Indexed In
- Open J Gate
- Genamics JournalSeek
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2023) Volume 13, Issue 1
Subdural Haemorrhage: A Case Report
Amartya De1*, Dipan Biswas2 and Shraddha Basu12Department of Pharmacy, Radha Gobindakar (R.G.Kar) Medical College & Hospital, Kolkata, India
Received: 02-Jan-2023, Manuscript No. CPECR-23-18965; Editor assigned: 04-Jan-2023, Pre QC No. CPECR-23-18965 (PQ); Reviewed: 18-Jan-2023, QC No. CPECR-23-18965; Revised: 23-Jan-2023, Manuscript No. CPECR-23-18965 (R); Published: 03-Feb-2023, DOI: 10.35428/2161-1459.23.13.348
Abstract
A subdural hemorrhage (hematoma) is a type of bleeding that occurs outside the brain as a result of a severe head injury occurs when a blood vessel ruptures between the brain and the leathery membrane that surrounds it. A 78 year-old male presented with drowsiness and altered sensorium. He had accidental domestic fall at his residence twice in an interval of one hour. Subdural Haemorrhage was revealed in the CT scan. For Burr hole decompression a high index suspicion and investigation with a computed tomography of the brain to reach the diagnosis of subdural haemorrhage is important.
Keywords
Subdural haemorrhage; Unilateral; Bilateral; Morbidity; Burr hole decompression
INTRODUCTION
Subdural Haemorrhage (SDH) is a common intracranial haemorrhage that is associated with significant morbidity [1]. The bleeding or haemorrhage occurs within the layers of tissue that surround the brain. SDH is managed by surgical or non-surgical way [2]. The surgical techniques involve burr-hole craniotomy with or without continuous closed-system drainage, small craniotomy with endoscopic removal and large craniotomy followed by membranectomy [2-4].
The symptoms of subdural haemorrhage depend on how quickly blood accumulates inside the skull. It typically presents with headache, seizure, altered mental state and extra pyramidal syndromes e.g. dystonia and dyskinesia. Diagnosis requires a high index of suspicion based on the clinical presentation, as sometimes the patient may not reveal that they had any trauma unless asked specifically. Computed tomography is needed for diagnosis because it is able to delineate larger bleeds [5].
Case Presentation
A 78 year-old male was brought with a complaint of accidental domestic fall at residence twice in an interval of 1 hour. He was suffering from progressive drowsiness and altered sensorium. Pre-morbidly, he had hypertension and coronary artery disease (post PTCA) for which he was on antiplatelet drug. On physical examination his blood pressure was found to be 140/70 mm Hg and pulsed rate was 84 beats per minute. Neurological examination, including the Glasgow coma scale was 2/15 and plantar reflex was enhanced. Case was referred for urgent computed tomography of brain which showed right temporo-parietal subdural haemorrhage measuring 1.3 cm (Figures 1-3).

Figure 1: Computed Tomography (CT) scan, Unilateral Subdural Haemorrhage (SDH).
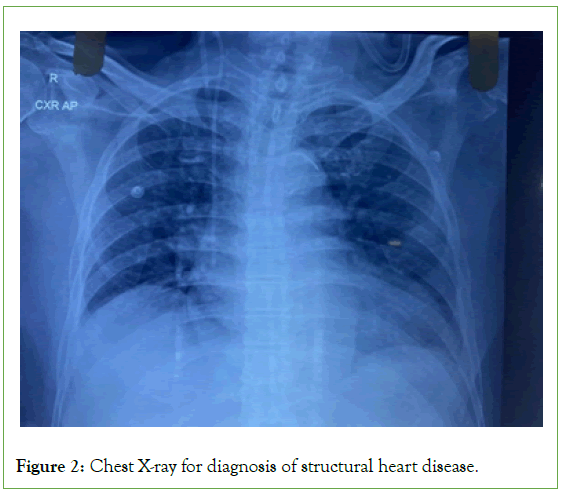
Figure 2: Chest X-ray for diagnosis of structural heart disease.
