Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
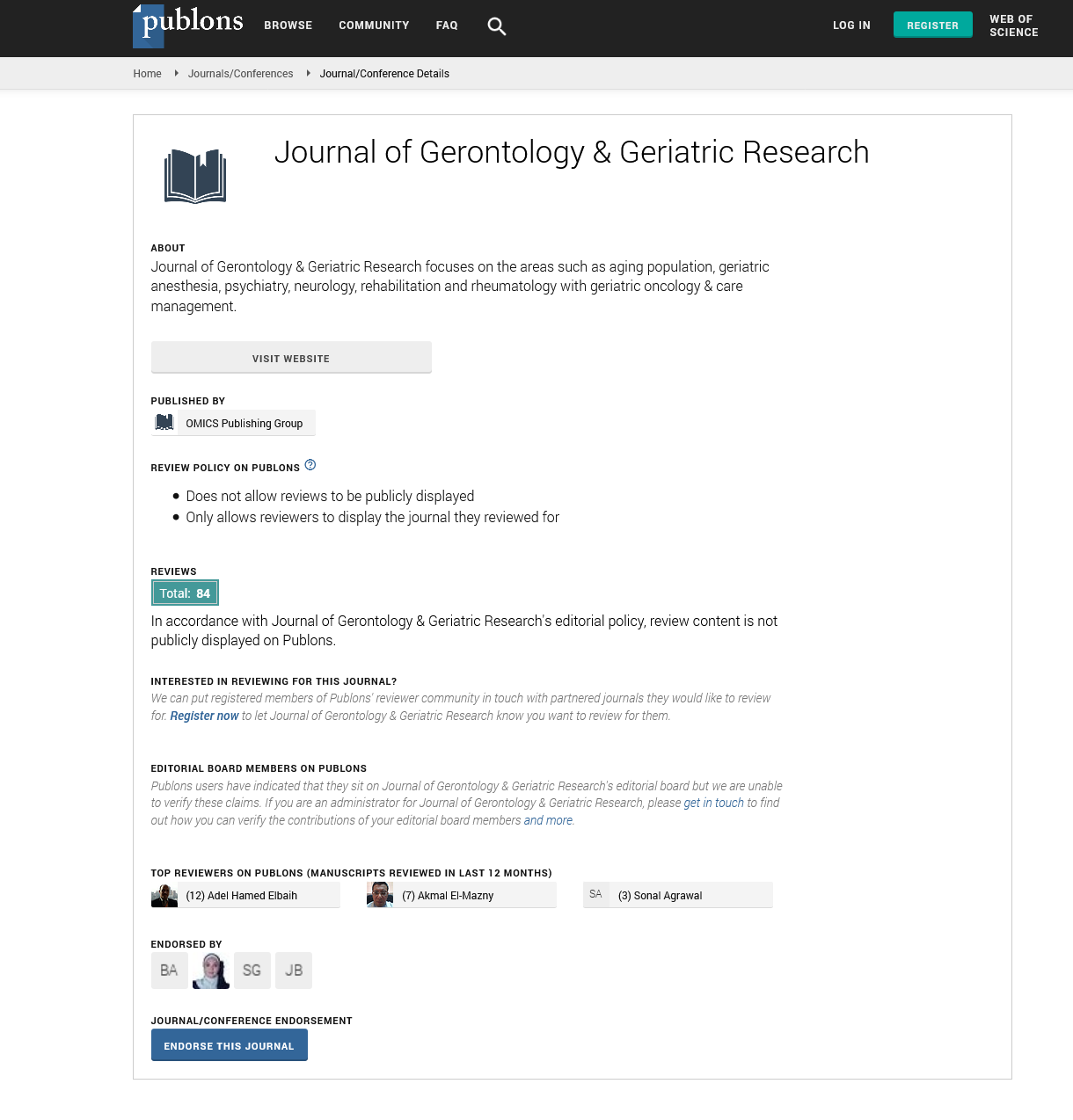
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Editorial - (2022) Volume 11, Issue 2
Traumatic Brain Injury in the Older Adults
Jothi Vasudev*Received: 11-Feb-2022, Manuscript No. jggr -22-15768; Editor assigned: 13-Feb-2022, Pre QC No. P-15768; Reviewed: 18-Feb-2022, QC No. Q-15768; Revised: 23-Feb-2022, Manuscript No. R-15768; Published: 28-Feb-2022, DOI: 10.35248/2167-7182.22.11.600
Editorial
Traumatic Brain Injury (TBI) is a silent pandemic, and elderly people with TBI are an apparently silent population within this silent epidemic. Although it is well understood that older age has a negative impact on outcome following TBI, studies clarifying why this is so, as well as information on age-appropriate therapy of senior TBI patients, are scarce. Moreover, despite the fact that geriatric and neurotrauma researchers have identified the prognostic significance of preadmission functional ability, the presence of comorbidities, sex, and other factors such as Cerebral Perfusion Pressure (CPP) on recovery after illness or injury in older adults with TBI, these variables have received little attention in older adults with TBI. The exclusion of these factors in neuroscience research could explain why predicting outcomes and providing care to older adults with TBI is so difficult. The current "one-sizefits- all" approach to TBI management typically ignores the special problems of the elderly. The epidemiology of TBI in older people and the factors that influence patient outcomes are examined in this study, with a focus on the implications of current information and recommendations for further research and therapeutic inquiry.
