Indexed In
- Open J Gate
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 12, Issue 6
Prevalence of Carbapenem Resistant Enterobacteriaceae (CRE) Among Patients Admitted to Palestine Red Crescent Society Hospital in Hebron, Palestine
Amal M. Dofesh*Received: 24-Sep-2023, Manuscript No. CMO-23-23895; Editor assigned: 28-Sep-2023, Pre QC No. CMO-23-23895(PQ); Reviewed: 13-Oct-2023, QC No. CMO-23-23895; Revised: 19-Oct-2023, Manuscript No. CMO-23-23895(R); Published: 26-Oct-2023, DOI: 10.35248/2327-5073.23.12.370
Abstract
Carbapenem-Resistant Enterobacterales (CRE) pose a significant threat to global healthcare due to limited treatment options and high morbidity and mortality rates. Our study, conducted at Palestine Red Crescent Society Hospital, investigated the prevalence and acquisition dynamics of CRE colonization among patients from 2020 to 2023. Of the 5,445 patients, 219 met the inclusion criteria, with CRE prevalence varying annually (4.3%-6.28%). Notably, 22.7%-57.1% of patients exhibited CRE colonization upon admission, and 43.9%-77.2% acquired CRE during hospitalization. Comparatively, 24.0%-76.0% of patients acquired multidrug-resistant MDR bacteria. Our findings emphasize the need for vigilant monitoring and infection control measures to curb CRE transmission in healthcare settings.
Keywords
Carbapenem-resistant enterobacterales; Prevalence; Multidrug-resistant (MDR) bacteria; CRE colonization
Introduction
Carbapenem-Resistant Enterobacterales (CRE) infection is regarded as a serious threat to global health [1]. Treatment of CRE infection is difficult due to the limited number of effective antibiotics against CRE and it is associated with high morbidity and mortality [2,3]. Hospitals and patient populations have different rates of CRE colonization and infection [4]. CRE colonization and infection are more common in patients who have recently been hospitalized or who have been given broadspectrum antibiotics, especially carbapenems [5]. Community transmission of CRE from patients with CRE colonization and infection is also a serious concern [6].
The rise of CRE represents a complex interplay of factors, including the overuse and misuse of antibiotics and healthcare practices such as invasive procedures, prolonged hospital stays, and the increasing reliance on broad-spectrum antibiotics [7,8]. The adaptability of these bacteria, driven by mechanisms such as increased efflux pump-action and acquisition of plasmid-borne carbapenemase genes, have rendered traditional infection control measures less effective [9,10].
The prevalence of Carbapenem-Resistant Enterobacterales (CRE) colonization in hospitals varied across the studies. One study conducted in Hematological Malignancy (HM) patients found a colonization rate of 10.3% among screened patients [11]. In Siriraj Hospital, Thailand, the prevalence of CRE colonization upon admission was 15.5%, and 28.3% of patients acquired CRE during their hospitalization [12]. In 2012, Al- Makassed Hospital, Jerusalem NICU had an OXA-48-Producing Enterobacteriaceae (OPE) outbreak, infecting 49 patients and the Ministry of Health interventions reduced cases after genetic analysis identified the responsible strain [13]. In another study, the prevalence of CRE colonization in rural hospitals was 7%, while in urban hospitals it was 17% [14]. Overall, the prevalence of CRE colonization in hospitals ranged from 6.8% to 45% depending on the population and setting.
CRE colonization may provide a risk to patients because bloodstream invasion through injured mucosa may occur during severe mucositis in CRE colonized persons, resulting in subsequent bacteremia [15].
Furthermore, intestinal carriers of CRE may act as silent shedders, resulting in the spread of carbapenemase-producing genes such as blaNDM and blaOXA48 [16]. As a result, stopping the spread of CRE infection may rely on the correct identification of both infected patients and colonized carriers.
This study aimed to determine the prevalence of CRE colonization upon admission as well as the acquisition of CRE during hospitalization among patients at Palestine Red Crescent Society Hospital in Hebron, Palestine.
Materials and Methods
Rectal swabs were collected from each patient upon admission and at intervals of two to three times weekly throughout their hospitalization to monitor healthcare-associated infections.
