Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2017) Volume 6, Issue 2
Effects of an Arginine-Enriched Oral Nutritional Supplement on the Healing of Chronic Wounds in Non-Malnourished Patients; A Multicenter Case Series from the Netherlands and Hungary
Abstract
Aim: To explore the effects of a specific arginine-enriched oral nutritional supplement on the healing of chronic wounds in non-malnourished patients.
Method: A case series using a prepared and Medically Ethically approved evaluation template. Out of three clinical centres in the Netherlands and one in Hungary, 27 patients with arterial leg ulcers, venous leg ulcers, diabetic foot ulcers, and pressure ulcers participated. They consumed a specific ready to drink arginine-enriched oral nutritional supplement daily, in addition to their regular diet and standard wound care, for a maximum of 12 weeks. Main outcome measures were wound healing progress, patients’ compliance and rating of the specific nutritional supplement.
Results: Seventeen females and twelve males with a mean age of 73.7 years were included. Within 2 to 12 weeks, complete healing occurred in eight ulcers, thirteen ulcers showed clear signs of healing through decreased wound surface area ranging from 25% to 88% reduction, and three ulcers kept unchanged. Overall, the daily oral nutritional supplements, on average two servings per day (= 400 ml), were almost fully consumed (99.5%), and the patients’ rating of the oral nutritional supplement was good.
Conclusion: Extra nutritional support with a specific ready to drink arginine-enriched oral nutritional supplement seems to be beneficial for the healing of different types of chronic wounds. The patients’ compliance with the product was very high, and they rated it as good. Further research, especially prospective randomised controlled studies on arginine-enriched oral nutritional supplements in patients with chronic wounds are necessary.
Keywords: Oral nutritional supplementation; Wound healing; Arginine; Zinc; Vitamin C
Introduction
Although many wounds will heal without delay or complications, both acute and chronic wounds may be affected by intrinsic factors such as diabetes and ischemia and extrinsic factors (e.g. infection and under-nutrition) [1]. Wound healing in any tissue follows a predictive sequence of cellular and molecular events leading to the repair of injured tissue [2]. However, some wounds somehow show failure in the healing processes and are then termed chronic wounds [3,4]. In contrast to acute wounds, chronic wounds such as pressure ulcers (PUs), leg ulcers (LUs) and diabetic foot ulcers (DFUs) are more complicated because the physiological process of the wound healing is significantly altered [5]. Wound chronicity is the result of one or more of the following factors: enhanced inflammation and proteolysis, extra cellular matrix degradation, impaired fibroblast migration together with a decrease in collagen synthesis and delayed epithelialization [6].
In the last decade, wound research has led to new and multifaceted wound healing interventions but delayed wound healing is still a major burden for health care in general and patients in particular [7]. The negative impact of chronic wounds on patients’ quality of life in terms of ulcer pain, sleep, mobility, social interaction is profound [8-10]. Worldwide, the chronic wound burden lies chiefly within the elderly population [6,11,12] and the morbidity accompanying age-related delay in healing, is readily acknowledged [11,12]. In 2013 in the Netherlands, a multi-centre cross-sectional point-prevalence measurement on chronic wounds in nursing home patients was conducted [13]. Out of 1514 patients, 63 patients had one or more chronic wounds, which resulted in a prevalence of 4.2%. Almost half (46%) of these wounds were PUs.
A good nutritional status contributes to a good health status, independence and quality of life, especially in older individuals. Nutrition is a relevant mediator for the preservation of skin tissue, strengthening of tissue resistance, and promoting tissue repair [14- 16]. Skin regeneration is a vital aspect of wound healing, facilitated by adequate nutrition. Adequate nutritional support therefore plays a pivotal role in wound healing. However, based on the results of two randomized controlled trials in patients with PUs, it appears that some nutrients play an active role in wound healing independently of protein and energy provision [17,18]. In the study of van Anholt et al. the authors had used the same specific high protein, arginine- and micronutrients-enriched oral nutritional supplement (ONS) in nonmalnourished PU patients and showed beneficial effects: accelerated PU healing and decreased wound care intensity (significantly fewer dressings required per week and less time spent per week on changing the dressings), which is likely to decrease overall costs of PU treatment [17]. The OligoElement Sore Trial of Cereda et al. shows that the additional provision of arginine, zinc, and antioxydants in the nutritional support in malnourished PU patients improved PU healing [18]. Strength of this large multicenter, blinded RCT study was that specific micronutrients were given within the content of appropriate nutritional care and both groups received a similar high-protein, highcalorie support to promote new tissue synthesis.
