Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
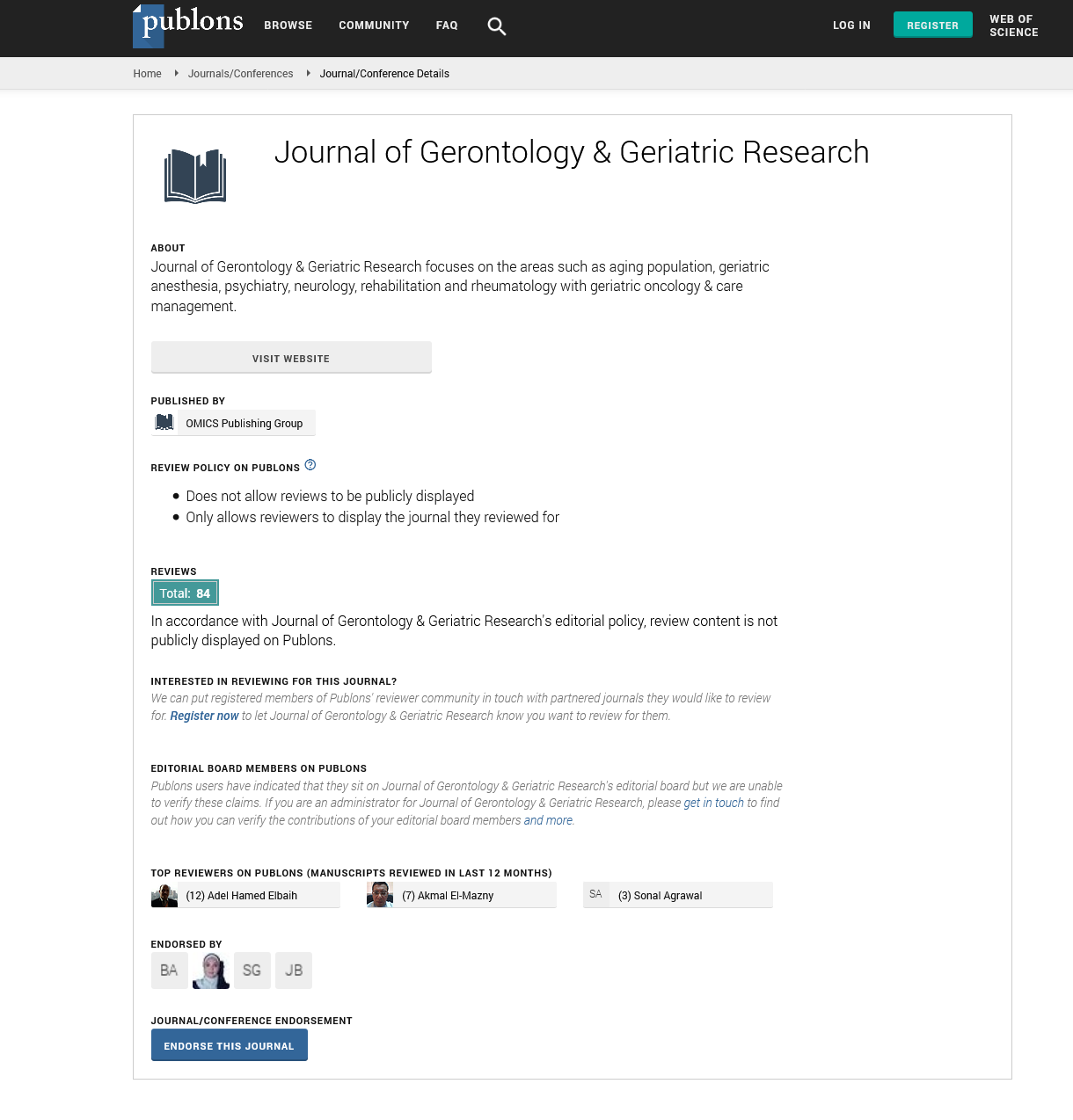
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 12, Issue 2
Falling Down the Slippery Slope of Anticoagulation in Older Adults (>80): More Than Meets the Eye
Vatche Melkonian1, Mackenzie Mayhew2, Rachele J Solomon3, Adilia Ortega3, Shari Selesky3, Bradley Rogers3, Brenda Shaver3, Candace Pineda3, Chauniqua Kiffin3, Ibrahim I Jabbour3, Sara Hennessy4, Juan D Arenas2,3, Eddy H Carrillo3, Andrew A Rosenthal3 and Tjasa Hranjec2,3*2Department of Surgery, Florida Internation University, Herbert Wertheim College of Medicine, Miami, FL, USA
3Department of Surgery, Memorial Regional Hospital, Hollywood, FL, USA
4Department of Surgery, University of Texas Southwesterm Medical Center, Dallas, TX, USA
Received: 23-Sep-2022, Manuscript No. JGGR-22-18153; Editor assigned: 25-Sep-2022, Pre QC No. P-18153; Reviewed: 30-Sep-2022, QC No. Q-18153; Revised: 14-Mar-2023, Manuscript No. R-18153; Published: 22-Mar-2023, DOI: 10.35248/2167-7182.23.11.661
Abstract
Background: Although fall risk increases with age, many patients remain anticoagulated (AC) indefinitely, regardless of mental or physical frailty. We hypothesized that in patients >80 years, risk of anticoagulation outweighs its benefits.
Methods: Retrospective chart review was conducted to identify older patients (>80), who have fallen from standing/ sitting, at a single level-one trauma center. Patients on and off AC were compared for demographics, injury patterns, length of stay, and long-and short-term outcomes. Data was analyzed using univariate and multivariate (MV) analyses.