Data collection
All rectal swab results were documented within AL-SAHEL program at PRCS Hospital. Data collection encompassed the period spanning from January 2020 to August 2023. These data were extracted at two critical time points: Upon patient admission and during the course of hospitalization. Subsequently, the data were exported to an Excel file before being transferred to SPSS version 23 for comprehensive analysis.
Microbiological analysis
Rectal swabs underwent thorough microbiological examination in accordance with the Clinical Laboratory Standards Institute (CLSI) guidelines. Each swab was directly plated on selective MacConkey agar media supplemented with meropenem to facilitate the growth of CRE (carbapenem-resistant enterobacteriaceae) while suppressing the proliferation of other microorganisms. The culture plates were then aerobically incubated at 37°C for a duration of 18 to 24 hours.
Subsequently, isolates were subcultured directly onto API 20 (bioMérieux, France) for bacterial identification in addition to CHROMagar Orientation (hyLabs, Israel), which selectively promoted the growth of multidrug-resistant organisms under aerobic conditions. Additionally, subculturing was performed on Muller Hinton Agar (MHA) to enable further identification and Antibiotic Susceptibility Testing (AST). This subculture took place at 37°C for 18 to 24 hours. All recovered colonies were interpreted as per the manufacturer's instructions.
Antibiotic Susceptibility Testing (AST)
Carbapenems, namely Ertapenem (ETP) and Meropenem (MEM), were used for enterobacterales testing, in addition to the Modified Carbapenem Inactivation Method (MCIM) Test. For the detection of Pseudomonas species, Meropenem (MEM), Zeftazidime (CAZ), and Chloramphenicol (C) were used.
Acinetobacter MDR (multidrug-resistant) detection entailed the use of antibiotics such as Amikacin (AK), gentamicin (CN), Ceftazidime (CAZ), Imipenem (IPM), Meropenem (MEM), Sulfamethoxazole/Trimethoprim (SXT), Ciprofloxacin (CIP), Levofloxacin (LEV), and Colistin (CT). The identification of Stenotrophomonas maltophilia involved the application of Levofloxacin (LEV), Sulfamethoxazole/Trimethoprim (SXT), and Meropenem (MEM).
Statistical analysis
The collected data were meticulously coded and entered into the statistical software SPSS version 23. Descriptive statistics, encompassing numbers and percentages, were employed to summarize qualitative variables. To discern significant differences between various groups, the Chi-square and Fisher's Exact Test were used for the comparison of qualitative variables. P values less than or equal to 0.05 were considered statistically significant.
Ethical approval statement
This research study has received ethical approval from the Palestine Red Crescent Society hospital. The study was conducted in full compliance with the ethical guidelines and regulations established by this review board.
Results
Prevalence of CRE colonization at PRCS in each year (from 2020–2023)
Out of the 5,445 patients included in the study, 219 met the enrollment criteria. The prevalence of CRE colonization in the hospital, as determined from rectal swab samples, exhibited annual variations, with rates of 4.3%, 2.8%, 3.6%, and 6.28% in the respective years. The expected rate is two CRE cases out of every 100 cases annually (2%) with a p value<0.05.
A statistically significant relationship was observed between consecutive years when comparing each year to the preceding year (specifically, with the reference year 2023), with a p value<0.05.
Prevalence of CRE colonization upon admission
Among the cohort of 92 patients exhibiting Carbapenem- Resistant Enterobacteriaceae (CRE) colonization in either rectal swab samples upon hospital admission, the respective prevalence rates of CRE colonization upon admission for each year were 22.7%, 57.1%, 54.9%, and 46.8%. Furthermore, it was observed that a notable proportion of these patients had a documented history of CRE colonization or infection prior to their current admission (Figures 1-4).
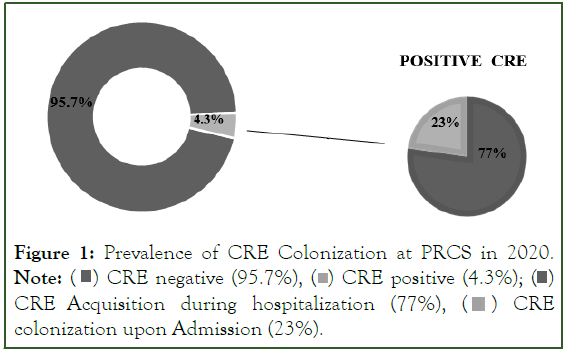
Figure 1: Prevalence of CRE Colonization at PRCS in 2020.