The studies of van Anholt et al. and Cereda et al. have shown the adequate nutritional support by an arginine-enriched ONS significantly improved the healing of PUs [17,18]. Subsequently, the question was whether this effect also counts for diabetic foot ulcers (DFUs), arterial leg ulcers (ALUs), and venous leg ulcers (VLUs). Therefore, a multicenter case series has been conducted to explore the effect of a specific arginine-enriched ONS and the healing process in different types of chronic wounds.
Objectives
The objective of the case series was to evaluate the effect of an arginine-enriched ONS in non-malnourished patients with a DFU, LU, or PU. The primary outcome measures were: 1) wound healing progress (complete healing and wound size reduction), 2) patients’ compliance to the specific ONS, and 3) patients’ rating of the specific ONS.
Methods
A convenience sample of patients with chronic wounds was recruited from three Dutch clinical centres: two nursing homes and one community wound centre, and one clinical health centre in Hungary. The wounds existed for at least three weeks and remained unchanged or worsened despite the centre’s standard wound care. This wound chronicity represented a rationale for the prescription of an arginineenriched ONS. If the patient had several wounds, the most severe ulcer was selected for follow-up. All patients were non-malnourished i.e., with a normal BMI and no signs of undesired weight loss or insufficient nutritional intake. Permission was sought and received from the Medical Ethics Committee of Maastricht University to undertake the case series using the evaluation template to record data. The patients received a comprehensive explanation of the study before providing informed consent. Patient anonymity and confidentiality were maintained throughout the evaluation period. Table 1 shows the general inclusion/exclusion criteria that were applied to all patients.
| Inclusion criteria |
|---|
| The patient is aged between 18 years and 95 years. |
| The patient is able to drink ONS. |
| The patient is not malnourished i.e., with a normal BMI and no signs of undesired weight loss or insufficient nutritional intake. |
| The patient has a regular diet. |
| The patient has standard wound care. |
| The patient has a life expectancy > 6 months. |
| The patient has a DFU, LU or PU that exists for at least 3 weeks and remained unchanged or worsened despite standard wound care. |
| If the case study starts in a clinical centre, the patient is able to visit the clinical centre once per two weeks after discharge. |
| Patient has provided informed consent. |
| Expected duration specific arginine-enriched ONS use >1 month. |
| Exclusion criteria |
| The patient in a severe medical condition e.g. ICU patients, sepsis, serious infection, malignancy requiring chemotherapy, recent (<3 months) myocardial infarction, organ failure, anaemia, and the acute phase after stroke (first two weeks). |
| The patient is suffering from drugs or alcohol in the opinion of the health care practitioner. |
| The patient has a protein restricted diet. |
| The patient used specific arginine-enriched ONS over the last 2 weeks. |
| The patient requires other oral nutritional supplements / tube feeds during the course of the case series. |
| The patient is malnourished i.e., has >5% weight loss in the previous month or >10% weight loss in the previous 6 months |
Table 1: General inclusion/exclusion criteria.
Table 2 refers to the additional specific inclusion criteria for patients with a DFU, LU or PU respectively.
| Diabetic foot ulcer (DFU): |
|---|
| The patient has a DFU > grade II (Wagner’s classification). |
| The patient has a DFU but not a PU or LU. |
| Leg ulcer (LU): |
| The patient has a LU with a size >1 cm2. |
| The patient has a LU but not a DFU or a PU. |
| Pressure ulcer (PU): |
| The patient has a PU category/grade >II. |
| The patient has a PU but not a DFU or LU. |
Table 2: Additional specific inclusion criteria per wound type.
In order to consume at least 5g arginine per day, all participants were daily offered one to three servings of a specific ready to drink arginineenriched ONS (Cubitan®, Nutricia) in addition to their centre’s regular diet and centre’s standard wound care, for a maximum of 12 weeks or until complete healing. The physician of the participants determined the number of ONS servings taking into account the renal function. One serving (200 mL) provides 250 kcal, 20 g protein, 3 g L-arginine, 250 mg vitamin C, 38 mg vitamin E (α-TE), 9 mg zinc, 1.5 mg carotenoids). At study start, wound existence (3-4 weeks, 5-12 weeks, >12 weeks), wound location, and patients’ mobility (bedfast, chairfast, walks occasionally, walks frequently) (Table 3) were recorded.
| Bedfast: Confined to bed. |
| Chairfast: Occasional slight changes in body or extremity position but unable to make frequent or significant changes independently. |
| Walks occasionally: Walks occasionally during day, but for very short distance, with or without assistance. Spends majority of each shift in bed or chair. |
| Walks frequently: Walks outside room at least twice a day and inside room at least once every two hours during waking hours. |
Table 3: Definitions of patient mobility.
