflammatory diseases like hypertension, obesity and asthma.
As we learn more about COVID-19, it becomes increasingly clear that certain factors may contribute to its severity and mortality. These include age, age related conditions and underlying disorders like CVD, metabolic syndrome (including NIDDM), obesity and hypertension. In coronavirus disease development, a potential role for mitochondria has been discovered. Mitochondria and its mtDAMPs control the immune system and impact coronavirus infection. It is suggested that mitochondria hijacked by the coronavirus could significantly affect COVID-19 pathogenesis potentially causing massive inflammation and damage to multiple organs. A new study in the journal nature sheds light on why some people with COVID-19 develop these severe symptoms, revealing that the virus may be able to infect and cause fatalities in vital immune cells within the bloodstream and lungs. As we continue to investigate this virus, it has been proven that mitochondrial dysfunction significantly eliminates these immune cells.
Studies have proposed that people living in "blue zones" lead long and healthy lives by adhering to healthy habits such as exercising regularly, eating a balanced diet, mainly being PBD, abstaining from harmful substances, managing stress effectively, having strong social support and getting enough rest. These lifestyle choices contribute to maintaining healthy mitochondria. Mitochondrial function can be improved by consuming PBD foods, specific natural products, caloric restriction, intermittent fasting and exercise. Our elderly coronavirus cardiology patients have been living a blue zone lifestyle for many years, leading us to hypothesize that this has resulted in less severe symptoms and zero mortality due to their healthy mitochondria [11].
Potential benefits of telomere manipulation in Coronavirus treatment: As the Centers for Disease Control and Prevention (CDC) reported, the most sign:ificant factor in determining poor outcomes and severe illness in individuals with COVID-19 is aging. Data from the National Vital Statistics System (NVSS) at the CDC reveals that people aged 50-64 with COVID-19 are 25 times more likely to die than those under 30 years old. For individuals aged 65-74, the risk of death increases to 60 times, while for those over 85, it jumps to 340 times. This data includes all deaths in America from February 2020 to July 1, 2022, regardless of vaccination status.
Short telomeres are affiliated with a higher probability of allcause mortality and dis-ease-specific mortality in the general population. Studies suggest that COVID-19 severity in older individuals may be influenced by the same molecular pathways that cause aging. One of these pathways involves gradual telomeres shortening. Telomeres are protective structures at the ends of chromosomes. When telomeres become excessively short, they can hinder tissue regeneration and disrupt tissue homeostasis, leading to disease. Since the Coronavirus infects various cell types, it triggers cell turnover and regeneration to support homeostasis. Research has shown that people with shorter telomeres are at an increased risk of experiencing severe Coronavirus symptoms. The risk of developing severe Coronavirus pathologies has been associated with individuals with higher percentiles of short telomeres and lower percentiles of telomere length. Myeloid and lymphoid cells contribute to innate and adaptive immunity, which is essential in defending against Coronavirus. To resist the infection, the production of myeloid cells is rapidly activated when the virus enters the body. The length of telomeres will shorten with age; this will affect the production of T and B cells, which are crucial to clearing the virus. Understandably, older people will have a higher risk of a T-cell shortfall when contracting Coronavirus compared to younger people. People with inherently short T-cell telomeres will experience poor adaptive immune response caused by a Tcell deficit, which might con-tribute to the severity of COVID-19. These individuals might also generate inadequate Tcell response to anti-SARS-Cov-2 vaccination, which is vital to know. Furthermore, ACE2 (Angiotensin Converting Enzyme 2), the receptor for SARS-CoV-2, is upregulated by shortened telomeres. So, telomere shortening in elderly individuals increases their susceptibility to corona-virus infection and increases their risk for Coronavirus severity and mortality.
Chronic inflammation can cause the shortening of telomeres, altering the genes related to telomeres and decreasing telomerase enzymes, which control the release of cytokines that cause inflammation. All of these mechanisms will cause severe COVID-19 disease and mortality. There is a two-way relationship between telomere shortening and inflammation; telomere attrition and dysfunction can cause low-grade inflammation. On the other hand, inflammation can speed up telomere wear and telomere dysfunction.