Note: 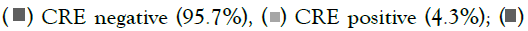 CRE Acquisition during hospitalization (77%),
CRE Acquisition during hospitalization (77%),  CRE colonization upon Admission (23%).
CRE colonization upon Admission (23%).
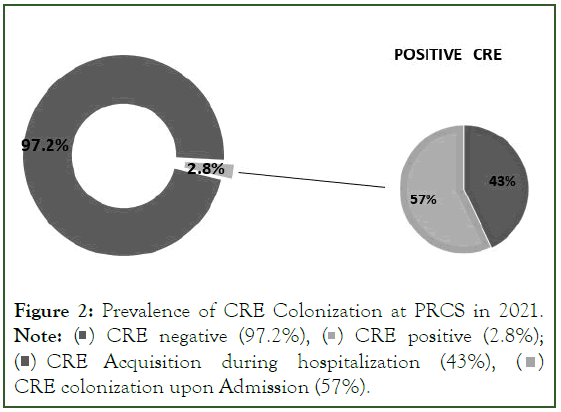
Figure 2: Prevalence of CRE Colonization at PRCS in 2021.
Note:  CRE positive (2.8%);
CRE positive (2.8%); 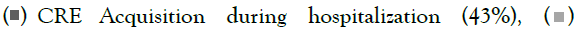 CRE colonization upon Admission (57%).
CRE colonization upon Admission (57%).
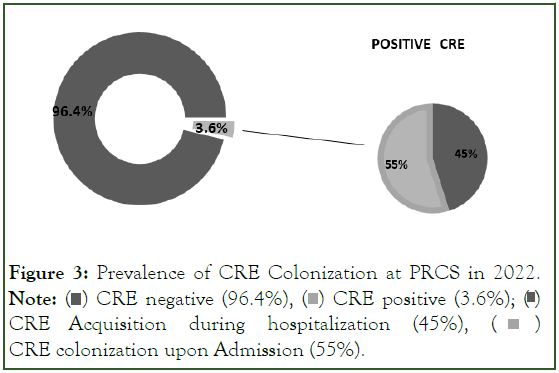
Figure 3: Prevalence of CRE Colonization at PRCS in 2022.
Note: 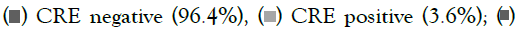 CRE Acquisition during hospitalization (45%),
CRE Acquisition during hospitalization (45%),  CRE colonization upon Admission (55%).
CRE colonization upon Admission (55%).
Figure 4: Prevalence of CRE Colonization at PRCS in 2023 (until 29/8/2023).
Note:  CRE positive (6.28%);
CRE positive (6.28%);  CRE Acquisition during hospitalization (53%),
CRE Acquisition during hospitalization (53%),  CRE colonization upon Admission (47%).
CRE colonization upon Admission (47%).
Acquisition of CRE during hospitalization
In our study cohort of 127 patients who initially tested negative for Carbapenem-Resistant Enterobacteriaceae (CRE) upon admission and underwent at least one follow-up stool or rectal swab test for CRE, we observed varying rates of CRE colonization over the years, which were 77.2%, 43.9%, 45.1%, and 53.2%, respectively. Furthermore, it was evident that a substantial number of these patients acquired CRE during the course of their hospitalization (Figures 1-4). Moreover, statistically significant differences (p value<0.05) were found in CRE colonization between cases upon admission and cases acquired CRE during hospitalization within each year.
Comparison of patients with positive CRE and Multidrug-Resistant bacteria (MDR) between patients who had colonization upon Admission vs. Acquisition during hospitalization
The data reveal that in 2022 and 2023, 56.5% and 76.0% of swabs, respectively, indicated the acquisition of Carbapenem- Resistant Enterobacteriaceae (CRE) during hospitalization. In the same years, 43.4% and 24.0% of swabs tested positive for Multidrug-Resistant (MDR) bacteria.