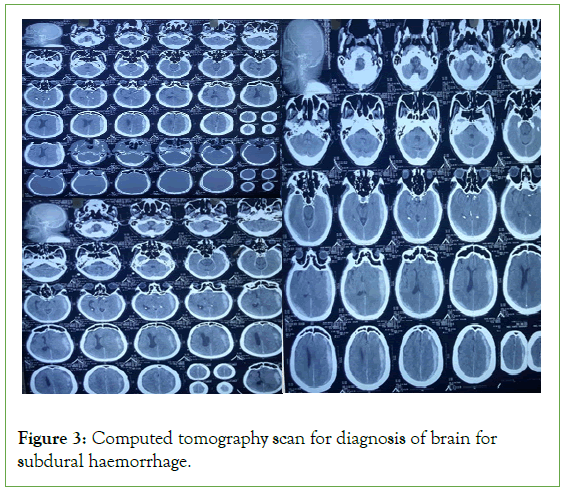
Figure 3: Computed tomography scan for diagnosis of brain for subdural haemorrhage.
To stabilize him, he was immediately administered:
• Inj Mannitol (D- mannitol, C6H14O6)-IV: 8 hourly
• Inj Lasix 20 (Furosemide 20 mg)-IV: Twice daily
• Inj Levipil 500 (Levetiracetam)-IV: Twice daily
• IVF NS 500 (Sodium Chloride 0.9% W/V): 12 hourly
• Inj Pan 40 (Pantoprazole 40 mg)-IV: Once daily
• Inj Futaz 4.5 (Piperacillin 400 mg +Tazobactum 500 mg)- IV: 8 hourly
• Inj Vit K (Phytomenadione)-IV: Once daily
• Tab Atorva 20 (Atorvastatin 20 mg): Once daily at bedtime
• Tab Cytoguard (Trimetazidine): Once daily at bedtime
His routine investigation was done and neurosurgeon opined surgery. The patient was not responding well. He was further given 4 unit of FFP (Fresh Frozen Plasma) and doctors planned for decompression craniectomy. His mannitol dose was changed to Inj Mannitol (50 ml ) 6 hourly. Doctors further added Nebu Duolin (Levosalbutamol+Ipratropium) Antihypertensive drug: 8 hourly.
These re-established his sensorium. Some more changes were done to his drug administration. He was introduced to:
• Liq Glycerine 6 tea spoon full: Thrice daily
• Tab Aldactone (Spironolactone 25 mg) 1 tab- Once daily
• Inj Mnnitol, Lasix and Levipil was withdrawn. Instead, he was administerd
• Liq Levipil 5 ml: Twice a day (post meals)
• Tab Dytor 10 (Torasemide 10 mg): Once daily
• Tab Crdace 2.5 (Ramipril 2.5 mg): Once daily
Rest was kept same as before. CT scan was done again. His Structural Heart Disease (SHD) was resolved by comparative study. Moreover, he was administered Tab Dexona 2 mg (Dexamethasone) twice daily. When his Total Leukocyte Count (TLC) increased, he was injected Dalcinex (Clindamycin) IV thrice daily.
Considering overall clinical appearance, doctors opted for Burr Hole decompression after 1 week. During surgery after 1 week, an incision was made in the scalp. The surgeon drilled one or two burr holes using a special drill and the access to dura was achieved. Then the dura was incised and excess fluid was evacuated to reduce the pressure within the skull. The wounds were then closed. Information on the findings during surgery is not available to us. Patient was intubated and kept for close observation at ICCU with ventilation support. The prognosis after surgery is usually good because of development of modern imaging methods and improvemen in surgical techniques. Then, he was warded in the neurological ward where he made an uneventful recovery.
Results and Discussion
Frequently, a subdural haemorrhage develops after traumatic brain injury. It may also occur in case of patients with significant cerebral atrophy or those with chronic alcohol abuse [6]. Subdural haemorrhage manifests between the dura and the arachnoid membranes and results due to shearing force or by spontaneous rupture of the bridging veins that drain blood from the surface of the brain to the dural sinuses. A subdural haemorrhage is usually venous in origin and often limits itself by the rising intracranial pressure. If the haemorrhage is of significant size, it can disrupt the physiologic flow of CSF and will in turn raise the intracranial pressure [7].
Recently, new evidence suggests that a chronic subdural haemorrhage (i.e. when the haemorrhage persists more than 3 weeks) enlarges because of recurrent spontaneous bleeding from a richly vascularised membrane encapsulating the haemorrhage due to a continuous process of angiogenesis, inflammation, coagulation and fibrolysis [8]. The expansion causes compression of functional cerebral tissue and thus causes neurologic deficiency.
A chronic subdural haemorrhage can be of two nature- Unilateral or Bilateral. Our patient was diagnosed with unilateral subdural haemorrhage. It occurs in majority of the patients. The recurrence rate in case of unilateral subdural haemorrhage is low.