Chronic inflammation and oxidative stress can accelerate telomere shortening. However, consuming healthy PBD, which is full of anti-inflammatory and antioxidant properties, counteracts this process. Observational studies have indicated that adopting a healthy PBD, consuming seeds and their derivatives and incorporating carotenoids will promote telomere lengthening. This can lead to improved overall health and longevity.
Elizabeth Blackburn, a Nobel Prize winner, discovered that switching to a vegan diet can change over 500 genes in just three months. This diet can activate genes that help prevent diseases and deactivate genes that cause chronic inflammatory diseases. There are various ways to strengthen our telomeres, including exercising regularly, avoiding smoking and consuming a diet rich in plant based foods that protect telomeres. Dean Ornish and Elizabeth Blackburn conducted a study demonstrating how PBD can increase telomerase activity, the enzyme responsible for maintaining long telomeres. The ability to lengthen telomeres is crucial for longevity. While we cannot reverse chronological age, we can reverse biological age, which can help us reverse chronic illnesses in our patients and protect them from severe morbidity and mortality from coronavirus. Additionally, reducing our patients' biological age by one or two decades will automatically decrease their risk of developing severe coronavirus. We hypothesized that one of the mechanisms implies that the elderly coronavirus patients in our study have milder symptoms and experience no mortality, which is linked to their telomere superiority [12].
Caloric restriction is emerging as an essential factor in the fight against inflammation: Reducing caloric intake, commonly known as Caloric Restriction or CR, has been shown to have consistent anti-aging effects across various organisms. Age-related diseases, including chronic inflammatory disorders such as stroke, NIDDM, cardiovascular disease, hypertension and cancer, have been shown to improve with the practice of CR. CR can reduce oxidative stress and inflammation while boosting the production and activity of antioxidant enzymes and antiinflammatory mediators. Studies have also revealed that CR can improve overall health and well-being, reduce ROS and inflammation, enhance cellular protection, optimize energy metabolism, improve insulin sensitivity and glucose regulation, induce functional changes in the neuroendocrine systems and even shape the gut microbiota.
DNA and RNA viruses, including coronavirus, use the mammalian Target of Rapamycin (mTOR) as their signaling system to replicate and persist in host cells. CR has been found to inhibit the mTOR pathway, similar to the effect of Rapamycin in laboratory research. One of the mechanisms CR benefits in Coronavirus is mTOR inhibition and autophagy promotion. More-over, CR could help fight the virus by interrupting the viral cycle (protein synthesis).
In our modern society, unhealthy habits like consuming excessive calories and living a sedentary lifestyle are significant determinants of health issues and inflammatory disorders. The overconsumption of food, especially unhealthy food, can pose big problems. Therefore, COVID-19 patients who consume excessive calories with poor nutrients will struggle to fight inflammation, especially if their bodies are already inflamed. We hypothesized that the whole food PBD emphasizing CR may have contributed to the mild illness and zero mortality observed in our COVID-19 elderly patients with multiple comorbidities study [13].
Supplements their significant role in managing COVID-19
In the preliminary phase of our research, we did not come across any academic literature demonstrating the role of dietary supplements in mitigating the frequency, severity and mortality of Coronavirus infection. Therefore, the literature we used to determine the types of vitamins, minerals and nutraceuticals in our study was taken from the literature we used in previous studies, where we combatted chronic inflammatory diseases with PBD and dietary supplements. Those dietary supplements have been known to increase NO levels, reduce inflammation, serve as immunomodulatory, decrease the likelihood of cytokine storms, fight oxidative stress and exhibit antiviral properties. We also studied extensively literature about dietary supplements that have shown their benefits in previous viral pandemics.
Most adults consume a poor-quality diet and lack essential nutrients such as magnesium, calcium, potassium, iron, vitamins A, C, D, E, fiber and choline. Therefore, we provide our patients with multivitamins based on the literature and blood levels. It is worth noting that all of our cardiology patients who follow PBD have been advised to take B12, dietary multivitamins and supplements with anti-oxidant, anti-inflammatory, endothelialsupporting and other properties relevant to cardiovascular health [14].
