Indexed In
- Open J Gate
- Academic Keys
- JournalTOCs
- ResearchBible
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2025) Volume 13, Issue 2
Different Effects of Functional Food and Music Aerobic Exercise on Complete Blood Counts, Blood Biochemistry and Frailty Scores of Older Adults
Kuender D. Yang1*, Mu-Hsuan Pan2, Shu-Hui Yeh2, Chia-Hua Lee3, Ming-Tsung Lee4, Jeng-Hwan Wang5 and Wen-Chien Sung62Department of Medical Research, Mackay Medical College, New Taipei City, Taiwan
3Department of Nursing, Suang-Lien Elderly Center, New Taipei City, Taiwan
4Department of Geriatrics and Welfare Research, National Health Research Center, Yunlin County, Taiwan
5Department of Food Beverage Management, MacKay Junior College of Medicine, Taipei, Taiwan
6Department of Food Science, National Taiwan Ocean University, Taipei, Taiwan
Received: 25-Sep-2023, Manuscript No. JASC-23-23173; Editor assigned: 28-Sep-2023, Pre QC No. JASC-23-23173 (PQ); Reviewed: 12-Oct-2023, QC No. JASC-23-23173; Revised: 08-Apr-2025, Manuscript No. JASC-23-23173 (R); Published: 15-Apr-2025, DOI: 10.35248/2329-8847.25.13.405
Abstract
This study prepared Functional Foods (FF) with softened chicken moose and milkfish without fin for older adults and compared the different effects of FF from those of Music Aerobic Exercise (MAE) on the complete blood counts, blood biochemistry, including nutrition index of albumin, and cholesterol levels, and frailty scores before and after institution of FF and MAE among residents of long-term care institutes. The FF significantly increased the high-density lipoprotein cholesterol and albumin levels. In contrast, MAE significantly increased Red Blood Cells (RBC), and decreased the rates of frailty items on fatigue feeling and low physical activity. In comparison between FF and MAE groups, we found that the FF significantly improved better on HDL-C and MCV while the MAE improved significantly better on hematopoiesis as increases in red blood cells and platelets. A combination of FF and MAE might improve better nutrition, physical function, and frailty for older adults.
Keywords
Functional food; Music aerobic exercise; Complete blood counts; Biochemistry; Frailty
Introduction
Older adults with Chewing Difficulty (CD) are prone to insufficient intake of meat and plant fibers. They are more likely to cause many health problems, such as malnutrition, frailty, and sarcopenia. Similarly, older adults with Insufficient Physical Activity (IPA) are prone to frailty, sarcopenia, and anabolic resistance to muscle metabolism. The prevalence of CD and IPA in older adults with sarcopenia has increased by over 30% and 50%, respectively [1].
Older adults with CD and/or IPA are closely correlated to frailty and linked with geriatric syndrome. There is an urgent need to promote healthy physical activity and prepare functional foods for older adults to prevent malnutrition and frailty. We have previously shown that moderate exercise such as Tai Chi Chuan, Yoga, and Music Aerobic Exercise (MAE) could enhance immune function, stress adaptation, and neural function. Tai Chi Chuan exercise for 12 weeks improved immune regulation and neuropathy Yoga exercise could improve stress adaptation and MAE could enhance immune function decrease depression, and increase brain-derived neurotrophic factor levels. We also found that CD is prevalent in nursing homes and correlated to the institution of gastric tube feeding and frailty. Here, we postulated that the FF made in softened meat and jelly fruit juice for older adults could be comparative to or different from the effects of the MAE on frailty and blood biochemistry [2].
This study aimed to compare the different effects between the Moderate Exercise of music (MAE) and Functional Food (FF) made in softened chicken meat or fish with antioxidant herbs and fresh jelly fruit juices on complete blood counts, blood biochemistry including nutrition index of albumin, and cholesterol levels, and rates of the frailty items among residents of long-term care institutes [3-5].