Results: A total of 465 patients with mean age 87.7±0.2 (range of 80-105) were evaluated over a 10-month period, following a fall. Nearly 65% of the patients (n=300) were receiving some type of anticoagulation: aspirin and warfarin were the most frequently used. Most injuries were minor: painful extremity hematomas, lacerations, or fractures. Although 76% (n=364) of the patients were admitted from home, 30% were discharged to a skilled nursing facility. Extremity fractures were less common in AC patients; however, AC patients were more likely to bleed after a serious injury, require ICU admission and transfusion. Incidence of intracranial hemorrhage was similar between the two groups, although head injuries were more common in AC patients. The most severe (in-hospital) outcomes were seen in AC patients: five required tracheostomies and five died (p=0.0955). Short- (<90-day) and long-term (two-year) mortality was equivalent between the two groups; long-term, 35% of all patients died following a fall. MV analysis revealed that chronic medical conditions, rather than anticoagulants correlated with two-year mortality.
Conclusion: A fall from standing may foreshadow patient’s worsening physical or mental condition regardless of the cause of fall or anticoagulation status. In discharged patients, AC does not seem to contribute directly to patient demise. Instead, fall should become a marker of disease severity and patient frailty.
Keywords
Anticoagulation in Older Adults; Falls in older adults; Falls and Anticoagulation in older adults; Falls in Elderly
Introduction
Older adults falling on anticoagulation
According to the National Council on Aging (NCOA), falls are the leading cause of fatal injury, and the most common cause of nonfatal trauma-related hospital admissions among older adults. The NCOA reports that one in four Americans over 65 will fall annually, resulting in more than 3 million injuries treated in the Emergency Department (ED), with more than 800,000 hospitalizations [1]. For those living in long-term institutions, 30- 50% suffers a single fall, while 40% experience recurrent falls [2,3]. Approximately 30-40% of community-dwelling adults over 65 years of age fall, with 50% sustaining an injury [2]. More serious injuries are noted especially in patients over 80, imposing a significant social and financial burden for fall-related hospitalizations. In fact, patients 85 and older have the highest fall fatality rate - 106 per 100,000 in women and 153 per 100,000 in men [4]. An estimated $50 billion per year is spent on medical costs related to non-fatal fall injuries, while $754 million is spent on fatal falls [1].
Falls are a result of both intrinsic and extrinsic risk factors, such as race, socioeconomic status, age, gender, medical and physical conditions (e.g. neuropathy, mobility impairment), and behavioral factors (e.g. sedentary lifestyle, alcohol misuse) [3]. Seemingly simple tasks like standing become difficult in balance-impaired older adults. They may show higher levels of sway, especially when performing a secondary cognitive task. During locomotion, balance control requirements may be even higher, given that the body’s center of mass is already in motion, with momentum that must be maintained or slowed in order to prevent a fall [5].
Physicians are faced with the difficult task of providing appropriate care to older patients by balancing their social, emotional, and physiologic factors in a setting of increasingly complex and numerous medical problems. Anticoagulation for the prevention of thromboemboli secondary to atrial fibrillation (afib) is one of the more difficult therapeutic decisions; it is often juxtaposed against the risk of falling, which in turn may cause additional injuries and have devastating effects in aging and frail patients [3].
Although there is some data to support the use of anticoagulants in prevention and treatment of patients following embolic/ thrombotic events – cardiac, neurologic, or vascular – only a few publications address the association between anticoagulation and short- or long-term outcomes following a fall in older adults (> 80 years of age). We hypothesized that anticoagulated (AC) older patients would have worse outcomes following a fall and would suffer more significant injuries and increased bleeding.
Materials and Methods
Patient population and data collection
A retrospective chart review was conducted of older (>80 years of age) patients, presenting to the ED, at a single level-one trauma center (Memorial Regional Hospital, Hollywood, Florida), following a fall between April 2016 and January 2017. Only 1.5% of the patients reported falling from a height (ladder or stool), the rest fell from standing, sitting (wheelchair), or supine (bed) positions. No patients were excluded and complete two-year follow up data was available. The Memorial Healthcare System Institutional Review Board approved the study with a waiver of consent.
All study subjects underwent a standard trauma evaluation with appropriate imaging. Upon arrival to the ED, patients were seen, evaluated, and treated by the ED staff including physicians, nurses, respiratory therapists, and pharmacists. Patients received basic x-rays of chest, pelvis, or injured extremities. Computer tomography (CT) scans and expert consultation from trauma, neurosurgery, and orthopaedic sub-specialists was based on sustained injuries and their severity. Hemodynamically unstable patients were treated (e.g. intubated, transfused) before proceeding to imaging or surgery. Injured patients were either admitted to the intensive care unit (ICU) or floor, while minimally injured were discharged upon evaluation by ED social workers. Patients were considered to be anticoagulated if they were receiving anti-factor (e.g. warfarin, apixaban) and/or anti-platelet (e.g. aspirin, clopidogrel) medications regardless of dosing or level of anticoagulation. Of note, only one patient received anti-factor medications other than warfarin, rivaroxaban, or enoxaparin.