Vitamin C: Due to its anti-infective properties and safety, many experts have proposed vitamin C as a potential treatment for Coronavirus. Studies have shown the severity and duration of colds can be reduced by taking vitamin C. numerous studies have revealed that vitamin C may support cellular health and defense against Coronavirus infection. This is believed because vitamin C has anti-oxidative stress and anti-inflammatory properties. In severe corona virus cases, high doses of vitamin C help fight oxidative stress and relieve the severity of cytokine storms. A high dose of intravenous vitamin C shortens patients' time in the ICU and if combined with corticosteroids and thiamin, it also reduces mortality.
In treating patients who require mechanical ventilation caused by an acute inflammatory lung injury, vitamin C has positive effects due to its oxidative stress properties. A study from China suggested that high-dose intravenous vitamin C can effectively treat Coronavirus patients. Those patients who received intravenous bolus vitamin C had their oxygenation improved and no mortality was observed.
In recent meta-analyses of randomized controlled trials, vitamin C may improve mortality rates in patients with severe Coronavirus infections. Nonetheless, the current guidelines for Coronavirus management do not yet recommend using vitamin C [15].
Vitamin D: In our previous experience with cardiology patients who strictly adhered to a plant-based diet, we found that most of them were deficient in vitamin D. Therefore, we recommend that our patients take vitamin D supplements and adjust the dosage based on their blood vitamin D levels. We have discovered that vitamin D plays a crucial role in chronic inflammatory diseases, including coronary heart disease and it may also play a role in combating COVID-19, in which inflammation plays a significant role.
T regulatory lymphocytes (Tregs) are essential in fighting against uncontrolled inflammation and viral infections. However, many COVID-19 patients have low Tregs levels. One way to increase Tregs levels is through supplementation with vitamin D. Decreased vitamin D has been linked to increased inflammatory cytokines, which significantly increase the risk of infection in the upper respiratory tract, including viral and pneumonia. The recent paper has acknowledged the role of vitamin D in reducing the risk of COVID-19. The proposed mechanism is the induction of cathelicidin and defensins, which decreases the risk of viral and bacterial infections and diseases, including pneumonia. Additionally, vitamin D may reduce the binding of the virus to the ACE2 receptor, which could potentially lessen the risk of cytokine storms in coronavirus infection.
The likelihood of thrombotic events, commonly observed in coronavirus patients, has been associated with a vitamin D deficiency. During the pandemic, it was observed that many coronavirus patients developed severe diseases or died due to vitamin D deficiency. A recent meta-analysis has suggested that vitamin D supplementation could positively impact the incidence, severity and mortality of SARS-CoV-2 illness, especially in patients with vitamin D deficiency.
Vitamin B3, precursor of NAD+: There are three primary types of vitamin B3, i.e., Nicotinic Acid (NA), Nicotinamide Riboside (NR) and Nicotinamide (NAM). These vitamins are not only helpful in preventing pellagra but may also prevent some of the physiological changes that occur with age-related diseases and promote healthy aging, particularly NR. It has been suggested that increasing NAD+ levels might enhance the body's ability to fight off viruses and reduce inflammation. NA, NR and NAM play essential roles as precursors of NAD+ and provide the production of NAD+ through different metabolic pathways [16].
Studies indicate that different types of B3 vitamins will support NAD+ levels differently. To increase NAD+ concentrations, one can give NMN, which is derived from NAM and in the body will be converted into NAD+. NMN only requires one enzymatic step to be transformed into NAD+ and is currently the most effective method to raise NAD+ levels. Research on NAD+ in vascular aging and chronic inflammatory diseases like coronary artery disease has been promising. NAD+ has been shown to reduce chronic inflammation, induce reactivate autophagy and assist mitochondrial biogenesis. These findings suggest that supplementing with precursor NAD+ may be a useful therapeutic approach for treating these conditions as we have done for our elderly cardiology patients long before the coronavirus pandemic. Further, more sophisticated research is required before recommending precursor NAD+ to reduce the morbidity and mortality of Coronavirus patients.