Materials and Methods
Study design
This quasi-experimental research was conducted in communities around the northeastern coast of Taiwan. Eighty-five older adults in eight long-term care institutes were recruited to participate in the FF group (n=36 in 2 senile centers) or MAE group (n=49 in 2 senile centers) after obtaining informed consent for the participation agreement from the institutes and residents. This comparative study was initially designed to do a parallel comparison between FF and MAE groups for 10 weeks. During the COVID-19 pandemic, the quarantine policy for group meals at long-term care facilities was changed to prohibit extramural preparation of group meals so that the study period of the FF group was cut off at 5 weeks. The MAE group performed the study as scheduled three times a week, each for 50 minutes of performance for 10 weeks. Inclusion criteria are older adults who were over 65 years old, signed the participation agreement, and moved independently. Exclusion criteria for participation are those who were bedridden, unable to move or eat softened food [6].
Preparation of functional foods
Functional foods, including softened chicken meat, softened milkfish, and jelly fruit juice for older adults with CD, were made in tongue-crushed food with a physical property tester of less than 2.0 × 104 N/m2 [16]. Choosing a technique of vacuum low-temperature cooking of the meat and fish with phytochemical-rich herbs makes meat sufficiently soft to be broken up by the tongue and gives a good taste of herbs’ fragrance. The FF included softened milkfish (Figure 1) and chicken moose with herbs containing ginseng and wolfberry, and the jelly fruit juice was made from golden and green fruits (apple, pineapple, kiwi, and strawberry) prepared by a central kitchen. The low-temperature cooking foods were put into the vacuum packaging of aluminum foil for better storage of 6 months. The two FF products fulfilled the microbiological standards for frozen foods requirement at less than 10 colonyforming units of E. coli. The FF group consumed original meals plus chicken moose and milkfish 5 packs and two bottles of fresh fruit jelly per week for 5 weeks [7].
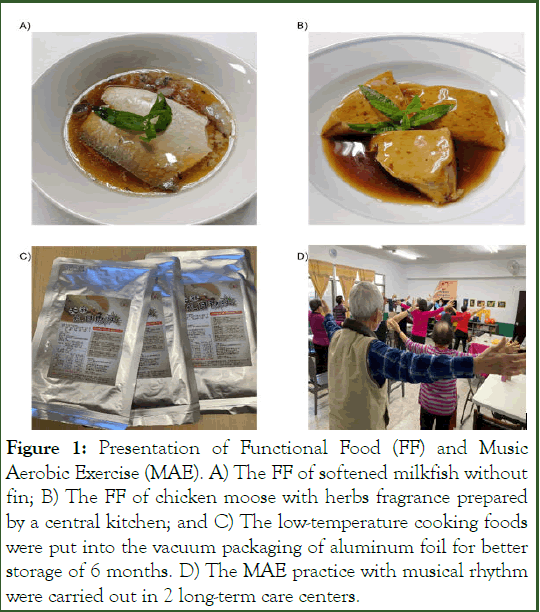
Figure 1: Presentation of Functional Food (FF) and Music Aerobic Exercise (MAE). A) The FF of softened milkfish without fin; B) The FF of chicken moose with herbs fragrance prepared by a central kitchen; and C) The low-temperature cooking foods were put into the vacuum packaging of aluminum foil for better storage of 6 months. D) The MAE practice with musical rhythm were carried out in 2 long-term care centers.
Moderate exercise of Music Aerobic Exercise (MAE)
The physical activity for older adults with IPA should be moderate exercise and harmonious balance without cardiopulmonary exacerbation. Previous studies showed that the MAE was a moderate exercise for community adults, effectively improving stress adaptation and immune regulatory function. The MAE included rhythmic exercise for 50 minutes (10 minutes of warm-up, 30 minutes of musical exercise, and 10 minutes of cool-down exercise) 3 times a week for 10 consecutive weeks. Before and after the program, the participants received tests on frailty, biochemistry, and complete blood counts [8-9].