Besides patient characteristics, information on wound surface area (WSA) (length x width), daily ONS servings (1, 2, 3), compliance per serving (100%, 75%, 50%, 25%, 0%), patients’ ONS rating (excellent, very good, good, moderate, bad), and photographs of the wounds were recorded monthly over the twelve-week period.
PUs were categorised/staged in line with the NPUAP-EPUAPPPPIA Guidelines in 2014 [19]. A Pressure Ulcer Scale for Healing (PUSH) was generated for all PU patients [20]. The PUSH score categorises the PU and generates a score in relation to; WSA (length × width), level of exudate (none, light, moderate, heavy), and type of tissue (closed, epithelial tissue, granulation tissue, slough, and necrotic tissue). The sum of the sub-scores provides the total PUSH score and comparison of these scores over time provides guidance on the status of the ulcer as regards improvement or worsening.
LUs were divided in ALUs and VLUs through measurement of the Ankle Brachial Pressure Index (ABPI). DFUs were graded in line with Wagner’s classification [21].
Trained and instructed research assistants were responsible for collecting the data among the participants. All data was anonymised and analysed using Microsoft Excel.
Results
Twenty-nine non-malnourished patients were included i.e., seventeen females and twelve males with a mean age of 73.7 years ranging from 50-95 years. The mean BMI was 27.6 and overall mobility ranged between chairfast (N=8), walks occasionally (N=8), and walks frequently (N=13). The chronic wounds involved, were DFU (N=9), ALU (N=5), VLU (N=8), and PU (N=7).
Overall at study start, the wounds existed between >12 weeks (N=21), 5-12 weeks (N=3), and 3-4 weeks (N=5).
Within 2 to 12 weeks, complete healing occurred in ten ulcers (3 DFUs, 3 VLUs, 4 PUs), thirteen ulcers showed clear signs of healing through decreased WSA ranging from 25% to 88% reduction (6 DFUs, 3 ALUs, 4 VLUs), and three ulcers kept unchanged (2 ALUs, 1 VLU). Three PU patients were lost to follow (one deceased, one hospital admission post stroke, and one withdrew due to cognitive decline). Overall, the patients used 2 ONS servings per day (= 400 ml), consumed 99.5% per serving, and rated the ONS as good. Tables 4, 5, 6 and 7 show the characteristics and ONS data of DFU, ALU, VLU and PU patients respectively.
| DFU patients (N=9) |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| Age | 79 | 89 | 55 | 50 | 62 | 63 | 54 | 69 | 53 |
| Gender | male | female | female | male | female | male | male | male | male |
| BMI | 25.7 | 32.7 | 27.3 | 41.5 | 26.7 | 36.6 | 29 | 35.9 | 36.3 |
| Main diagnose | stroke | hypertension | DM | DM | DM, hypertension | DM | DM | DM, hypertension | DM |
| Mobility | walks occasionally | walks occasionally | walks frequently |
walks frequently |
walks frequently |
walks frequently |
walks frequently |
walks frequently |
walks frequently |
| Regular diet | yes | yes | yes | yes | yes | yes | yes | yes | yes |
| Wound existence | >12 weeks | 5-12 weeks | >12 weeks | >12 weeks | >12 weeks | >12 weeks | >12 weeks | >12 weeks | >12 weeks |
| Wound location | left heel | left foot, 2nd toe |
left foot | left foot, 2nd toe |
right foot, hallux |
left foot, plantare |
left foot, plantare |
left foot, 2nd toe |
left foot, transmetatarsal amputation |
| DFU grade | III | II | II | II | II | II | II | II | III |
| WSA* at start | 20 cm2 | 1 cm2 | 6.29 cm2 | 3.28 cm2 | 0.61 cm2 | 1.16 cm2 | 1.45 cm2 | 1.45 cm2 | 57.49 cm2 |
| Effect on healing | |||||||||
| completely healed in weeks | - | 12 | - | - | - | - | 12 | 12 | - |
| % decreased WSA* (in weeks) |
60% (8)1 |
100% | 82% (12) |
45% (12) |
72% (12) |
58% (12) |
100% | 100% | 88% (12) |
| ONS° servings/day |
1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| ONS° compliance/serving | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% |
| ONS° rating |
very good | good | very good | very good | very good | very good | very good | good | very good |
DFU= Diabetic Foot Ulcer BMI= Body Mass Index *= Wound Surface Area°= Oral Nutritional Supplementation1= hospital admission after 8 weeks
Table 4: Characteristics of diabetic foot ulcer patients and ONS data.
