Indexed In
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Access to Global Online Research in Agriculture (AGORA)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Scholarsteer
- SWB online catalog
- Publons
- Euro Pub
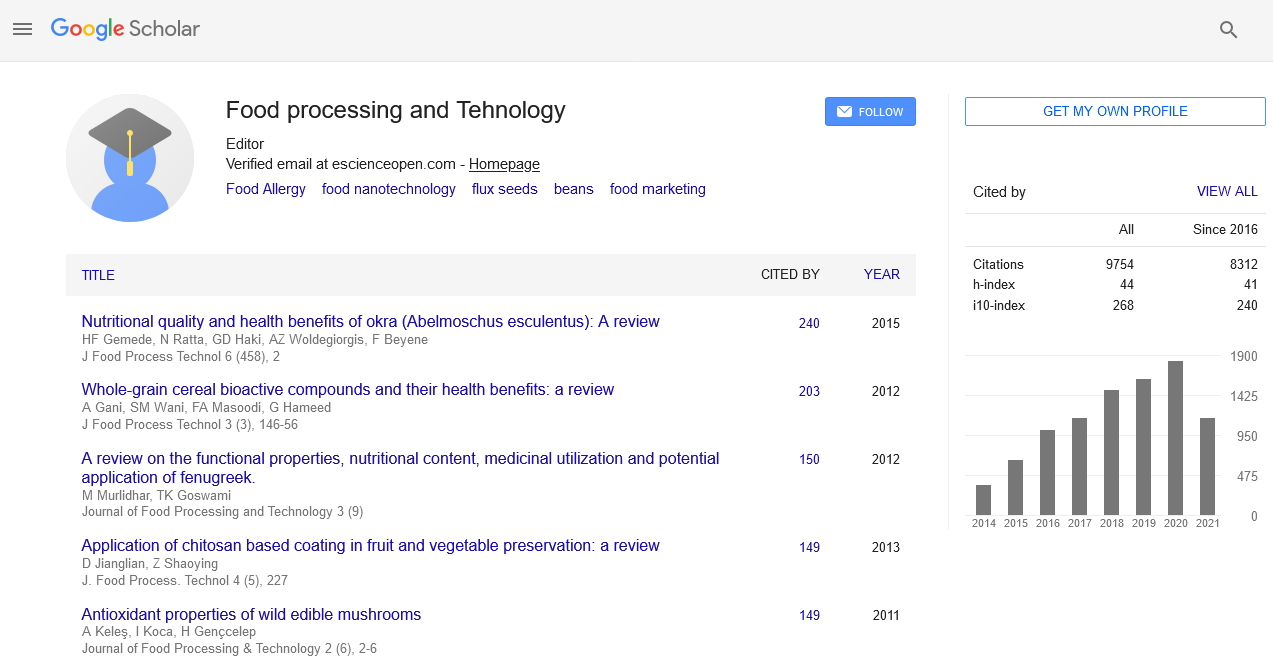
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2024) Volume 15, Issue 5
Evaluating the Effectiveness of Immunotherapy in Food Allergy Treatment
Leslie Kim*Received: 30-Sep-2024, Manuscript No. JFPT-24-26888; Editor assigned: 03-Oct-2024, Pre QC No. JFPT-24-26888 (PQ); Reviewed: 17-Oct-2024, QC No. JFPT-24-26888; Revised: 24-Oct-2024, Manuscript No. JFPT-24-26888 (R); Published: 31-Oct-2024, DOI: 10.35248/2157-7110.24.15.1125
Description
Food allergies represent a growing concern for millions of people worldwide. Considered by an abnormal immune response to specific food proteins, these allergies can lead to a range of symptoms from mild gastrointestinal discomfort to severe anaphylactic reactions. Traditional treatment primarily involves strict avoidance of the offending food and emergency intervention for accidental exposures. However, immunotherapy has emerged as a promising approach to modify the underlying allergic response and provide long-term relief. This article evaluates the effectiveness of immunotherapy in treating food allergies, exploring its mechanisms, benefits, limitations and future prospects.
Food allergies occur when the immune system erroneously identifies a normally harmless food protein as a threat. Antibodies known as Immunoglobulin E (IgE) are produced as a result of this immunological reaction. Upon subsequent exposure to the allergen, these IgE antibodies bind to mast cells and basophils, leading to the release of inflammatory mediators such as histamine, which cause allergic symptoms. Immuno- therapy aims to retrain the immune system to tolerate the offending allergens. Oral Immune Therapy (OIT) and Sub Lingual Immune Therapy (SLIT) are the two primary forms of immunotherapy. OIT involves administering gradually increasing doses of the allergen orally, while SLIT involves placing the allergen under the tongue. Both approaches seek to desensitize the immune system, reducing the severity of allergic reactions over time.
Mechanisms of immunotherapy
Immunotherapy works through several mechanisms:
Immune tolerance development: By repeatedly exposing the immune system to the allergen, immunotherapy encourages the development of regulatory T cells, which help modulate the immune response and promote tolerance.
Immunoglobulin G4 (IgG4) production: Immunotherapy often results in increased production of IgG4 antibodies. These antibodies compete with IgE for binding to the allergen, potentially reducing the allergic response.
Mast cell degranulation reduction: Immunotherapy can alter the behavior of mast cells, reducing their degranulation and the release of inflammatory mediators.
Changes in immune cell populations: Immunotherapy can lead to shifts in the populations of various immune cells, such as increasing the number of Trigs and decreasing Th2 cells, which are involved in allergic responses.
Benefits of immunotherapy
Immunotherapy offers several benefits over traditional allergen avoidance strategies:
Long-term tolerance: One of the most significant advantages of immunotherapy is its potential to induce long-term tolerance, even after the treatment has ended. This can provide lasting protection against accidental exposures and reduce the risk of severe allergic reactions.
Improved quality of life: By reducing the severity of allergic reactions and the need for strict avoidance, immunotherapy can significantly improve the quality of life for individuals with food allergies.
Reduced reliance on medication: Successful immunotherapy can decrease the reliance on medications, such as antihistamines and epinephrine, which are typically used to manage allergic reactions.
Limitations and risks of immunotherapy
Despite its benefits, immunotherapy has limitations and potential risks:
Allergic reactions: During the buildup phase of immunotherapy, patients may experience allergic reactions, including mild to moderate symptoms.
Duration of treatment: Immunotherapy often requires a long- term commitment, with treatment durations ranging from several months to a few years. This can be a barrier for some patients and families.
Variable response: Not all patients respond to immunotherapy and the degree of desensitization can vary. Factors such as age, the severity of the allergy and adherence to the treatment regimen can influence outcomes.
Access and cost: Immunotherapy can be costly and may not be widely available in all regions. Access to specialized centers and insurance coverage can impact the feasibility of treatment.
Immunotherapy represents a significant advancement in the treatment of food allergies, offering the potential for long-term tolerance and improved quality of life. Clinical evidence supports its effectiveness, particularly for common allergens like peanuts, milk and eggs. However, challenges such as treatment duration, potential risks and variability in response remain. As progresses, immunotherapy may become a more accessible and effective solution for managing food allergies, providing hope for those affected by these challenging conditions.
Citation: Kim L (2024). Evaluating the Effectiveness of Immunotherapy in Food Allergy Treatment. J Food Process Technol. 15:1125.
Copyright: © 2024 Kim L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.