Assessment of complete blood counts and biochemistry
Blood samples (5 ml) were subject to measurement of CBC and biochemistry. The biochemistry, including high-density lipoprotein cholesterol (HDL-C, mg/dl), low-density lipoprotein cholesterol (LDL-C, mg/dl), and albumin (gm/dl), were measured by Roche c702 (Roche Diagnostics, Indianapolis, USA). The complete blood counts including WBC (cells/ul), RBC (x106/ul), Hemoglobin (gm/dl), Hematocrit (%), MCV (pl/cell), MCH (pg/ cell), MCHC (gm/dl), Platelet (x103/ul), Neutrophil (cells/ul), Lymphocyte (cells/ul), Monocyte (cells/ul), Basophil (cells/ul) and Eosinophil (cells/ul) were measured by Sysmex XP300 (Sysmex Diagnostics, Seattle, USA) [10].
Measurement of the rate changes of the frailty items
Employing Fried’s frailty assessment scales, including body weight loss, fatigue feeling, low physical activity, decreased muscle strength, and slowed walking speed we assessed the rate changes of the frailty items before and after the FF or MAE program. The cut-off values for the frailty items were defined as 1) Weight loss: Less than 20% of peers; 2) Fatigue feeling: Tired 3 or more days a week; 3) Decreased muscle strength: Grip strength test in male (female) <26 (18) kg determined by a digital hand dynamometer (Handexer Inc., Sacramento, CA); 4) Slowly walking speed less than 0.8 m/s (6 minutes <288 m); and 5) Low physical activity: Less than 20% of peers. The rates (percentages) of the 5 frailty items were assessed before and after the FF and MAE programs [11].
Data analyses and statistics
This study recruited older adults in eight long-term care facilities, where the institutes and residents were willing to participate in moderate exercise or function food study. The sample size was estimated based on the effect size on the changes in cholesterol levels or blood counts at 0.2 before and after MAE or FF intake, study power of 0.8, and alpha level of 0.05. The estimated number of effective samples was calculated as 40. Statistical analyses are performed using SPSS version 22 (IBM, Inc., Armonk, NY, USA). The Chi-square test was applied to compare the difference of rates (percentages), paired t-test was applied to test the normally distributed changes before and after the FF or MAE program, and the Generalized Estimating Equation (GEE) statistics were used to compare the differences between the effects of FF and MAE [12].
Results
Demographic data of the FF and MAE groups
This study was designed to do a parallel 10-week comparison between FF and MAE groups for the different effects on nutrition biochemistry, CBC, and frailty rates. The FF study was cut off to a 5-week study due to the change of quarantine policy in the COVID-19 periodic outbreaks. Forty-nine participants in two long-term care institutes completed the 10-week MAE study, and thirty-six participants completed the 5-week FF study. The demographic data of the two studies are shown in Table 1. More female residents participated in the MAE group, and more male residents participated in the FF group. The population studied had an average of 76 years old. Neither FF nor MAE group had a significant difference in age, weight, height, or blood pressure [13].
|
|
MAE (n=49) |
FF (n=36) |
Total (n=85) |
|
|||
|---|---|---|---|---|---|---|---|
|
Mean |
SD |
Mean |
SD |
Mean |
SD |
||
|
Gender |
|||||||
|
Male/female |
15/34 |
|
21/15 |
|
36/49 |
|
|
|
Age, year |
78.2 |
5.7 |
73.1 |
7.8 |
76 |
7.1 |
|
|
Height, cm |
157 |
8.4 |
160.1 |
8.8 |
158.3 |
8.7 |
|
|
Weight, kg |
60.3 |
10.1 |
66.3 |
11.5 |
62.8 |
11 |
|
|
Blood pressure |
|||||||
|
Systolic |
129.9 |
15.2 |
138.5 |
20 |
134.1 |
18.1 |
|
|
Diastolic |
70.8 |
10.9 |
73.4 |
12.7 |
72 |
11.8 |
|
Table 1: Demographic data of participants between FF and MAE groups.