Baseline demographics, date and location of hospital admission and discharge, co-morbidities, treatment with anticoagulants, need for transfusion or mechanical ventilation, site of traumatic injury, in- and out-of-hospital complications, including short (in-hospital, <30, <90 day) and long-term mortality (90 days – 2 years), were entered into a secure, password-protected computer database. Patients marked as ‘moribund’ on discharge, were either deceased or discharged to hospice with expected short-term mortality, although not everyone died within 30 days post discharge. Of note, <30 and <90-day mortality included patients who died in the hospital. Two years of long-term follow-up was used to evaluate re-admission and mortality, including deaths from any cause occurring prior to or following hospital discharge. When our electronic medical records (EMR) were insufficient, phone calls were made to home/ institutions in order to acquire complete long-term data.
Statistical analysis
Univariate statistical analysis was used to compare patients with and without anticoagulation following a fall, with statistical significance set to <0.05. Continuous variables were presented as a mean ± standard error (SE) and compared using a two-sample t-test for independent samples. Non-parametric testing using Mann Whitney U test compared medians. Categorical variables were analyzed using a Chi-square or Fisher’s exact test. Multivariate logistic regression analysis was performed to identify independent risk factors of short- and long-term mortality following a fall using covariates (e.g. AC) that were chosen a priori for clinical importance. Patients who died within 90 days were considered to have shortterm mortality, while those who died after 90 days, were placed in the category of long-term mortality. All statistical analyses were performed using SAS software, version 9.4 (SAS Institute, Cary, North Carolina).
Results
Demographics: A total of 465 patients (>80 years old) were evaluated following a fall from standing over a 10-month period. The majority of the patients in the study was Caucasian, female, and admitted from home (Table 1). Approximately two-thirds of the patients were older than 85 and 35% were over 90. Nearly all were admitted with an impaired gait requiring a cane, walker, or wheelchair for mobility, and about 40% of the patients sustained a fall previously (Table 1). Medical history of patients receiving AC was more extensive, with significant differences in cardiac, vascular, and neurologic disorders. Patients receiving no AC were more likely to have a malignancy (Table 1).
| Anticoagulation (N=300) n% | No Anticoagulation (N=165) n% | p-value | |||
|---|---|---|---|---|---|
| Age | |||||
| Mean+SE | 87.8±0.3 | - | 87.6±0.3 | - | 0.7120 |
| Median (IQR) | 87 (84,92) | - | 87 (84,91) | - | 0.7461 |
| Patients over age 85 | 200 | 66.7 | 114 | 69.1 | 0.5932 |
| Patients over age 90 | 107 | 35.7 | 54 | 32.7 | 0.5238 |
| Gender | |||||
| Male | 93 | 31.0 | 46 | 27.9 | 0.4818 |
| Race | |||||
| Caucasian | 208 | 69.3 | 114 | 69.1 | 0.2245 |
| African American | 21 | 7.0 | 8 | 4.9 | |
| Hispanic | 16 | 5.3 | 4 | 2.4 | |
| Other | 55 | 18.3 | 39 | 23.6 | |
| Medical History | |||||
| Coronary Artery Disease | 112 | 37.3 | 18 | 10.9 | <0.0001* |
| Congestive Heart Failure | 50 | 16.7 | 13 | 7.9 | 0.0081* |
| Myocardial Infarction | 43 | 14.3 | 9 | 5.5 | 0.0037* |
| Coronary Revascularization | 29 | 9.7 | 3 | 1.8 | 0.0014* |
| Hypertension | 263 | 87.7 | 112 | 67.9 | <0.0001* |
| Peripheral Vascular Disease | 27 | 9.0 | 5 | 3.0 | 0.0150* |
| Arrhythmia | 130 | 43.3 | 26 | 15.8 | <0.0001* |
| Deep Vein Thrombosis | 21 | 7.0 | 4 | 2.4 | 0.0363* |
| Pulmonary Embolism | 6 | 2.0 | 1 | 0.6 | 0.2376 |
| TIA/CVA | 81 | 27.0 | 20 | 12.1 | 0.0002 |
| Dementia | 89 | 29.7 | 44 | 26.7 | 0.4934 |
| Malignancy | 20 | 6.7 | 22 | 13.3 | 0.0164 |
| Cirrhosis/Ascites | 0 | 0.0 | 0 | 0.0 | n/a |
| Hemodialysis | 3 | 1.0 | 0 | 0.0 | 0.1975 |
| Steroids | 4 | 1.3 | 2 | 1.2 | 0.9118 |
| Inflammatory Bowel Disease | 0 | 0.0 | 2 | 1.2 | 0.0560* |
| Renal Insufficiency | 37 | 12.3 | 15 | 9.1 | 0.2885 |
| Mobility Impaired Gait |
229 | 76.6 | 128 | 77.6 | 0.8091 |
| Previous Fall | 129 | 43.0 | 72 | 43.6 | 0.8946 |
| Admission Location | |||||
| Home | 229 | 76.3 | 125 | 75.8 | 0.3976 |
| Skilled Nursing Facility | 19 | 6.3 | 7 | 4.2 | |
| Assisted Living Facility | 29 | 9.7 | 23 | 13.9 | |
| Other | 23 | 7.7 | 10 | 6.1 | |
SE = standard error, IQR = interquartile range, TIA = transient ischemic attack, CVA = cerebrovascular accident
Table 1: Demographics (Pre-Fall).