Moreover, our findings demonstrate that 54.9% of all detected positive patient swabs at the time of admission in 2022 lacked information regarding the specific nature of colonization, whether it was associated with enterobacterales or non-enterobacterales. Conversely, in 2023, 81.8% of swabs at admission were positive for CRE, while 18.1% of swabs indicated the presence of MDR organisms as shown in Table 1.
| Acquisition during hospitalization | 2022 | 2023 | |
| CRE positive | 56.50% | 76.00% | |
| MDR positive | 43.40% | 24.00% | |
| Upon Admission | CRE positive | 54.90% | 81.80% |
| MDR positive | 18.10% |
Table 1: Comparison of patients with positive CRE and Multidrug-Resistant Bacteria (MDR) between patients who had colonization upon Admission vs. Acquisition during hospitalization in 2022 and 2023.
Discussion
The findings of this research shed light on the evolving landscape of Carbapenem-Resistant Enterobacteriaceae (CRE) prevalence among patients admitted to Palestine Red Crescent Society Hospital in Hebron, Palestine, over the course of four consecutive years, from 2020 to 2023.
The data revealed noticeable variations in the prevalence rates of CRE colonization within each year. In 2020, 4.3% of the study population exhibited CRE colonization, which decreased to 2.8% in 2021, followed by an increase to 3.6% in 2022, and a significant spike to 6.28% in 2023.
Our findings demonstrated an annual variation, encompassing a range of 4.3% to 6.28%. This rate was comparable to the prevalence rates observed in the pooled prevalence of carbapenem-resistant K. pneumoniae colonization for the Asian continent, which is 4.56% [17]. However, our findings remained lower than the prevalence rates reported locally in the Gaza strip, Palestine (13.2%) [18]. On a global scale, we found higher prevalence rates in India (22%), China (21%), Egypt (19%), Jordan (41.2%), Spain (16%), and the USA (15%), while Japan had the lowest (0.13%) [17,19].
Such variations in CRE colonization rates may be indicative of changing epidemiological patterns, potentially influenced by factors such as patient demographics and infection control measures [20]. Variables including sample size, sample sources, study timing, utilized laboratory methodologies, and heightened risk faced by patients with longer stays are at higher risk due to prolonged antibiotic usage might contribute to the fluctuations in prevalence rates [12].
Many patients exhibited CRE colonization upon admission, with rates varying from 22.7% in 2020 to 57.1% in 2021, followed by 54.9% in 2022 and 46.8% in 2023, indicating recurrent colonization. Some patients acquired CRE during their hospital stay, with acquisition rates ranging from 43.9% in 2021 to 77.2% in 2020, 45.1% in 2022, and 53.2% in 2023, highlighting the persistent concern of nosocomial CRE acquisition [21].
An interesting observation from our study is the simultaneous detection of CRE and Multidrug-Resistant (MDR) bacteria in patient’s swabs. In 2022 and 2023, the data showed a higher proportion of swabs indicating the acquisition of CRE during hospitalization, compared to MDR bacteria. This could suggest that CRE may be more readily transmitted within the hospital setting during these years. Moreover, it is noteworthy that in 2022, a significant portion of positive patient swabs at admission lacked specific information regarding the nature of colonization. In contrast, in 2023, a higher percentage of swabs indicated CRE colonization upon admission.
The data underscores the importance of robust infection control measures, active surveillance, and early detection of CRE colonization to minimize the risk of nosocomial transmission within healthcare settings, especially for patients with a prior history of CRE colonization, as it reflects a shift in the epidemiological landscape with implications for patient care and infection control practices [22].
While the Red Crescent Hospital's infection statistics have been on the rise, they still lag behind other regions and hospitals. This can be attributed to the hospital's proactive approach in detecting, managing, and isolating infections to curb their spread, a testament to the effectiveness of their infection control policies.
However, it is important not to underestimate the role of hand hygiene, as inadequate hand hygiene among healthcare workers is a significant facilitator for CRE transmission within the hospital. This can subsequently lead to its spread through contaminated medical equipment, surfaces, and even clothing, thereby enabling patient-to-patient transmission. Additionally, the transfer of patients between different healthcare facilities can introduce CRE to new environments [23].