Effects of the FF on biochemistry, CBC and frailty
As shown in Table 2, we found that the intake of FF increased the HDL-C from 48.8 ± 12.7 mg/dl to 50.8 ± 14.6 mg/dl (p=0.049). The albumin levels increased from 4.13 ± 0.32 g/dl to 4.25 ± 0.27 g/dl (p=0.027) after the intake of FF for 5 weeks. Total White Blood Cells (WBC) and Red Blood Cells (RBC) were not significant difference before and after the intake of FF. Differential counts of WBC were not significantly different except basophils increased significantly from 0.69 to 0.76 cells/ul. Hemoglobin (Hb) and Hematocrit (Hct) levels were not significant differences, but Mean Corpuscular Volume (MCV) significantly increased from 91.9 to 92.4 (pl/cells) after the intake of FF. As shown in Table 3, we found that the frailty rate in the study population was 35% (â?§ 3 of 5 items). The intake of FF improved the frailty at slow walking speed (p=0.021) but not weight loss, fatigue feeling, low physical activity, or grip strength (Table 3) [14].
| Parameters | Pre-test | Post-test | t | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | p | ||||
|
HDL-C (mg/dl) |
48.8 |
12.7 |
50.8 |
14.6 |
-2.043 |
0.049 |
|
|
|
LDL-C (mg/dl) |
99 |
33.8 |
96.2 |
34.9 |
0.969 |
0.339 |
|
|
|
Albumin (gm/dl) |
4.13 |
0.32 |
4.25 |
0.27 |
-2.477 |
0.027 |
|
|
|
WBC (cells/ul) |
6230.6 |
1238.3 |
6027.5 |
932.4 |
1.28 |
0.209 |
|
|
|
RBC (× 106 cells/ul) |
4.53 |
0.48 |
4.51 |
0.44 |
0.601 |
0.552 |
|
|
|
Hemoglobin (gm/dl) |
14.1 |
1.4 |
14 |
1.3 |
0.164 |
0.87 |
|
|
|
Hematocrit (%) |
41.6 |
4 |
41.7 |
3.8 |
-0.231 |
0.819 |
|
|
|
MCV (pl/cell) |
91.9 |
3.6 |
92.4 |
4.2 |
-2.218 |
0.033 |
|
|
|
MCH (pg/cell) |
31.1 |
1.6 |
31.2 |
1.5 |
-1.245 |
0.221 |
|
|
|
MCHC (gm/dl) |
33.8 |
1.1 |
33.7 |
0.9 |
0.879 |
0.386 |
|
|
|
Platelet (× 103/ul) |
218 |
57.4 |
210.6 |
55.7 |
1.748 |
0.089 |
|
|
|
Neutrophil (cells/ul) |
60.2 |
10.3 |
60.9 |
8.2 |
-0.783 |
0.439 |
|
|
|
Lymphocyte (cells/ul) |
29.4 |
9.2 |
29.1 |
7.8 |
0.449 |
0.656 |
|
|
|
Monocyte (cells/ul) |
6.28 |
1.53 |
6.23 |
1.37 |
0.246 |
0.807 |
|
|
|
Basophil (cells/ul) |
0.69 |
0.28 |
0.76 |
0.23 |
-2.236 |
0.032 |
|
|
|
Eosinophil (cells/ul) |
3.48 |
2.86 |
3.09 |
1.91 |
1.226 |
0.229 |
|
|
Table 2: Data of biochemistry and complete blood counts in FF participants.
