Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
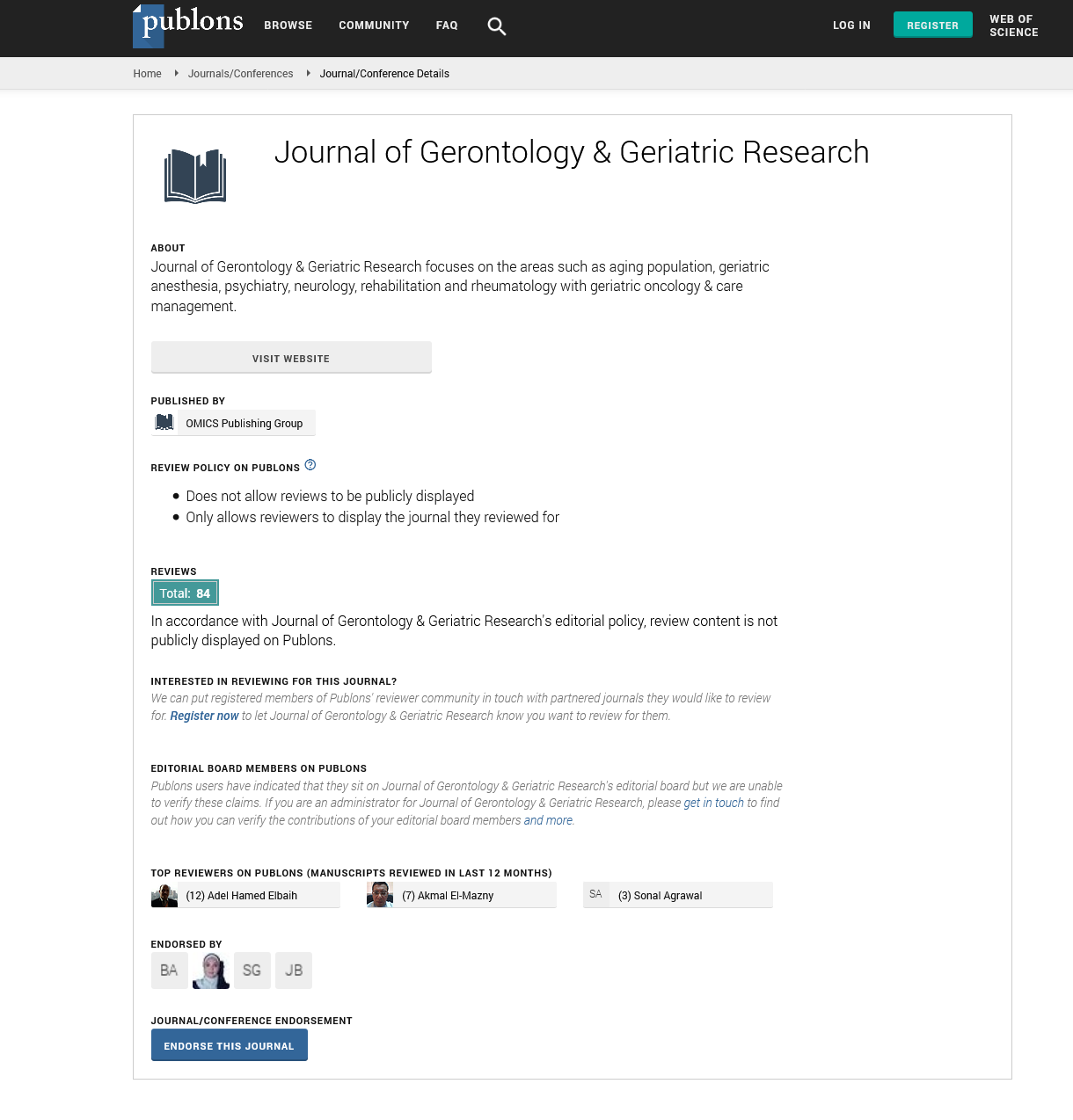
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2022) Volume 11, Issue 5
Geriatric Diabetes Guideline Development
Tania Kalsi*Received: 05-May-2022, Manuscript No. jggr-22-17193; Editor assigned: 07-May-2022, Pre QC No. P-17193; Reviewed: 20-May-2022, QC No. Q-17193; Revised: 25-May-2022, Manuscript No. R-17193; Published: 30-May-2022, DOI: 10.35248/2167-7182.2022.11.612
Introduction
In newly diagnosed diabetes patients aged 65 and older, we recommend that an endocrinologist or diabetes care expert collaborate with the primary care provider, a multidisciplinary team, and the patient to set tailored diabetes management goals. If the patient has type 1 diabetes, requires sophisticated hyperglycaemia treatment to reach treatment goals, has recurrent severe hypoglycaemia, or has many diabetic complications, an endocrinologist or diabetes care specialist should be the primary care provider. Technical note: Because of comorbidities that can influence the longevity of red blood cells in the circulation, HbA1c measurements in this age range may be erroneous. Although the best screening frequency for patients who have a normal initial screening test is unknown, the writing committee recommends repeat screening every two years after that. The decision of diabetes and prediabetes screening for an individual patient, like any other health screening, is based on whether or not action will be taken as a result of the screening and the possibility of benefit. For an elderly patient with end-stage cancer or organ system failure, for example, such screening may not be suitable. In these cases, it's best to make decisions along with the patient [1].
