Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Scientific Indexing Services (SIS)
- Euro Pub
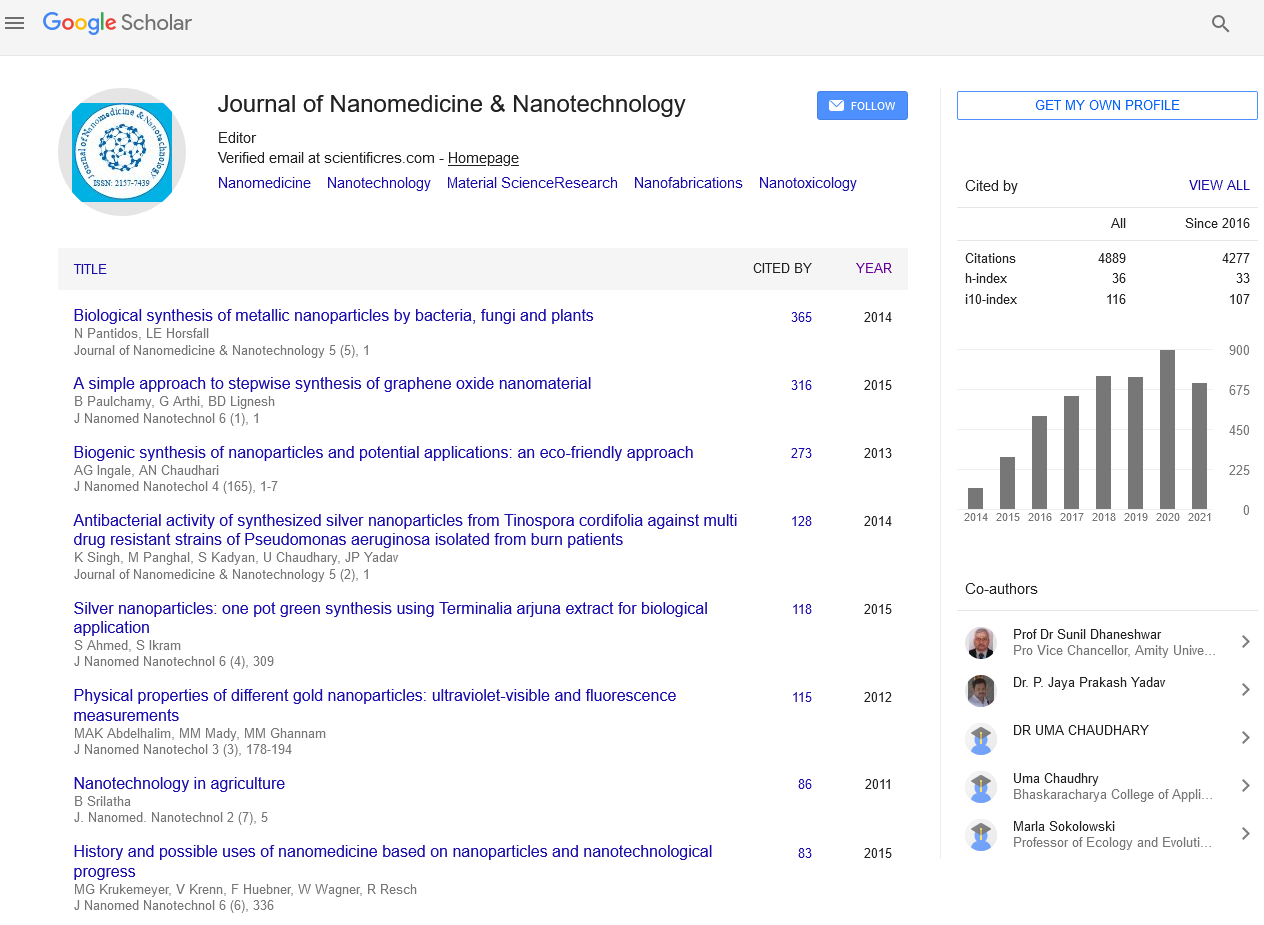
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Paramagnetic nanoparticles conjugated with lipopolysaccharide for blood-brain barrier disruption in a model of glioblastoma
2nd International Conference and Exhibition on Pharmaceutical Nanotechnology & Nanomedicine
March 20 - 21, 2019 | New York, USA
Andrew J Kobets
Childrenā??s Hospital at Montefiore, USA
Scientific Tracks Abstracts: J Nanomed Nanotechnol
Abstract:
Background: Glioblastoma (GBM) is the most aggressive primary adult brain tumor with only 14.6 months of median survival. Carrier nanoparticles have emerged as a novel strategy for chemotherapeutic delivery, yet penetration of the blood-brain barrier (BBB) and tumor retention remain significant hurdles. The evolution of paramagnetic nanoparticles (PMNPs) shows promise for reliable, magnetically-targeted drug delivery, and coupled with a lipopolysaccharide-coating (LPSPMNPs) allows for concurrent, reversible BBB disruption.
Methods: Luciferase-expressing GBM6 cells were implanted intracranially in nu/nu immunodeficient mice to model GBM in two experiments. First, bioluminescence assays (BLIs) characterized tumor growth postoperatively in cohorts administered LPS-PMNPs, inert PNMPs (OA-PMNP), or saline intravenously at four weeks. Magnets were positioned external to the tumor for onehour post-injection. Subsequent BLIs trended tumor growth with survival. The second experiment involved LPS-PMNPs, OAPMNPs, or saline injection postoperatively, followed by magnetic localization. Afterward, Evans blue dye (EBD) was administered as an albumin-bound marker of BBB breakdown. The mice were perfused, the tumors homogenized, and the dye extracted for spectrophotometric assessment.
Results: Tumor size doubled every 5.8 days, and mice expired at a mean 52 days. LPS-PMNPs reduced BLI signal three days post-injection compared to both OA-PMNPs and saline (p=0.02). This effect was reversed six days post-injection (p=0.39). EBD was significantly extravasated in LPS-PMNP-treated tumors compared to all other tumors (p=0.011). No immediate particle-associated adverse reactions occurred and survival was similar between all groups (p=0.27) with a trend toward survival between the LPS group and highest-dose PMNP group (53.5 vs. 47.8 days, p=0.12).
Conclusion: The BBB can be safely and reversibly disrupted for targeted permeability of large molecules in a model of GBM. LPS induces transient disruption of bioluminescence of tumors and increases tumor absorption of albuminbound EBD. Future work will start with packaging known chemotherapeutics not normally BBB permeable in LPSPMNPs to determine delivery efficacy and anti-neoplastic effects on survival.
Biography :
Andrew Kobets is currently a Chief Resident of a neurosurgical resident at Montefiore Medical Center and is working on a translational research project as a Visiting Scientist at both the Feinstein Institute for Medical Research at Northwell Health and at the Albert Einstein College of Medicine. He has initiated and overseen the initiation of three clinical trials in the Department of Neurological Surgery at Montefiore Medical Center and is the first utilizing MR elastography to evaluation shunt function in New York. Andrew graduated from the Yale School of Medicine with a medical degree and a masters in health sciences. He studied systems neuroscience at the Johns Hopkins University as an undergraduate and will return to Johns Hopkins after residency for a fellowship in pediatric neurosurgery.
E-mail: Akobets@montefiore.org