| Parameters | MAE (n=49) | FF (n=36) | ||||
|---|---|---|---|---|---|---|
| Pretest | Post-test | p | Pretest | Post-test | p | |
|
Weight loss |
0.053 |
0 |
- |
0.154 |
0.103 |
0.687 |
|
Fatigue feeling |
0.342 |
0.053 |
0.001 |
0.205 |
0.231 |
1 |
|
Low physical activity |
0.4 |
0.114 |
0.006 |
0.41 |
0.308 |
0.454 |
|
Grip strength |
0.364 |
0.273 |
0.5 |
0.385 |
0.436 |
0.754 |
|
Slow walking |
0.522 |
0.565 |
1 |
0.538 |
0.282 |
0.021 |
|
|
||||||
Table 3: Changes of frailty rates before and after MAE and FF.
Effects of MAE on biochemistry, CBC, and frailty
The MAE for 10 weeks did not significantly increase blood albumin or cholesterol levels (Table 4). The MAE did increase the RBC significantly from 4.26 to 4.33 (x106 cells/ul), but decreased the MCV from 94.8 to 94.2 pl/cell. The platelet counts increased from 203.1 to 212.6 (x103/ul), which did not reach a significant increase (p=0.085). The MAE for 10 weeks had no significant effects on differential counts of WBC. The MAE improved the frailty at fatigue feeling (p=0.001) and low physical activity (p=0.006) but not at slowly walking speed, weight loss, or grip strength (Table 4) [15].
| Parameters | Pre-test | Post-test | T | P | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| HDL-C (mg/dl) | 57 | 15 | 55.5 | 16.3 | 1.393 | 0.173 |
| LDL-C (mg/dl) | 91.9 | 27.2 | 92.8 | 27.2 | -0.214 | 0.832 |
| Albumin (gm/dl) | 4.42 | 0.26 | 4.46 | 0.22 | -1.104 | 0.278 |
| WBC (cells/ul) | 6142.3 | 1482.6 | 6246.6 | 1438.8 | -0.675 | 0.504 |
| RBC (× 106 cells/ul) | 4.26 | 0.48 | 4.33 | 0.52 | -2.141 | 0.038 |
| Hemoglobin (gm/dl) | 13.1 | 1.4 | 13.3 | 1.5 | -1.589 | 0.119 |
| Hematocrit (%) | 40.3 | 4 | 40.7 | 4.4 | -1.207 | 0.234 |
| MCV (pl/cell) | 94.8 | 5.3 | 94.2 | 5 | 2.702 | 0.01 |
| MCH (pg/cell) | 30.9 | 2 | 30.8 | 1.9 | 1.966 | 0.056 |
| MCHC (gm/dl) | 32.6 | 0.9 | 32.6 | 0.8 | -0.633 | 0.53 |
| Platelet (× 103/ul) | 203.1 | 65.4 | 212.6 | 63.8 | -1.766 | 0.085 |
| Neutrophil (cells/ul) | 63.9 | 8.6 | 64.4 | 6.6 | -0.543 | 0.59 |
| Lymphocyte (cells/ul) | 26.7 | 7.7 | 26.4 | 6.5 | 0.496 | 0.622 |
| Monocyte (cells/ul) | 6.44 | 1.85 | 6.2 | 1.47 | 1.14 | 0.261 |
| Basophil (cells/ul) | 0.62 | 0.35 | 0.6 | 0.35 | 0.296 | 0.769 |
| Eosinophil (cells/ul) | 2.33 | 1.81 | 2.45 | 1.86 | -0.529 | 0.6 |
Table 4: Data of biochemistry and complete blood counts in participants with MAE.