Diabetes is a serious health problem that affects the elderly. Onequarter of people over 65 have diabetes, and half of older adults have prediabetes and the number of older adults living with these disorders is predicted to rise dramatically in the future decades. The medical, psychological, functional, and social dimensions of diabetes management in older persons must be assessed on a regular basis. Premature death, functional disability, accelerated muscle loss, and comorbid disorders, such as hypertension, coronary heart disease, and stroke, are all more common in older persons with diabetes than in those without. Screening for diabetic problems in older persons should be tailored to the individual and repeated on a regular basis, as the results of screening tests may influence therapeutic aims and approaches [2].
Description
This recommendation is most appropriate for high-risk patients who have one or more of the following characteristics: obesity, diabetes in a first-degree relative, high-risk race/ethnicity (e.g., African American, Latino, Native American, Asian American, Pacific Islander), history of cardiovascular disease, hypertension (140/90 mm Hg or on hypertension therapy), high-density lipoprotein cholesterol level 35 mg/dL (0.90 mmol/L), and/or When doing this operation on frail elderly people or those who may find it too taxing, shared decision-making is recommended. For an oral glucose tolerance test, standard food preparation is recommended. The physical, functional, and cognitive state of older persons with diabetes is diverse, necessitating thorough individualization of their treatment regimes. However, there is no evidence-based guidance in the absence of specific information from therapeutic studies involving older persons with different characteristics, which is a significant drawback of current care techniques. It's vital to remember that the profiles of older adults with diabetes can vary depending on their age, functional health, frailty, and comorbidity profiles. Furthermore, all older adults with diabetes, ranging from healthy individuals to those staying in care facilities with a short life expectancy, those requiring palliative care, and those requiring end-of-life management, require a tailored approach to care. Our diverse team of professionals describes in this Review [3].
Cognitive impairment in older persons with diabetes should be carefully tested and managed. Several simple assessment tools, such as the Mini Mental State Examination, Mini-Cog and the Montreal Cognitive Assessment are available to screen for cognitive impairment and may help to identify patients who require neuropsychological evaluation, particularly those with dementia suspicion (i.e., experiencing memory loss and decline in their basic and instrumental activities of daily living). Adults 65 years and older should have an annual screening to detect moderate cognitive impairment or dementia early. When a patient's clinical status has deteriorated significantly due to increased difficulty with self-care duties, such as errors in medication administration, a screening for cognitive impairment may be undertaken [4,5].
Conclusion
Diabetes management in older persons is difficult since there is such a wide range of clinical presentation, psychosocial environment, and resource availability in this population. Both glycaemic goals and diabetes management can be influenced by a person's living situation and the level of accessible social support. Diabetes management varies depending on where old patients reside (i.e., whether they live in the community, in an assisted-living facility, or in a nursing home) the characteristics of older persons in various living settings, as well as how these traits may influence diabetes care. People who test positive for cognitive impairment should be evaluated further, including referred to a behavioural health practitioner for a thorough cognitive/neuropsychological evaluation.
REFERENCES
- Abbatecola AM, Antonelli-Incalzi R. COVID-19 spiraling of frailty in older Italian patients. J Nutrition Health Aging. 2020;24:453-455.
- Andersen KG. The proximal origin of SARS-CoV-2. Nat Med. 2020;26:450-452.
- Arentz M. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323:1612-1614.
- Chhetri JK. Prevention of COVID-19 in older adults: A brief guidance from the International Association for Gerontology and Geriatrics (IAGG) Asia/Oceania region. J Nutr Health Aging. 2020;24:471-472.
- Herzallah HK. Temporal trends in the incidence and demographics of cancers, communicable diseases, and non-communicable diseases in Saudi Arabia over the last decade. Saudi Med J. 2019;40:277.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Citation: Kalsi T (2022) Geriatric Diabetes Guideline Development. J Gerontol Geriatr Res. 11:612.
Copyright: © 2022 Kalsi T. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.