Injuries: Most patients sustained minor injuries requiring a mean hospital stay of 4.4±0.2 days (range 0-53) for painful extremity hematomas, lacerations, or bony fractures (Table 2). Head was the most frequently injured site, especially in AC patients. Intracranial hemorrhage (ICH) was detected in 69 (14.8%) patients overall and was noted to be similar between AC and non-AC groups (Table 2). Risk of bleeding from any source (e.g. lacerations, fractures) excluding head after a fall was significantly increased in AC group as compared to non-AC group (96 (32.1%) vs. 34 (20.6%), p=0.0083). Meanwhile, extremity injuries (mainly fractures), were more frequent in non-AC patients (Table 2).
| Anticoagulation (N=300) n% | No Anticoagulation (N=165) n% | p-value | |||
|---|---|---|---|---|---|
| Head Injury | 183 | 61.0 | 65 | 39.4 | <0.0001* |
| Head AIS > 4 | 20 | 6.7 | 10 | 6.1 | 0.7991 |
| ICH on Presentation | 46 | 15.3 | 23 | 13.9 | 0.6858 |
| Subdural hemorrhage | 22 | 7.3 | 10 | 6.1 | 0.6039 |
| Subarachnoid hemorrhage | 8 | 2.7 | 4 | 2.4 | 0.8747 |
| Epidural hemorrhage | 0 | 0.0 | 0 | 0.0 | n/a |
| IVH hemorrhage | 0 | 0.0 | 2 | 1.2 | 0.0560* |
| Multiple hemorrhages | 16 | 5.3 | 7 | 4.2 | 0.6037 |
| Craniotomy | 3 | 1.0 | 0 | 0.0 | 0.1975 |
| Chest Injury | 28 | 9.3 | 14 | 8.3 | 0.7601 |
| Rib Fractures | 22 | 7.3 | 1 | 6.7 | 0.7888 |
| Hemothorax | 4 | 1.3 | 2 | 1.2 | 0.9118 |
| Pneumothorax | 6 | 2.0 | 2 | 1.2 | 0.5319 |
| Thoracostomy tube | 4 | 1.3 | 2 | 1.2 | 0.9118 |
| Abdominal Injury | 0 | 0.0 | 1 | 0.6 | 0.1771 |
| Pelvic Injury | 13 | 4.3 | 10 | 6.1 | 0.4111 |
| Pelvic Surgery | 0 | 0.0 | 1 | 0.6 | 0.1771 |
| Extremity Injuries | 133 | 44.3 | 112 | 67.9 | <0.0001* |
| Extremity Fractures | 119 | 39.7 | 112 | 67.9 | <0.0001* |
| Extremity Surgery | 72 | 47.7 | 71 | 55.5 | 0.1948 |
AIS = abbreviated injury score, ICH = intracranial hemorrhage, IVH = intraventricular hemorrhage
Table 2: Distribution of Injuries following a Fall in Elderly.
Anticoagulation: Almost 65% of the patients (n=300) were receiving some type of AC; 43% were over 85 years of age, and 23% of patients over 90. Antiplatelet agents (n=215) and warfarin (n=76) were the most frequently used. Of the AC medications, aspirin was the most frequently prescribed (n=176), both as a mono-therapy as well as in conjunction with other AC agents. Most common reasons for AC were arrhythmias (atrial fibrillation), followed by coronary artery disease (CAD), stroke, or clotting disorder. Almost 5% of AC patients presented with supra-therapeutic International Normalized Ratio (INR) ranging from 3 to 7.5. Of note, many patients were discharged on AC and several started AC anew post fall.
Short-term outcomes: Patients, who were considered therapeutic (INR >2) or supratherapeutic (INR >3) on warfarin, were more likely to be admitted to the ICU (p=0.0291), with a 43% increased risk of death (RR = 1.43, CI 1.02 – 2.02). Patients in the AC group were more likely to receive transfusion of platelets and fresh frozen plasma (FFP) for the correction of medication-induced coagulopathy in an attempt to prevent further bleeding (Table 3). Among AC patients, no increased intracranial bleeding was seen in those treated with antiplatelet versus anti-factor agents. The most severely injured patients, requiring the highest level of intervention were patients in the AC group: five required tracheostomies, including two patients over 90, while five AC patients died following a fall (p=0.0955) (Table 3). For the patients with poor outcomes - death or discharge to hospice-13 (44.8%) were receiving anti-factor treatment and 16 anti-platelet (55.2%). Of the patients with in-hospital mortality, 4 (80%) received anti-factor reversal and 1 (20%) anti-platelet therapy.