Zinc: Oral Zinc (Zn) supplementation can reduce the 30-day death rate, shorten the duration of symptoms and decrease the ICU admission rate, as shown in a recent randomized, double blind controlled trial. Trace element zinc is crucial in stimulating innate and acquired immunity. A recent metaanalysis has found that zinc supplementation can reduce coronavirus mortality in hospitals. Due to the scientific evidence of zinc's role in coronavirus patients, it should be considered an adjunct therapy.
Copper: Both Copper (Cu) and zinc play an essential role in the production of an important antioxidant enzyme known as Superoxide Dismutase (SOD). This enzyme aids in combating free radicals and decreasing oxidative stress. Maintaining the appropriate ratio between the two is essential to ensure the optimal functioning of this enzyme. It is important to know that zinc can lead to copper deficiency. Therefore, seeking guidance from a qualified healthcare professional is crucial to prevent adverse effects. Cu plays a critical role in assisting the functions of macrophages, neutrophils and immune cells such as B cells, T helper cells and Natural Killer (NK) cells. These blood cells kill infectious microbes, produce specific antibodies against pathogens and mediate cell-mediated immunity. In humans with Cu deficiency, there is an in-creased risk for infections due to these blood cells' decreased number and function.
Additionally, Cu can kill viral infections like poliovirus, Human Immunodeficiency Virus type 1 (HIV-1), single or doublestranded DNA or RNA and other enveloped or non-enveloped viruses. Moreover, Cu has a potent contact-killing capacity against several viruses, including SARS-CoV-2. We always combine Zn and Cu in our center since Zn can lead to Cu deficiency.
Selenium: Several studies have suggested that lacking selenium may negatively affect viral disorders. The correlation between selenium and Coronavirus disease severity research has yielded mixed results. According to the report, a shortage of selenium is linked to a higher risk of chronic diseases with inflammatory pathogenesis. In viral disorders, supplementing with selenium has shown promising outcomes. This is assumed due to selenium's immune-boosting, anti-inflammatory and antithrombotic effects. Most of our cardiology patients have been consuming selenium before contracting Coronavirus.
Coenzyme Q10 (CoQ10): CoQ10 benefits cardiovascular health by helping reduce total cholesterol, improving endothelial function and fighting inflammation and oxidative stress. This also makes it a suitable option for treating COVID-19. A recent meta-analysis found that CoQ10 supplements taken for 10 weeks may lower Malondialdehyde (MDA), IL-6 and TNF-α levels, which are all involved in COVID-19 inflammation.
In the course of the resurgence of the Coronavirus pandemic in China in 2023, there has been a growing demand for Ubiquinolthe active form of CoQ10. Supplementing with Ubiq-uinol can significantly increase the level of CoQ10 in whole blood, platelets and plasma. CoQ10 can also accelerate the regeneration of mitochondrial function. Recent research has shown that patients recovered from Coronavirus have reduced levels of platelet mitochondrial function and decreased endogenous CoQ10. Mitochondria are the energy powerhouses of our cells and are vital for cellular metabolism and immune responses. Further research has proposed that mitochondria have a role in antiviral defense. We used CoQ10 on our cardiology patients, which may also benefit Coronavirus patients [17].
Astaxanthin: Studies have shown that astaxanthin significantly reduces oxidative stress biomarkers, such as blood MDA levels. This effect is particularly notable in NIDDM patients, especially those who are overweight, where astaxanthin has been found to improve superoxide dismutase activity and reduce serum isoprostane, which has an antioxidant effect and can neutralize free radicals.
Natural astaxanthin can potentially alleviate cytokine release syndrome by regulating in-flammatory cytokines. The mechanism is by inhibiting the activities of key players such as JAK/STAT-3, NF-kB, NLRP3, while regulating the expression of proinflammatory factors such as IL-6, IL-8, TNF-α and IL-1ß. Additionally, natural astaxanthin can prevent oxidative dam-age. Given these benefits, it is reasonable to consider supplementation with astaxanthin since it has a potential therapeutic effect against inflammation and cytokine storms in coronavirus patients.