| ALU patients (N=5) | 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|---|
| Age | 81 | 71 | 85 | 84 | 76 | |
| Gender | female | male | female | female | female | |
| BMI | 24 | 26.1 | 22.2 | 23 | 23.4 | |
| Main diagnose | diabetes | PVD1 | hypertension | hypertension | diabetes | |
| Mobility | walks occasionally | walks frequently | walks frequently | walks occasionally | walks occasionally | |
| Regular diet | yes | yes | yes | yes | yes | |
| Wound existence | >12 weeks | >12 weeks | >12 weeks | >12 weeks | >12 weeks | |
| Wound location | left leg | right leg | left leg | right leg | left leg | |
| WSA* at start | 45 cm2 | 46 cm2 | 6.6 cm2 | 16 cm2 | 12 cm2 | |
| Effect on healing: | ||||||
| % decreased WSA* unchanged |
33% | 53% | - | - | 75% | |
| - | - | x | x | - | ||
| ONS° servings/day | 1 | 2 | 2 | 1 | 2 | |
| ONS° compliance/serving | 100% | 100% | 100% | 100% | 100% | |
| ONS° rating | excellent | good | good | good | good | |
1= Peripheral Vascular Disease ; *= Wound Surface Area; °= Oral Nutritional Supplementation ; ALU= Arterial Leg Ulcer; BMI= Body Mass Index
Table 5: Characteristics of arterial leg ulcer patients and ONS data.
| VLU patients (N=8) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Age | 75 | 78 | 77 | 95 | 85 | 82 | 76 | 86 |
| Gender | male | female | female | female | female | female | female | female |
| BMI | 32.5 | 22.3 | 34.6 | 25.8 | 34 | 29.4 | 28.2 | 38 |
| Main diagnose | hypertension | hypertension | hypertension | diabetes | diabetes | hypertension | hypertension | hypertension |
| Mobility | walks freq | walks freq | walks occasion | walks occasion | chair- fast |
walks freq | walks occasion | chair- fast |
| Regular diet | yes | yes | yes | yes | yes | yes | yes | yes |
| Wound existence: | ||||||||
| 3-4 weeks | - | - | - | - | x | - | - | - |
| >12 weeks | x | x | x | x | - | x | x | x |
| Wound location | left leg | right leg | right leg | left leg | left leg | right leg | left leg | left leg |
| WSA* at start in cm2 | 5 | 1 | 0.5 | 6 | 24 | 12 | 36 | 17 |
| Effect on healing: | ||||||||
| completely healed in weeks | 12 | 8 | - | - | - | 8 | - | - |
| % decreased WSA* | 100% | 100% | - | 25% | 66% | 100% | 85% | 65% |
| unchanged | - | - | x | - | - | - | - | - |
| ONS° servings/day | 1 | 1 | 1 | 1 | 2 | 2 | 2 | 2 |
| ONS° compliance/serving | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% |
| ONS° rating | good | very good | very good | good | good | good | good | good |
*= Wound Surface Area;°= Oral Nutritional Supplementation; VLU= Venous Leg Ulcer; BMI= Body Mass Index
Table 6: Characteristics of venous leg ulcer patients and ONS data.
| PU patients (N=7) ss | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| Age | 52 | 75 | 66 | 80 | 77 | 75 | 66 |
| Gender | male | female | male | female | male | male | female |
| BMI | 24 | 20 | 22.9 | 21 | 20.5 | 29.6 | 28.9 |
| Main diagnose | Huntington | hyper-tension | stroke | hyper-tension | hyper-tension | hip fracture |
diabetes |
| Mobility | chairfast | walks freq | chairfast | chairfast | chairfast | chairfast | chairfast |
| Regular diet | yes | yes | yes | yes | yes | yes | yes |
| Wound existence: | |||||||
| 3-4 weeks | - | - | x | x | - | x | x |
| 5-12 weeks | x | x | - | - | - | - | - |
| >12 weeks | - | - | - | - | x | - | - |
| Wound location | left shoulder | right ankle | left heel | right hip | right heel | right hip | sacrum |
| PU grade | IV | IV | II | III | IV | II | II |
| WSA* at start in cm2 | 1 | 3.75 | 16 | 2.25 | 6 | 9 | 4 |
| PUSH score at start | 8 | 10 | 11 | 12 | 14 | 8 | 8 |
| PUSH score at end | 0 | 0 | 0 | 12 | 11 | 10 | 0 |
| Effect on healing: | |||||||
| completely healed in weeks | 8 | 8 | 4 | - | - | - | 2 |
| lost to follow-up | - | - | - | ×1 | ×2 | ×3 | - |
| ONS° servings/day | 3 | 2 | 2 | 2 | 2 | 2 | 2 |
| ONS° compliance/serving | 100% | 100% | 100% | 50% | 100% | 75% | 100% |
| ONS° rating | very good | good | good | mode-rate | good | good | good |
1= deceased after 4 weeks; 2= hospital admission after 8 weeks; 3= withdrawal after 5 weeks; (deterioration)*= Wound Surface Area; °= Oral Nutritional Supplementation; PU= Pressure Ulcer; BMI= Body Mass Index; PUSH= Pressure Ulcer Score of Healing
Table 7: Characteristics of pressure ulcer patients and ONS data.