| Anticoagulation (N=300) n% | No Anticoagulation (N=165) n% | p-value | |||
|---|---|---|---|---|---|
| Hospital LOS | |||||
| Mean+SE | 5.7±1.3 | 4.3±0.4 | 0.4190 | ||
| Median (IQR) | 3 (1,6) | 3 (2,5) | 0.4273 | ||
| ICU Admission (n=10) | 77 | 25.8 | 28 | 16.9 | 0.0291* |
| ICU LOS | |||||
| Mean+SE | 4.1±0.5 | 2.9±0.5 | 0.1091 | ||
| Median (IQR) | 3 (2,5) | 2 (1,4) | 0.1682 | ||
| Transfusion (all) | 81 | 27.0 | 36 | 21.8 | 0.2179 |
| Within first 24 hours | 71 | 23.7 | 32 | 19.4 | 0.2884 |
| Red Blood Cells | 62 | 20.7 | 36 | 21.8 | 0.7708 |
| Platelets | 14 | 4.7 | 1 | 0.6 | 0.0177* |
| Fresh Frozen Plasma | 19 | 6.4 | 0 | 0.0 | 0.0003* |
| Other Intervention | |||||
| Tracheostomy | 5 | 1.7 | 0 | 0.0 | 0.0955* |
| Peg Tube | 3 | 1.0 | 1 | 0.6 | 0.6598 |
| Discharge Disposition | |||||
| Worset (Death/Hospice/SNF) | 109 | 36.5 | 75 | 45.7 | 0.0511* |
| Home/Rehab | 179 | 59.7 | 86 | 52.1 | 0.1158 |
| Skilled Nursing Facility | 82 | 27.4 | 65 | 39.6 | 0.0074* |
| Assisted Living Facility | 11 | 3.7 | 3 | 1.8 | 0.2644 |
| Short-term mortality (<90 days) | 44 | 14.7 | 20 | 12.1 | 0.4459 |
| In-hospital Mortality | 5 | 1.7 | 0 | 0.0 | 0.0955* |
| Mortality (<30 days) | 26 | 8.7 | 10 | 6.1 | 0.2539 |
| Long-term Mortality (all) | 114 | 38.0 | 49 | 29.7 | 0.0726* |
| Discharge on Anticoagulation | 207 | 69.0 | 44 | 26.7 | <0.0001* |
| Readmission | |||||
| Re-CVA (all) | 22 | 7.3 | 6 | 3.6 | 0.1088 |
| Re-CVA (bleed) | 14 | 4.7 | 7 | 4.2 | 0.8331 |
| New thrombus (PE/DVT) | 5 | 1.7 | 4 | 2.4 | 0.5705 |
| Readmit for fall within 1 year | 90 | 30.0 | 43 | 26.1 | 0.3684 |
*Indicates statistical significance at α = 0.05
SE = standard error, IQR = interquartile range, SNF = skilled nursing facility, CVA = cerebrovascular accident, PE = pulmonary embolus. DVT = deep venous thrombosis
Table 3: Outcomes (Post-Fall).
Approximately 40% of all patients required a discharge to skilled nursing (SNF) or assisted living facility even after being admitted from home; surprisingly, more patients in the non-AC group were discharged to SNF (RR=1.23, CI 1.1-1.4) following a fall (Table 4). No in-hospital mortality was reported in the non-AC group and no statistically significant differences were seen in the 30- and 90-day mortality between the two groups. About half of the AC patients, who died within 30 days, were on anti-factor treatment, and half were receiving anti-platelet medications at home. Only two patients with 30-day mortality were receiving both anticoagulants on admission.
| OR | Wald χ2 | p-value | 95% CI | |
|---|---|---|---|---|
| Gender (F vs. M) | 1.06 | 0.0 | 0.8643 | 0.5 - 2.1 |
| Age | ||||
| 85-90 vs <85 | 0.61 | 2.8 | 0.0946 | 0.3 - 1.4 |
| ≥90 vs <85 | 1.26 | 2.2 | 0.1399 | 0.6 - 2.6 |
| Race | ||||
| AA vs. Caucasian | 0.52 | 0.5 | 0.4894 | 0.1 - 2.0 |
| Hispanic vs. Caucasian | 0.45 | 1.7 | 0.1937 | 0.2 - 1.1 |
| Other vs. Caucasian | 1.40 | 1.3 | 0.2626 | 0.4 - 5.6 |
| Impaired gait | 2.45 | 3.5 | 0.0608* | 0.96 - 6.3 |
| Dementia | 1.17 | 0.2 | 0.6443 | 0.6 - 2.3 |
| AC on admission | 0.85 | 0.2 | 0.6274 | 0.4 - 1.7 |
| Supra/Therapeutic INR | 1.00 | 0.0 | 0.9952 | 0.3 - 2.9 |
| Transfusion | 2.04 | 4.7 | 0.0304* | 1.1 - 3.9 |
| Severe head injury | 3.16 | 8.0 | 0.0048* | 1.4 - 7.0 |
| Mechanical ventilation | 30.40 | 20.8 | <0.0001* | 7 - 131.7 |
| Previous fall | 0.69 | 1.3 | 0.2486 | 0.4 - 1.3 |
| Congestive heart failure& | 2.40 | 4.9 | 0.0270* | 1.1 - 5.1 |
| TIA/CVA& | 1.64 | 1.8 | 0.1809 | 0.8 - 3.4 |
| Myocardial infarction& | 0.62 | 0.8 | 0.3633 | 0.2 - 1.7 |
| Admit from SNF | 3.88 | 7.5 | 0.0062* | 1.5 - 10.3 |
& Indicates patient’s medical history
OR = odds ratio, CI = confidence interval, AA = African American; AC = anticoagulation, Supra = surpratherapeutic, TIA = transient ischemic attack, CVA = cerebrovascular accident, SNF = Skilled nursing facility
Table 4: Multivariate Analysis of Short-Term Mortality.
Long-term outcomes: Approximately 33% of the patients were readmitted after a fall within one year following discharge. Readmissions for new hemorrhagic or ischemic strokes were not statistically different between the groups. Altogether, 163 (40.6%) patients died within two years: mortality was higher in AC group (114 (38%) vs. 49 (29.7%), p=0.0726). A large portion of patients, who eventually died, were discharged on anticoagulants: 7 (11.1%) out of 34 moribund patients (excluding five patients who died in the hospital), 60 (60.6%) out of 99 patients who died past 90 days, and 85 (52.1%) out of total 163 patients who died within two years.
The difference in mortality between AC and non-AC groups disappeared once patients with initial grave injuries following fall, were excluded. That is, in patients who survived to discharge, short-term (30 or 90 days) mortality was similar regardless of anticoagulation.