The comparative effects between FF and MAE
We used Generalized Estimating Equation (GEE) statistics to compare the different effects of the FF and MAE on CBC and biochemistry (Table 5). We found that the participants in the FF group revealed a significantly better impact on the HDL-C level (Wald X2=4.32, p=0.038). In contrast, participants in the MAE group compared to the FF group significantly increased RBC (Wald X2=3.86, p=0.049) and platelets (Wald X2=6.69, p=0.01), suggesting that MAE for 10 weeks tends to enhance hematopoiesis on RBC and platelets [16].
| Groups parameters | MAE changes | FF changes | Wald X2 | p* |
|---|---|---|---|---|
| HDL-C (mg/dl) | -1.56 | 2.03 | 4.316 | 0.038 |
| LDL-C (mg/dl) | 0.97 | -2.86 | 2.327 | 0.127 |
| Albumin (gm/dl) | 0.04 | 0.13 | 0.058 | 0.81 |
| WBC (cells/ul) | 104.32 | -203.06 | 0.846 | 0.358 |
| RBC (× 106 cells/ul) | 0.07 | -0.02 | 3.861 | 0.049 |
| Hemoglobin (gm/dl) | 0.15 | -0.01 | 1.7 | 0.192 |
| Hematocrit (%) | 0.38 | 0.07 | 0.426 | 0.514 |
| MCV (pl/cell) | -0.64 | -0.54 | 14.120 | <0.001 |
| MCH (pg/cell) | -0.13 | 0.09 | 5.13 | 0.024 |
| MCHC (gm/dl) | 0.06 | -0.09 | 1.336 | 0.248 |
| Platelet (× 103/ul) | 9.5 | -7.39 | 6.689 | 0.01 |
| Neutrophil (cells/ul) | 0.49 | 0.69 | 0.152 | 0.697 |
| Lymphocyte (cells/ul) | -0.35 | -0.33 | 0.005 | 0.944 |
| Monocyte (cells/ul) | -0.25 | -0.05 | 0.525 | 0.469 |
| Basophil (cells/ul) | -0.01 | 0.07 | 1.437 | 0.231 |
| Eosinophil (cells/ul) | 0.12 | -0.39 | 3.373 | 0.066 |
| Note: p* values are calculated by Generalized Estimating Equation (GEE) analysis adjusted for gender, age and body weight. | ||||
Table 5: Changes of blood biochemistry and complete blood counts between MAE and FF group participants.
Discussion
Results from this study showed that the intake of FF increased the HDL-C and albumin levels, suggesting improvement in metabolism and nutrition. In contrast, the MAE appeared to increase RBC and platelets, suggesting the MAE might enhance erythropoiesis and thrombopoiesis in older adults with age over 70 in this study [17].
Frailty is closely associated with IPA and nutritional status. Inappropriate nutrient intake has been shown to cause a risk of malnourishment and frailty in older adults [18]. Poor appetite, and low protein intake and low vitamin D intake have been correlated to frailty. A clinical trial with higher protein intake for 12 weeks has been shown to increase muscle mass and physical activity in frail elders. Proper supplementation of functional food may be applied to improve nutrition and functional activity. We showed in this study that additional supplementation of chicken moose and milkfish in softened texture with herbs fragrance 5 times a week for 5 weeks did improve the blood albumin level, HDL-C level, and better walking speed. Although this short-term administration of higher protein intake did not improve fatigue feeling, weight gain, or muscle strength, a more prolonged supplementation or a combination with physical exercise may improve both nutrition and physical activity [18].
Different exercises have been shown to prevent physical dysfunctions and reverse frailty in older adults. However, older adults with different ages and comorbidities may require different styles of exercises, aerobic, resistant, or balanced training. Combined training on strength, endurance, and balance has been shown the best to prevent falls and improve balance and physical performance in the frailty elderly. The problem is how to encourage older adults to exercise regularly and practice moderate exercise without falls or cardiopulmonary exacerbation safely. Employing the MAE, which is a moderate exercise with harmonious posture in musical rhythm we showed that the MAE exercise 3 times (50 minutes a session) a week for 12 weeks, increased erythropoiesis and thrombopoiesis in addition to improving fatigue feeling and physical activity. The MAE alone did not improve nutrition status on blood albumin levels or blood cholesterol levels in the study population with an average of 76 years of age [19].