Quercetin: Quercetin may reduce the likelihood of Coronavirus patients being admitted to ICU, as has been shown in recent systematic reviews and meta-analyses. It also can lower hospitalization rates and potentially decrease mortality. Quercetin, as an antioxidant, has also been known to possess antiviral and anti-inflammatory properties. According to studies, quercetin has been found to interfere with 85% of Coronavirus proteins in human cells. A study recently highlighted quercetin's capability to block ACE2 receptors, thereby interfering with viral replication. Moreover, protease enzymes that play a crucial role in virus replication may be inhibited by Quercetin.
Flavonoid quercetin in PBD has been found to block the active site of 6LU7, the major pro-tease in Coronavirus. This will inhibit virus replication. In addition to its an-ti-inflammatory and antioxidant effects, Quercetin exhibits a potent ironchelating property, which helps decrease the severity of Coronavirus symptoms. Due to these properties, we believe Quercetin can be a valuable therapeutic option for treating COVID-19 [18].
Curcumin: Curcumin is a natural polyphenolic compound with various benefits, such as an-ti-inflammatory, antiviral cytoprotective, anticoagulant and antiplatelet properties. It has been proven to help reduce the progression of several inflammatory diseases. These effects have made Curcumin a potential treatment option for Coronavirus patients. The patho-physiology of COVID-19 involves severe inflammatory reactions, coagulopathy and the development of cytokine storms. The benefits of Curcumin can be due to its anti-inflammatory effects, such as inhibiting inflammasome formation. By binding to the primary protease (Mpro) enzyme of Coronavirus, which is necessary for viral replication, Curcumin has been found to have antiviral effects. Additionally, Curcumin can effectively block viral attachment to entry into human cells. According to modeling studies, ACE2 receptor and spike proteins are both inhibited by Curcumin, thus preventing virus-receptor interaction. In a randomized trial, it was suggested that Curcumin could speed up the recovery of acute inflammatory immune response.
In Coronavirus patients who received nano-curcumin, the mRNA expression of interleu-kin-6 and interleukin-1ß was significantly decreased, which may reduce the systemic inflammatory reaction. Moreover, further trials showed a significant reduction in gene expression, the number of Th17 cells and serum levels of Th17- mediated cytokines upon administering cur-cumin. These mechanisms may benefit Coronavirus patients. Systematic reviews and meta-analyses of randomized trials recently concluded that oral administration of Curcumin as a supplement in Coronavirus patients could significantly decrease their death risk.
Taurine: Various studies suggest Taurine can act as an antioxidant, anti-inflammatory and antiviral substance. Taurine may also help regulate vascular function. Its potential effects are wide-ranging, from stopping viral invasion through the AT1Rmediated Coronavirus/ACE2 endocytosis pathway to reducing vascular injury and inflammation by affecting both inflammatory and coagulation pathways. Like other infections, COVID-19 decreases Taurine levels, which limits its protective properties under normal circumstances. It is hypothesized that early Taurine administration during COVID-19 onset can halt cytokine storms, reducing morbidity and mortality. Taurine seems to be a promising, supplementary option for Coronavirus patients [19].
Healthy lifestyles their significant role in managing the COVID-19 pandemic
As we demonstrated, the significance of PBD and supplementations in managing corona-virus patients has been emphasized. In addition to following a balanced diet, everyone must adopt certain lifestyle practices to mitigate chronic inflammatory conditions and prevent severe Coronavirus and its associated mortality. These practices include maintaining a healthy weight, engaging in regular physical activity, reducing stress, abstaining from harmful substances such as smoking and alcohol, ensuring adequate sleep and fostering positive personal relationships.