Multivariate analysis: Multivariate logistic regression modeling was used to estimate short- and long-term risk of death adjusted for covariates. The 90-day model evaluated short-term mortality with a c-statistic of 0.77 and a good ability to discriminate between survivors and decedents (Max R2 = 0.2672) (Table 4). The largest contributors to mortality were need for mechanical ventilation, which carried a 30-fold increased risk of death (Table 4), followed by presence of severe head injury, admission from SNF, history of congestive heart failure (CHF), need for transfusion, and impaired gait. Interestingly, presence of AC on admission was not a significant contributor to mortality when adjusted for covariates. Long-term model (>90 days) was also able to discriminate between survivors and decedents well (Max R2 = 0.2185) with a c-statistic of 0.75 (Table 5). The most important contributors to mortality were CHF, followed by impaired gait, dementia, age (>85), and severe head injury, while Hispanic race was found to be protective. Presence of AC was not a contributing factor to long-term mortality when adjusted for all the covariates. Of note, 30-day model could not be completed due to lack of events (deaths) over a short period of time.
| OR | Wald χ2 | p-value | 95% CI | |
|---|---|---|---|---|
| Gender (F vs. M) | 0.84 | 0.6 | 0.4471 | 0.5 - 1.4 |
| Age | ||||
| 85-90 vs <85 | 2.19 | 3.9 | 0.0474* | 1.1- 4.2 |
| ≥90 vs <85 | 1.63 | 0.1 | 0.7303 | 0.8 - 3.2 |
| Race | ||||
| AA vs. Caucasian | 0.84 | 0.0 | 0.8301 | 0.3 - 2.3 |
| Hispanic vs. Caucasian | 0.40 | 4.1 | 0.0428* | 0.2 - 0.8 |
| Other vs. Caucasian | 1.04 | 0.4 | 0.5261 | 0.3 - 3.5 |
| Impaired gait | 3.26 | 9.3 | 0.0023* | 1.5 - 7.0 |
| Dementia | 2.34 | 8.6 | 0.0033* | 1.3 - 4.1 |
| AC continued at discharge | 1.18 | 0.3 | 0.5571 | 0.7 - 2.0 |
| Discharge to worse (SNF/hospice) | 0.70 | 1.6 | 0.1998 | 0.4 - 1.2 |
| Previous fall | 0.79 | 0.7 | 0.3901 | 0.5 - 1.4 |
| Transfusion | 1.50 | 1.8 | 0.1841 | 0.8 - 2.7 |
| Severe head injury | 2.16 | 3.3 | 0.0678 | 0.95 - 4.9 |
| Mechanical ventilation | 7.98 | 2.6 | 0.1076 | 0.6 - 100.0 |
| Congestive heart failure& | 3.61 | 12.8 | 0.0004* | 1.8 - 7.3 |
| Arrhythmia& | 1.56 | 2.4 | 0.1253 | 0.9 - 2.7 |
| TIA/CVA& | 1.25 | 0.5 | 0.4817 | 0.7 - 2.4 |
| Hypertension& | 0.99 | 0.0 | 0.9789 | 0.5 - 1.9 |
| Myocardial infarction& | 1.10 | 0.1 | 0.8160 | 0.5 - 2.4 |
& Indicates patient’s medical history
OR = odds ratio, CI = confidence interval, AA = African American, AC = anticoagulation, NH = nursing home, TIA = transient ischemic attack, CVA = cerebrovascular accident, SNF = Skilled nursing facility
Table 5: Multivariate Analysis of Long-Term Mortality.
Discussion
Anticoagulation is initiated for various reasons, most notably high CHA2DS2-VASc scores for the prevention of stroke in older patients with cardiac arrhythmias [6-8]. While the data suggests that in patients over 65, there is great benefit in the use of oral AC in preventing thromboembolic events, there is little data to suggest benefit or detriment in patients over 80, with ever increasing physical frailty and multiple comorbidities, at risk for fall/injury [9,10]. While we hypothesized that in patients over 80, presence of anticoagulation would contribute to patient’s demise, both shortand long-term following a fall, our data instead showed that: (1) although AC patients were more likely to require a transfusion during the initial admission, (2) AC was not a significant contributor to mortality, unless the initial fall resulted in bleeding from severe injuries.
Patients >80 face a myriad of obstacles in their daily life, including an overall functional decline, worsening visual acuity, proprioception, vestibular function, and problems with memory and mentation, all-the-while navigating their complex environment with slippery floors, poorly fitting shoes, or improper lighting [11-13]. In our study, most patients were noted to have impaired gait and either used or were recommended to use a cane, walker, or wheelchair to maintain stability. Patients often had multiple comorbidities (e.g.. cardiovascular, neurologic) that could predispose them to falling, especially in the AC group, where falls could be attributed to initiation of new medications, venous pooling in the lower extremities with resultant hypotension, hypoglycemia, or improper fluid balance [14]. While older patients often attribute their fall to an accidental “slip and fall,” research by Robinovitch et al. reported that more commonly, frailty and failing vision led to incorrect transferring and shifting of body weight, followed by physical overcorrection - accounting for 40% of the falls, while slips account for only 3% [15].
Published rate of injuries in patients following a fall from standing remains at 10-20% [16]. While worse injuries may be seen in association with anticoagulants, causation between AC and morbidity/mortality has not been well established. Rate of ICH, as identified by head CT scan, varies in literature from 5.1-29.1% [17]. A retrospective study by Mina et al. reported a two-fold increase in the risk of intracranial injury in patients on AC after blunt head trauma, but Gage at al. reported that presence of AC does not affect the incidence of ICH [18,19]. Our study showed an overall rate of 14%, but no significant difference between the groups: 10% in AC vs. 5% in non-AC group [17]. Robinovitch et al. reported that up to 75% of the time, falls involve the extremity or hand impact [15]. Our data was consistent with literature; most patients fell onto their outstretched arm in an attempt to break their fall. Interestingly, AC patients had less extremity injuries and more head injuries, although no difference in ICH. Authors hypothesized that patients with higher comorbidities (and therefore on AC) may lack upper body muscle strength, rendering their extremities ineffective, even when reaction time is reportedly not altered [15]. One could infer that the pattern of injuries seen in AC patients with multiple comorbidities and frequent head impact was a result of their frailty [20].