Age has long been recognised as a predictor of poor TBI prognosis on its own. The mechanism through which this occurs is unknown. Because studies have been unable to discover useful clinical predictors of lesion formation, head CT scans are now recommended for all patients 65 and older with neurological symptoms and signs or a history of head trauma to aid in TBI diagnosis. Frailty syndrome and chronic diseases have many parallels, including a higher frequency in older people, simultaneous multimorbidities and impairments, and a general tendency toward increasingly severe disease states over time. Furthermore, patients and caregivers living with frailty and chronic diseases face a common set of challenges, including persistent symptoms, mental anguish, disability and functional loss, complex medical regimens, difficult lifestyle modifications, and receiving beneficial medical treatment. As a result, frailty therapeutic therapy for older people should incorporate unique and effective features of chronic illness care.
Older persons with moderate TBI have a much greater mortality rate than their younger counterparts. Although a single study found that adults aged 60 and older with mild TBI had significantly higher functioning (P.05) on the Glasgow Outcome Scale (GOS) at one month after injury than younger people with mild TBI, significance was lost when work status was included. Investigations into impairment after TBI have discovered evidence that older adult TBI survivors are more dependent than younger survivors, using global outcome measures such as the GOS and the Functional Independence Measure [1-5].
As a result, older people who have suffered a TBI have longer hospital stays and are more prone to have delayed neurological disability. As a result of their extended hospital stays, the cost of their care is substantially higher. Despite having lower injury severity scores and higher mean GCS scores than their younger peers, they had longer stays. When older TBI patients are referred to inpatient rehabilitation facilities, their stays are longer, which raises costs. The trauma literature has shed additional light on the outcomes of older people who have suffered a TBI. Elder trauma patients required more medical and specialised consultations for each injury and had more complications while in the hospital than their younger injured colleagues. Given that older adults demonstrate slower rates of functional change after recovery from TBI, the focus on early outcome time points (e.g., discharge) in currently available outcome studies in older adult TBI patients is a limitation. This is an important consideration in future intervention and study design.
REFERENCES
- Keller JM, Sciadini MF, Sinclair E, O’Toole RV. Geriatric Trauma: Demographics, Injuries, and Mortality. J Orthop Trauma. 2012;26:5.
- Samaras N, Chevalley T, Samaras D, Gold G. Older Patients in the Emergency Department: A Review. Ann Emerg Med. 2010;56:261-269.
- Betjemann JP, Lowenstein DH. Status epilepticus in adults. Lancet Neurol. 2015;14:615-624.
- Koubeissi M, Alshekhlee A. In-hospital mortality of generalized convulsive status epilepticus: A large US sample. Neurology. 2007;69:886-893.
- Dham BS, Hunter K, Rincon F. The epidemiology of status epilepticus in the United States. Neurocrit Care. 2014;20:476-483.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Citation: Vasudev J (2022) Traumatic Brain Injury in the Older Adults. J Gerontol Geriatr Res. 11: 600. DOI: 10.35248/2167-7182.22.11.600
Copyright: © 2022 Vasudev J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.