Limitations of the study include 1) This study was not a randomized control trial, 2) The FF group completed only 5 weeks of additional high protein FF, and 3) The participants in the MAE group had a high rate of female participants. Moreover, the outcome measurements were limited to blood biochemistry and frailty scales but not biomarkers of senescence or aging. We recently identified that older adults had a significantly higher Senescence-Associated Secretory Phenotype (SASP) in urinary extracellular vesicles than young adults. We thus propose that a combination of active aging exercise and functional food might improve nutrition, immunity, and frailty based on the pre- and post-interventional monitoring of aging biomarkers by non-invasive point-of-care tests of SASP in urinary extracellular vesicles [20].
Conclusion
Results from this study suggest that FF and MAE for older adults have different effects on nutrition status, hematopoiesis, biochemistry, and frailty. Further studies will investigate whether a combination of both FF and MAE for older adults improves physical function, nutrition, frailty, and mental health scales.
Conference Presentation
This study was partly presented in the American Geriatric Society 2023 (AGS23) annual scientific meeting at Long Beach, Los Angeles, as a poster with ID: 3863755.Author Contributions
Conceptualization, S.Y., and K.Y.; methodology, C.L., and J.W.; software, M.L.; validation, C.L., M.L., and S.Y.; formal analysis, M.L.; investigation, C.L., and S.Y.; resources, S.Y.; data curation, M.L., and K.Y.; writing original draft preparation, S.Y.; writingreview and editing, K.Y.; project administration, S.Y.; funding acquisition, S.Y, and J.W. All authors have read and agreed to the published version of the manuscript.Funding
This work was supported by grants MOST 110-2314-B-715-008 (for SY) and MOST 109-2811-B-195-503-MY3 (for KY) from the National Sciences Technology Council, Taiwan, and by grants MMC-RD-109-1C-04, and MMc-RD-109-1B-16 from Mackay Medical College.Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of MacKay Memorial Hospital for studies involving humans (code 19MMHIS019e and 2019/01/21 of approval).Informed Consent Statement
Informed consent was obtained from all participants involved in the study.Acknowledgments
The authors would like to present their appreciation to the participants and staff from eight long-term care institutes involved in this study.Conflicts of Interest
The authors declare no conflict of interest.References
- OzsUrekci C, Kara M, Gungor AE, Aycicek GS, CalÃÂ?±skan H, Dogu BB, et al. Relationship between Chewing Ability and Malnutrition, Sarcopenia, and Frailty in Older Adults. Nutr Clin Pract. 2022;37(6):1409-1417.
- Woo J, Tong C, Yu R. Chewing Difficulty Should be Included as a Geriatric Syndrome. Nutrients. 2018;10(12):1997.
- Breen L, Stokes KA. Chirchward-Venne TA, Moore DR, Baker KS, Smith K, et al. Two Weeks of Reduced Activity Decreases Leg Lean Mass and Induces “Anabolic Resistance” of Myofibrillar Protein Synthesis in Healthy Elderly. J Clin End Metab. 2013;98(6):2604–2612.
- Abreu MHD, Da Silva APL, Cavalcanti RVA, Cecilio Hallak Regalo S, Siéssere S, Gonçalves FM, et al. Prevalence of Chewing Difficulty in Older People in Long-term Care: A systematic review and meta-analysis. Gerodontology. 2023;40(1):10-25.
- Yeh SH, Pan MH. Chewing Screen and Interventions for Older Adults. Hu Li Za Zhi. 2020;67(4):6-13.
- Lubs L, Peplies J, Drell C, Bammann K. Cross-sectional, and Longitudinal Factors Influencing Physical Activity of 65 to 75-year-olds: A Pan European Cohort Study Based on the Survey of Health, Ageing and Retirement in Europe (SHARE). BMC Geriatr. 2018;18(1):94.