Following a fall, many older adults are forced to move from their homes in the community to long-term care facilities, as they are discovered to be unsafe living and ambulating independently. Our study showed that while only 5% of the patients were admitted from SNF, more than 40% were discharged to long-term care facilities after the fall. As supported by literature, patients with ICH were more likely to be admitted to SNF [19]. Interestingly, our study found that non-AC patients carried a 23% increased risk of discharge to a SNF as compared to those on anticoagulation. One plausible explanation could be that AC patients, with higher comorbidities, receive closer medical care and that increasing frailty of non-AC patients, remains undiscovered until their presentation at the hospital following a fall. Screening algorithms like STEADI (Stopping Elderly Accidents, Deaths and Injuries), developed by Centers for Disease Control and Prevention, can be administered in outpatient or inpatient setting to assess patients at risk for falls [21].
Increased risk of mortality in older AC patients has been reported. Mina et al. showed a four- to fivefold increased risk of death: 38% for AC patients receiving mainly warfarin and/or aspirin, as compared to 8% for non-AC group (p=0.006) [18]. In our study, AC patients had a higher rate of in-hospital mortality (5 vs. 0, p=0.0955), but this seemed to be a direct result of severe injuries following a fall. Gage at al. reported an increase in the severity of hemorrhagic events of AC patients, leading to poorer survival, but not increased short-term mortality following discharge [19]. Our data showed that AC patients were more likely to require ICU admission, tracheostomy, and transfusion with FFP and platelets in an attempt to reverse anticoagulation. However, similarly short-term follow-up (<30, <90 days), beyond the initial in-hospital mortality, showed no differences in survival. Logistic regression analysis, performed to eliminate confounding, demonstrated that mechanical ventilation, severity of head injury, admission from SNF, chronic medical conditions (e.g. CHF), and gait abnormalities were the most important contributors to mortality, but not anticoagulation.
Given that literature promotes prescription of AC in older patients with chronic conditions, especially in the setting of cardiac arrhythmias, due to a higher risk for ischemic events (13.7 per 100 patient-years), physicians continue to prescribe AC on discharge even following a fall [19]. In our study, 54% of the patients were discharged on AC. Our goal was to evaluate long-term effects on morbidity and mortality. Consistent with the literature, no difference was seen in the rate of readmission following a fall, or hemorrhagic and ischemic cerebral events regardless of anticoagulation treatment [22,23]. A retrospective review of patients, 65 years and older, showed that following a fall, one-year mortality was 21.3% [24]. While our patients were significantly older, we were able to show a similar trend with 40% of the patients on AC and 30% without AC dying at a two-year follow-up (p = 0.0726). Multivariate analysis found that discharge anticoagulants were not a significant contributor to long-term (two-year) mortality despite the fact that 1/3 of the patients were readmitted for a fall within one year [22,23]. Instead, logistic regression revealed impaired gait, dementia, CHF, and increasing age to be the most significant contributors to poor outcomes.
Our multivariate model failed to expose AC as a significant cause of mortality in the setting of fall from standing in patients >80. While AC may exacerbate the initial bleed, immediately following the fall, it is the injury itself that leads to patient demise. Instead, fall should serve as a marker of increasing frailty due chronic medical conditions or physical deconditioning related to aging. Given that most patient (long-term) deaths are related to their comorbidities, optimization of medical conditions, treatments and patient environments, could improve and prolong the lives of the older adults. Consistent use of the STEADI tool could allow for better assessment, diagnosis, and management of patients with gait difficulties or challenging home situations, in order to make necessary modifications proactively and potentially prevent fall readmissions.
One of the limitations of this study is that we were unable to evaluate the effectiveness of AC; instead, we could only record presence or absence of AC based on updated medical records. Additionally, our trauma center evaluates very old patients, who may be healthier than the average patient over 65. Therefore, our findings may not be directly transferable to other centers.
In conclusion, we were able to show that despite significant use of AC, outcomes between the AC and non-AC groups following a fall in patients over 80, were very similar. Severity of the initial injury may be exacerbated by the presence of AC, however, this may be quickly reversed using blood products and/or reversal agents. When confounders are eliminated using a multivariate analysis, it is the injury itself and not the presence of AC that lead to in-hospital patient demise. Long-term, considering that most patient deaths are related to worsening chronic medical conditions, initial falls can be used as foreshadowing events that can alert medical practitioners to the need for optimization of medical management and patients’ physical surroundings. Consequently, it seems as though, safe, individualized prescribing of AC with close monitoring of patient’s chronic conditions and their living environment, provides the key to quality survival of the aging population.