We faced certain limitations in this research. Firstly, incomplete registration in some years resulted in a lack of essential details, impacting the comprehensiveness of the data. Additionally, the microbiology lab's identification processes improved in recent years for detecting causative organisms and Multidrug-Resistant (MDR) bacteria, but this improvement was not consistently applied over the study period, potentially affecting data accuracy and comparability. Furthermore, there is a lack of hospital- specific statistics or percentages for CRE colonization. To address this, we hypothesized an annual prevalence of 2% in our statistical analysis. These limitations highlight the importance of standardizing data collection and laboratory practices in future research.
Conclusion
In conclusion, our study provides valuable insights into the prevalence, acquisition, and co-occurrence of CRE and MDR bacteria within the healthcare setting. These findings have implications for infection control and patient care strategies, and they underscore the importance of continuous monitoring and adaptation of practices to effectively manage and reduce CRE colonization and transmission in healthcare facilities. Further studies are needed to investigate the risk factors contributing to CRE transmission and to conduct genetic studies that illuminate the molecular basis of CRE resistance. These research initiatives are essential for refining infection control measures, developing targeted interventions, and effectively addressing the ongoing threat of CRE in healthcare settings.
Acknowledgment
We extend our gratitude to the Palestine Red Crescent Society Hospital in Hebron, Palestine, for their invaluable support and collaboration, which greatly contributed to the success of this research.
References
- Salam MA, Al-Amin MY, Salam MT, Pawar JS, Akhter N, Rabaan AA, et al. Antimicrobial resistance: A growing serious threat for global public health. Healthcare. 2023;11(13):1946.
[Crossref] [Google Scholar] [PubMed]
- Tompkins K, van Duin D. Treatment for carbapenem resistant Enterobacterales infections: Recent advances and future directions. Eur J Clin Microbiol Infect Dis. 2021;40(10):2053-2068.
[Crossref] [Google Scholar] [PubMed]
- Sabino S, Soares S, Ramos F, Moretti M, Zavascki AP, Rigatto MH. A cohort study of the impact of carbapenem-resistant Enterobacteriaceae infections on mortality of patients presenting with sepsis. MSphere. 2019;4(2):10-128.
[Crossref] [Google Scholar] [PubMed]
- Yun SJ, Kwon SM, Hur ES, Park SJ, Lee YH, Pyeon HS, et al. Outbreaks of Carbapenem Resistant Enterobacterales (CRE) According to the Type of Hospitals. Korean J Healthcare Assoc Infect Control Prev. 2022;27(2):162-167.
- Khawcharoenporn T, Laichuthai W. Subsequent Carbapenem Resistant Enterobacteriaceae (CRE)-associated infections among hospitalized patients with CRE colonization: Impact of antibiotic use and other factors. Infect Control Hosp Epidemiol. 2020;41(9):1084-1089.
[Crossref] [Google Scholar] [PubMed]
- Goodman KE, Simner PJ, Klein EY, Kazmi AQ, Gadala A, Rock C, et al. How frequently are hospitalized patients colonized with Carbapenem Resistant Enterobacteriaceae (CRE) already on contact precautions for other indications? Infect Control Hosp Epidemiol. 2018;39(12):1491-1493.
[Crossref] [Google Scholar] [PubMed]
- Hansen GT. Continuous evolution: Perspective on the epidemiology of carbapenemase resistance among Enterobacterales and other Gram-negative bacteria. Infect Dis Ther. 2021;10:75-92.
[Crossref] [Google Scholar] [PubMed]
- Lavagnoli LS, Bassetti BR, Kaiser TD, Kutz KM, Cerutti C. Factors associated with acquisition of carbapenem-resistant Enterobacteriaceae1. Rev Lat Am Enfermagem. 2017;25.
[Crossref] [Google Scholar] [PubMed]
- Hayden ZS, Kendall B. Carbapenem Resistant Enterobacteriaceae. 2023.
[PubMed]
- Nordmann P, Dortet L, Poirel L. Carbapenem resistance in Enterobacteriaceae: Here is the storm! Trends Mol Med. 2012;18(5):263-272.
[Crossref] [Google Scholar] [PubMed]
- Chen X, Wen X, Jiang Z, Yan Q. Prevalence and factors associated with Carbapenem Resistant Enterobacterales (CRE) infection among hematological malignancies patients with CRE intestinal colonization. Ann Clin Microbiol Antimicrob. 2023;22(1):1-10.