- Ohtsubo T, Nozoe M, Kanai M, Yasumoto I, Ueno K. Association of Sarcopenia and Physical Activity with Functional Outcome in Older Asian Patients Hospitalized for Rehabilitation. Aging Clin Exp Res. 2022;34(2):391-397.
- Hiltunen K, Saarela RKT, Kautiainen H, Roitto HM, Pitkala KH, Mäntyla P. Relationship between Fried's Frailty Phenotype and Oral Frailty in Long-term Care Residents. Age Ageing. 2021;50(6):2133-2139.
- Woo J, Tong C, Yu R. Chewing Difficulty Should be Included as a Geriatric Syndrome. Nutrients. 2018;10(12):1997.
- Yeh SH, Chuang H, Lin LW, Hsiao CY, Eng HL. Regular Tai Chi Chuan Exercise Enhances Functional Mobility and CD4CD25 Regulatory T Cells. Br J Sports Med. 2006;40:239-43. [Crossref]
[Google Scholar][PubMed]
- Hung JW, Liou CW, Wang PW, Yeh SH, Lin LW, Lo SK, et al. Effect of 12-week Tai Chi Chuan Exercise on Peripheral Nerve Modulation in Patients with Type 2 Diabetes Mellitus. J Rehabil Med. 2009;41:924-929.
- Lin SL, Huang CY, Shiu SP, Yeh SH. Effects of Yoga on Stress, Stress Adaption, and Heart Rate Variability Among Mental Health Professionals-A Randomized Controlled Trial. Worldviews Evid. Based Nurs. 2015;12(4):236-245.
- Yeh SH, Lai HL, Hsiao CY, Lin LW, Chuang YK, Yang YY, et al. Moderate Physical Activity of Music Aerobic Exercise Increases Lymphocyte Counts, Specific Subsets, and Differentiation. J Phys Act Health. 2014;11(7):1386-1392.
- Yeh SH, Lin LW, Chuang YK, Liu CL, Tsai LJ, Tsuei FS, et al. Effects of Music Aerobic Exercise on Depression and Brain-derived Neurotrophic Factor Levels in Community-Dwelling Women. Biomed Res Int. 2015:135893.
- Hsiao YS, Yeh SH. Current Status and Prospects for Nutritional Care of Patients with Dysphagia. VGH Nursing. 2018;35:2-9.
- Matsuo K, Fujishima I. Textural Changes by Mastication and Proper Food Texture for Patients with Oropharyngeal Dysphagia. Nutrients. 2020;12(6):1613.
- Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Cardiovascular Health Study Collaborative Research Group. Frailty in Older Adults: Evidence for A Phenotype. J Gerontol A Biol Sci Med Sci. 2001:56:146-156. [Crossref][Google Scholar][PubMed]
- Groessl EJ, Kaplan RM, Rejeski WJ, Katula JA, Glynn NW, King AC, et al. Physical Activity and Performance Impact Long-term Quality of Life in Older Adults at Risk for Major Mobility Disability. Am J Prev Med. 2019;56(1):141-146.
- Moradell A, Fernandez-Garcia AI, Navarrete-Villanueva D, Sagarra-Romero L, Gesteiro E, Perez-Gomez J, et al. Functional Frailty, Dietary Intake, and Risk of Malnutrition. Are Nutrients Involved in Muscle Synthesis the Key for Frailty Prevention? Nutrients. 2021;13(4):1231.
- Hernandez Morante JJ, Gomez Martinez C, Morillas-Ruiz JM. Dietary Factors Associated with Frailty in Old Adults: A Review of Nutritional Interventions to Prevent Frailty Development. Nutrients. 2019;11(1):102.
Citation: Yang KD, Pan MH, Yeh SH, Lee CH, Lee MT, Wang JH, et al. (2025) Different Effects of Functional Food and Music Aerobic Exercise on Complete Blood Counts, Blood Biochemistry and Frailty Scores of Older Adults. J Aging Sci. 13:405.
Copyright: © 2025 Yang KD, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