Urgent evacuation is usually done in cases of subdural haemorrhage with burr hole decompression [7,8]. The excess mortality risk following chronic subdural haemorrhage persists throughout the life. Factors determining the risk of mortality will include the degree of disability or dependence upon discharge and the presence of cerebral atrophy medical risk factors like stroke and hypertension.
The risks of a burr hole procedure includes: Bleeding, Infection, Blood clots, Brain injury, Heart attack or stroke, No relief from symptoms and needing craniectomy.
A typical burr hole compression procedure involves: (1) An Intravenous line is put in the arm or hand of the patient just before the procedure. A medicine to make the patient feel relaxed and sleepy will be given through the IV or General anesthesia will be given. (2) During the procedure, patient’s vital signs will be closely monitored. (3) Hair will be trimmed in the area of the scalp and numbing medicine will be injected into the scalp. (4) An incision will be made in the scalp. (5) Using a special drill, the surgeon drills one or two small hole in the skull to expose the dura. (6) The surgeon then opens the dura and drains any excess fluid to reduce the pressure within the skull. (7) The surgeon then may place a temporary drain to continue the drainage of the fluid or the dura and scalp will be closed right away.
After the procedure, the patient needs to stay in the hospital for a few days for recovery. Even after the discharge of the patient, adherence to medication is important for patients having risk factors like hypertension, diabetes and dyslipidaemia, to prevent the complication of subdural haemorrhage [9].
Conclusion
In a nutshell, this was a case of unilateral subdural haemorrhage that presented in a 78 year-old male as a consequence of accidental domestic fall. Generally Subdural haemorrhage develops after traumatic brain injury, in this case it occured due to accidental domestic fall. It needed a high index suspicion and investigation with a computed tomography of the brain to reach the diagnosis of subdural haemorrhage before urgent burr hole decompression was done. Subdural Haemorrhage was revealed in the CT scan, which is best daignostic method.
Acknowledgement
We thank to Dr. Dipan Biswas, General physician, R.G. Kar hospital, to support us in preparing the case report.
Declaration
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Conflict of Interest
The author declares no conflict of interest.
References
- Adhiyaman V, Asghar M, Ganeshram KN, Bhowmick BK. Chronic subdural haematoma in the elderly. Postgrad Med J. 2002;78(916):71-75.
- Cheung RT, Eliasziw M, Meldrum HE, Fox AJ, Barnett HJ. Risk, types, and severity of intracranial hemorrhage in patients with symptomatic carotid artery stenosis. Stroke. 2003;34(8):1847-1851.
- Ellis GL. Subdural hematoma in the elderly. Emerg Med Clin N Am. 1990;8(2):281-294.
- Fujisawa H, Ito H, Kashiwagi S, Nomura S, Toyosawa M. Kallikrein-kinin system in chronic subdural haematomas: its roles in vascular permeability and regulation of fibrinolysis and coagulation. J Neurol Neurosurg Psy. 1995;59(4):388-394.
- Sangondimath G, Chhabra HS, Venkatesh R, Nanda A, Tandon V. A rare case of chronic subdural haematoma presenting with paraparesis: A case report and review of literature. J Clin Orthop Trauma. 2015;6(4):265-268.
[Crossref] [Google Scholar] [PubMed]
- Manickam A, Marshman LA, Johnston R. Long-term survival after chronic subdural haematoma. J Clin Neurosci. 2016;34:100-104.
[Crossref] [Google Scholar] [PubMed]
- Chia YC, Ching SM, Chew BN, Devaraj NK, Siti Suhaila MY, Tay CL, et al. May measurement month 2017 blood pressure screening: findings from Malaysia-South-East Asia and Australasia. Eur Heart J Suppl. 2019;21:77-79.
[Crossref] [Google Scholar] [PubMed]
- Devaraj NK. Prevalence, factors influencing, and knowledge about adherence to lipid-lowering therapy among hyperlipidemia patients. Int J Cardiol. 2017;249:7-8.
- Markwalder TM, Seiler RW. Chronic subdural hematomas: to drain or not to drain? Neurosurg. 1985;16(2):185-188.
Citation: De A, Biswas D, Basu S (2023) Subdural Haemorrhage: A Case Report. J Clin Exp Pharmacol. 13:348.
Copyright: © 2023 De A, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