To enhance the immune system, consuming 2-3 cups of coffee daily and cabbage and fermented vegetables in one's diet is recommended. Cabbage is rich in sulforaphane, a natural and potent Nrf2 activator. Fermented vegetables are abundant in lactobacilli, another potent Nrf2 activator with antioxidant properties, helping alleviate the severity of Coronavirus infections.
During the COVID-19 pandemic, we recommended that our patients receive sun exposure. Research has demonstrated that sunlight exposure is associated with decreased mortality rates for COVID-19 patients, independent of its role in increasing vitamin D levels. It is believed that ultraviolet A and B radiation may promote the release of NO from the skin, which can benefit cardiovascular health and reduce the risk of Coronavirus infection [20].
Conclusion
PBD has been associated with reduced COVID-19 incidence, severity and mortality rates over time, as demonstrated by various studies. However, in early 2024, some experts in the field, including Rayman M, Stewart G, Mellor D and McCoway K, strongly reacted to a recent study published in BMJ Nutrition, Prevention and Health by Acosta-Navarro, et al. Their study focused on the relationship between different types of diets and COVID-19 infection. The experts specifically highlighted the deficiency of essential nutrients, such as vitamins B12 and D and minerals like iodine, iron, zinc, selenium and calcium, in PBD interventions, which can be detrimental, particularly for pregnant individuals. The experts also drew attention to the ambiguous definition of PBD in the study, which did not consider factors such as the quality, quantity and food preparation methods, as well as the loose definition of PBD encompassing ovo and pesco vegetarians. Since most of those studies used questionnaires, further research with a clear definition of PBD and adequate supplementation is needed to provide valuable insights and shed additional light on the subject, per the expert commentary.
In the context of those criticisms, our study has given considerable importance to the ex-pert opinions regarding the inclusion of micronutrients in our Coronavirus participant's dietary supplements, including vitamin C, vitamin D, vitamin B3/NAD+, zinc, copper, selenium and natural anti-inflammatory products such as astaxanthin, curcumin, quercetin, as well as CoQ10, taurine and multivitamins (containing various small doses of minerals and vitamins as recommended for daily RDA). To the best of our knowledge, as of the writing of this paper, no previous PBD studies on COVID-19 have included the use of supplements. Our study aims not only to ensure the adequacy of supplementation but also to validate our hypothesis that dietary supplements can enhance the anti-inflammatory, immune regulatory and antiviral properties of PBD in combating Coronavirus. However, in recent years, experts (not PBD experts) have highlighted the importance of using supplements in managing the virus.
The critical distinction between our research and others is that we accounted carefully for variations in food quality, quantity and preparation methods. Additionally, we closely monitored our participants' dietary intake throughout their illness. These factors that distinguish our study from others in the field are paramount. When considering these elements, evaluating the disparities between our research outcomes and those of other studies is crucial, particularly the lack of disease progression, hospitalization and mortality among our participants. Our study stands out due to these unique characteristics, which merit special attention.
Our research and theories have saved the lives of COVID-19 patients and improved and reversed their chronic diseases, enhancing their quality of life and extending their lifespan. Furthermore, our findings may offer protection against future pandemics, i.e., disease X, as the World Health Organization (WHO) has predicted.
Reviewing the historical record from the start of the 20th century, it is evident that a diet emphasizing PBD and adopting a healthier lifestyle has safeguarded numerous individuals from various pandemics. Furthermore, our extensive knowledge of supplementation will enrich our understanding of how to combat COVID-19 and may also motivate us to prepare for future pandemics. Numerous studies have demonstrated the importance of PBD in managing COVID-19 and our research has contributed significant evidence to support this claim. Despite this, the medical community remains cautious and skeptical about the use of PBD in treating the virus. Till the writing of this article, the World Health Organization has not endorsed PBD or supplementation specifically in their guidelines for managing Coronavirus. We hope that more research will be conducted to fully understand PBD and supplementation benefits in treating viral illnesses, leading to greater acceptance and adoption by the wide medical community.
