Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- The Global Impact Factor (GIF)
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
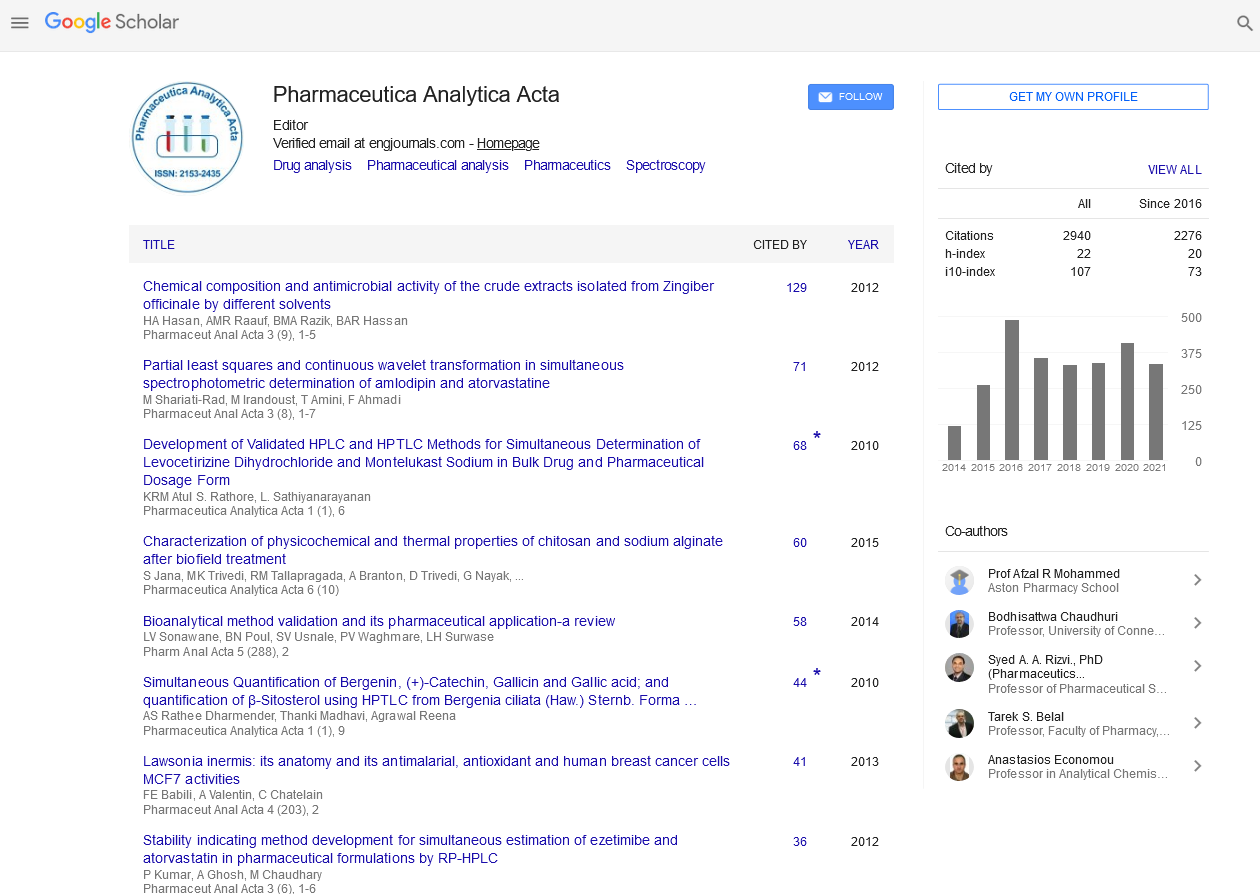
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Isolation and characterization of NDM-1 producing Klebsiella pneumoniae from three Palestinian hospitals
18th Annual Pharmaceutical and Chemical Analysis Congress
November 05-06, 2018 | Madrid, Spain
Mamoun Ibaideya, Ibrahim Alsahouri, Abeer Fathi and Issa Shtayah
Palestinian Medical Complex, Palestine
Beit Jala Governmental Hospital, Palestine
Rafedia Surgical Hospital, Palestine
Central Public Health Laboratory, Palestine
Posters & Accepted Abstracts: Pharm Anal Acta
Abstract:
Introduction: Klebsiella pneumoniae can cause an extensive variety of diseases, including meningitis, bacteremia, wound infection, pneumonia, urinary tract infection, etc. This life form is getting to be impervious to an extensive gathering of antimicrobials, particularly ?-lactam anti-infection agents. The reason for multidrug resistance may be the production of extended-spectrum ?-lactamases (ESBLs), carbapenemase/metallo ?-lactamases or AmpC ?-lactamases or changes in the bacterial cell wall structure. The aim of the present study was to isolate and characterize carbapenem resistant Klebsiella pneumoniae isolated from the patients admitted to one of three Palestinian hospitals (Palestinian Medical Complex, Rafedia Surgical Hospital, and Beit Jala Governmental Hospital) west bank, Palestine. Materials & Methods: Nineteen Klebsiella pneumoniae CRE (carbapenem-resistant Enterobacteriaceae) isolates were collected from three hospitals during the period from June 2017 to February 2018. Antibiotics susceptibility testing was performed by standard disc diffusion method (Kirby Bauer) except colistin and meropenem (done by E test) as recommended by CLSI 2017 and CLSI 2018, combination disc method, modified Hodge test, modified carbapenem inactivation method (mCIM), EDTA carbapenem inactivation method (eCIM), EDTA-IPM vs. IPM disc synergy test and cefoxitin disc test were performed for detection of ESBLs, carbapenemases, metallo ?-lactamases, and AmpC ?-lactamases, respectively. Polymerase chain reaction (PCR) was used to detect carbapenemases-encoding genes. Clonal relationships were analyzed by pulsed field gel electrophoresis (PFGE). Results: Nineteen carbapenem-resistant Klebsiella pneumoniae were isolated from wounds, sputum and blood specimens, all the isolates were resistant to all the ????lactam antibiotics including the carbapenems and all these isolates harbored blaNDM-1 genes. Two clinical Klebsiella pneumoniae isolates harboring both blaNDM-1 and blaOXA48. Two others harboring both blaNDM-1 and blaKPC2, the blaCTX-M, blaSHV and blaTEM genes were also present in most isolates. PFGE analysis showed that blaNDM-1 producing Klebsiella pneumoniae were clonally related. Conclusion: Increased frequency of multi-drug resistance supports the need for continuous surveillance to determine prevalence and evolution of these proteins in Palestinian hospitals.
Biography :
E-mail: mamoun.obeidia@iah.ps