[Crossref] [Google Scholar] [PubMed]
- Wangchinda W, Thamlikitkul V, Watcharasuwanseree S, Tangkoskul T. Active surveillance for Carbapenem Resistant Enterobacterales (CRE) colonization and clinical course of CRE colonization among hospitalized patients at a University Hospital in Thailand. Antibiotics. 2022;11(10):1401.
[Crossref] [Google Scholar] [PubMed]
- Adler A, Solter E, Masarwa S, Miller-Roll T, Abu-Libdeh B, Khammash H, et al. Epidemiological and microbiological characteristics of an outbreak caused by OXA-48-producing Enterobacteriaceae in a neonatal intensive care unit in Jerusalem, Israel. J Clin Microbiol. 2013;51(9):2926-2930.
[Crossref] [Google Scholar] [PubMed]
- Ita T, Luvsansharav UO, Smith RM, Mugoh R, Ayodo C, Oduor B, et al. Prevalence of colonization with multidrug-resistant bacteria in communities and hospitals in Kenya. Sci Rep. 2022;12(1):22290.
[Crossref] [Google Scholar] [PubMed]
- Korach-Rechtman H, Hreish M, Fried C, Gerassy-Vainberg S, Azzam ZS, Kashi Y, et al. Intestinal dysbiosis in carriers of carbapenem-resistant Enterobacteriaceae. mSphere. 2020;5(2):173.
[Crossref] [Google Scholar] [PubMed]
- Nordmann P, Naas T, Poirel L. Global spread of carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis. 2011;17(10):1791.
[Crossref] [Google Scholar] [PubMed]
- Tesfa T, Mitiku H, Edae M, Assefa N. Prevalence and incidence of carbapenem-resistant K. pneumoniae colonization: Systematic review and meta-analysis. Syst Rev. 2022;11(1):1-5.
[Crossref] [Google Scholar] [PubMed]
- Rida RH, Al Laham NA, Elmanama AA. Carbapenem resistance among clinical and environmental Gram-negative isolates recovered from hospitals in Gaza strip, Palestine. Germs. 2018;8(3):147.
[Crossref] [Google Scholar] [PubMed]
- Hammour KA, Abu-Farha R, Itani R, Karout S, Allan A, Manaseer Q, et al. the prevalence of carbapenem resistance gram negative pathogens in a tertiary teaching hospital in jordan. BMC Infect Dis. 2023;23(1):634.
[Crossref] [Google Scholar] [PubMed]
- Poole K, George R, Decraene V, Shankar K, Cawthorne J, Savage N, et al. Active case finding for carbapenemase producing Enterobacteriaceae in a teaching hospital: Prevalence and risk factors for colonization. J Hosp Infect. 2016;94(2):125-129.
[Crossref] [Google Scholar] [PubMed]
- Shibabaw A, Sahle Z, Metaferia Y, Atlaw A, Adenew B, Gedefie A, et al. Epidemiology and prevention of hospital-acquired carbapenem resistant Enterobacterales infection in hospitalized patients, Northeast Ethiopia. IJID Reg. 2023;7:77-83.
[Crossref] [Google Scholar] [PubMed]
- Gomides MD, Fontes AM, Silveira AO, Matoso DC, Ferreira AL, Sadoyama G. The importance of active surveillance of Carbapenem Resistant Enterobacterales (CRE) in colonization rates in critically ill patients. PLoS One. 2022;17(1):e0262554.
[Crossref] [Google Scholar] [PubMed]
- Thaden JT, Lewis SS, Hazen KC, Huslage K, Fowler VG, Moehring RW, et al. Rising rates of carbapenem-resistant enterobacteriaceae in community hospitals: a mixed-methods review of epidemiology and microbiology practices in a network of community hospitals in the southeastern United States. Infect Control Hosp Epidemiol. 2014;35(8):978-983.
[Crossref] [Google Scholar] [PubMed]
Citation: Dofesh AM (2023) Prevalence of Carbapenem-Resistant Enterobacteriaceae (CRE) Among Patients Admitted to Palestine Red Crescent Society Hospital in Hebron, Palestine. Clin Microbiol. 12:370.
Copyright: © 2023 Dofesh AM. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