Author Contributions
Conceptualization: D.M.; Writing-original draft: D.M.; Writingreview and editing: D.M., A.M.H., I.N.E.L., M.K.S. and H.U. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the National Institute of Health.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wang P, Song M, Eliassen AH, Wang M, Fung TT, Clinton SK, et al. Optimal dietary patterns for prevention of chronic disease. Nat Med. 2023;29(3):719-728.
- Pena-Jorquera H, Cid-Jofre V, Landaeta-Diaz L. Plant-based nutrition: exploring health benefits for atherosclerosis, chronic diseases and metabolic syndrome-a comprehensive review. Nutrients. 2023;15:3244.
- Kim H, Rebholz CM, Hedge S. Plant-based diets pescatarian diets and COVID-19 severity: A population-based case-control study in six countries. BMJ Nut Prevent Health. 2021;4:e000272.
- Oboza P, Ogarek N, Olszanecka-Glinianowicz. The main causes of death in patients with COVID-19. Eur Rev Med Pharmacol Sci. 2023;27(5):2165-2172.
- Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: A systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. 2021;21:855.
- Gupta SC, Prasad S, Aggarwal BB. Anti-inflammatory nutraceuticals and chronic diseases. Adv Exper Med Biol. 2016;928.
- Chojnacka K, Skrzypczak D, Izydorczyk G. Antiviral properties of polyphenols from plants. Foods. 2021;10:2277.
- Alesci A, Aragona M, Cicero N. Can nutraceuticals assist treatment and improve covid-19 symptoms? Nat Product Res. 2021.
- Alam S, Sarker Md MR, Afrin S. Traditional herbal medicines, bioactive metabolites and plant products against covid-19: Update on clinical trials and mechanism of actions. Front Pharmacol. 2021;12:671498.
- Loscalzo J, Welch G. Nitric Oxide and its role in cardiovascular system. Prog Cardiovasc Dis. 1995;38(2):87-104.
- Torregrossa AC, Aranke M, Bryan NS. Nitric oxide and geriatrics: Implications in diagnostics and treatment of the elderly. J Geriatr Cardiol. 2011;8(4):230-242.
- Nikolaidis A, Kramer R, Ostojic S. Nitric oxide: The missing factor in COVID-19 severity? Med Sci (Basel). 2022;10(1):3.
- Flaxman S, Whittaker C, Semenova E. Assessment of COVID-19 as the underlying cause of death among children and young people aged 0 to 19 Years in the US. 2023;6:e2253590.
- Babateen A, Shannon O, Mathers JC. Validity and reliability of test strips for the measurement of salivary nitrite concentration with and without the use of mouthwash in healthy adults. Nitric Oxide. 2019;91(5).
- Kobayashi J, Ohtake K, Uchida H. No-rich diet for lifestyle-related diseases. Nutrients. 2015;7(6):4911-4937.
- Fang W, Jiang J, Su L. The role of NO in COVID-19 and potential therapeutic strategies. Free Rad Biol Med. 2021;163:153-162.
- Ritz T, Trueba AF, Vogel PD. Exhaled nitric oxide and vascular endothelial growth factor as predictors of cold symptoms after stress. Biol Psychol. 2018;132:116-124.
- Alqahtani JS, Aldhahir AM, Al Ghamdi SS. Inhaled nitric oxide for clinical management of covid-19: A systematic review and meta-analysis. Int J Environ Public Health. 2022;19;12803.
- Mir JM, Maurya RC. Nitric oxide as a therapeutic option for COVID-19 treatment: A concise perspective. New J Chem. 2021;45:1774.
- Wiertsema SP, van Bergenhenegouwen J, Garssen J. The interplay between the gut microbiome and the immune system in the context of infectious diseases throughout life and the role of nutrition in optimizing treatment strategies. Nutrients. 2021;13(3):886.
Citation: Mulijono D, Hutapea AM, Lister INE, Sudaryo MK, Umniyati H (2025) The Mechanisms of How Plant-Based Diets and Dietary Supplements Reduce COVID-19 Severity and Achieve Zero Mortality in High-Risk Elderly Patients. J Gerontol Geriatr Res. 14:772.
Copyright: © 2025 Mulijono D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.