Acknowledgements
Authors have nothing to disclose; no conflicts of interest
Author Contributions
Vatche Melkonian – development of study design and concept, acquisition of data, preparation of manuscript, approval of the final version
Mackenzie Mayhew - acquisition of data, preparation of manuscript, approval of the final version
Rachele J Solomon – data analysis, preparation of manuscript, approval of the final version
Adilia Ortega – acquisition of long-term data, analysis and data interpretation, approval of the final version
Shari Selesky - data acquisition, drafting of manuscript, approval of the final version
Bradley Rogers – development of study design, data acquisition, patient acquisition, approval of the final version
Brenda Shaver – patient acquisition, data acquisition, development of study design, approval of the final version
Candace Pineda – development of study concept, acquisition of subjects, approval of the final version
Chauniqua Kiffin – study design, interpretation of data, preparation of manuscript, approval of the final version
Ibrahim I Jabbour – development of study concept, data acquisition, approval of final version
Sara Hennessy – study design and concept development, data analysis and interpretation, drafting and approval of manuscript
Juan D Arenas – study concept development, data interpretation, drafting and approval of manuscript
Eddy H Carrillo - study concept development, drafting and approval of manuscript
Andrew A Rosenthal - study concept development, data interpretation, drafting and approval of manuscript
Tjasa Hranjec – development of study design and concept, data acquisition, analysis and interpretation, drafting and approval of manuscript
REFERENCES
- Prevention CfDCa. “Facts About Falls.” In: Prevention CfDCa, ed. 2017.
- Phelan EA, Mahoney JE, Voit JC, Stevens JA. “Assessment and management of fall risk in primary care settings.” Med Clinics. 2015;99:281-93.
- Canada Go. “Seniors' Falls in Canada: Second Report.” In: Canada PHAo, ed.2014.
- Organization WH, Ageing WHO, Unit LC. “WHO global report on falls prevention in older age.” World Healt Org. 2008.
- Siu K-C, Chou L-S, Mayr U, van Donkelaar P, Woollacott MH. “Attentional mechanisms contributing to balance constraints during gait: the effects of balance impairments.” Brain Research. 2009;1248:59-67.
- Lip GY, Halperin JL. “Improving stroke risk stratification in atrial fibrillation.” Amer J Med 2010;123:484-8.
- Taillandier S, Olesen JB, Clementy N. “Prognosis in patients with atrial fibrillation and CHA2DS2‐VASc Score= 0 in a community‐based cohort study.” J Cardiov Electrophy 2012;23:708-13.
- Olesen JB, Torp-Pedersen C, Hansen ML, Lip GY. “The value of the CHA2DS2-VASc score for refining stroke risk stratification in patients with atrial fibrillation with a CHADS2 score 0–1: a nationwide cohort study.” Throm Haemos. 2012;107:1172-9.
- Lip GY, Lane DA. “Stroke prevention in atrial fibrillation: a systematic review.” Jama 2015;313:1950-1962.
- Singer DE, Chang Y, Fang MC. “The net clinical benefit of warfarin anticoagulation in atrial fibrillation.” Ann Inter Med. 2009;151:297-305.
- Schwab CW, Kauder DR. “Trauma in the geriatric patient.” Archives Surg. 1992;127:701-6.
- Fitzpatrick AL, Powe NR, Cooper LS, Ives DG, Robbins JA. “Barriers to health care access among the elderly and who perceives them.” Amer J Pub Health. 2004;94:1788-94.
- Colón-Emeric CS, Whitson HE, Pavon J, Hoenig H. “Functional decline in older adults.” Amer Family Phys. 2013;88:388.
- Kozloff MS, Adams Jr CA. “Trauma care of the elderly patient.” Rhode Island Med J. 2009;92:181.
- Robinovitch SN, Feldman F, Yang Y. “Video capture of the circumstances of falls in elderly people residing in long-term care: an observational study.” The Lancet. 2013;381:47-54.
- Alexander BH, Rivara FP, Wolf ME. “The cost and frequency of hospitalization for fall-related injuries in older adults.” Amer J Public Health. 1992;82:1020-3.
- Mann N, Welch K, Martin A. “Delayed intracranial hemorrhage in elderly anticoagulated patients sustaining a minor fall.” BMC Emerg Med. 2018;18:1-7.
- Mina AA, Knipfer JF, Park DY, Bair HA, Howells GA, Bendick PJ. “Intracranial complications of preinjury anticoagulation in trauma patients with head injury.” J Trauma Acute Care Surg 2002;53:668-72.
- Gage BF, Birman-Deych E, Kerzner R, Radford MJ, Nilasena DS, Rich MW. “Incidence of intracranial hemorrhage in patients with atrial fibrillation who are prone to fall.” Amer J Med. 2005;118:612-7.
- Murad K, Kitzman DW. “Frailty and multiple comorbidities in the elderly patient with heart failure: implications for management.” Heart Failure Rev. 2012;17:581-8.
- Prevention CfDCa. “STEADI - Older Adult Fall Prevention.” Control NCfIPa. 2021.
- Aronow WS, Ahn C. “Association of postprandial hypotension with incidence of falls, syncope, coronary events, stroke, and total mortality at 29‐month follow‐up in 499 older nursing home residents.” J Amer Geriat Soc. 1997;45:1051-3.
- Kiely DK, Kiel DP, Burrows AB, Lipsitz LA. “Identifying nursing home residents at risk for falling.” J Amer Geriat Soc. 1998;46:551-5.
- Larson LM, Sliter R, Helmer SD, Reyes J, Crawford G, Haan JM. “Outcomes in elderly fall victims: what happens after hospital discharge?.” Amer J Surg. 2016;212:1106-14.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Citation: Hranjec Tjasa (2023). Falling Down the Slippery Slope of Anticoagulation in Older Adults (>80): More Than Meets the Eye.�??�?� J Gerontol Geriatr Res. 12: 661.
Copyright: © 2023 Hranjec T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.