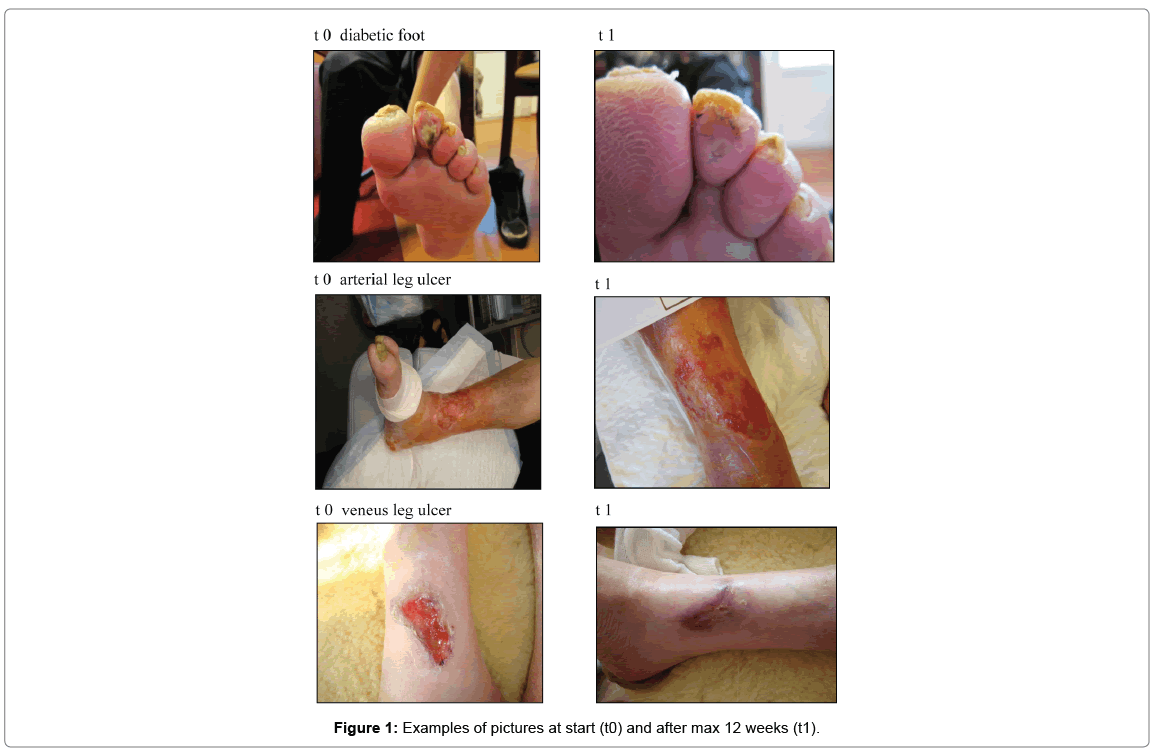
Figure 1 shows some pictures at start (t0) and after 12 weeks (t1) of a DFU, arterial LU and veneus LU respectively.
Discussion and conclusion
Twenty-nine non-malnourished patients were included in the case series. Within 2 to 12 weeks, complete healing occurred in ten ulcers (3 DFU, 3 VLUs, 4 PUs), thirteen ulcers showed clear signs of healing through decreased wound surface area ranging from 25% to 88% reduction (6 DFU, 3 ALUs, 4 VLUs), and three ulcers kept unchanged (2 ALUs, 1 VLU).
Overall, these case series show that use of an arginine-enriched ONS in addition to regular diet and standard wound care seems to be beneficial for the healing of different types of chronic wounds in non-malnourished patients. All primary outcome measures i.e., wound healing progress, patients’ compliance with and patients’ rate of the specific ONS were generally positive. These findings are in line with clinical studies showing a positive effect of nutritional supplementation with additional protein, arginine and micronutrients to promote PU healing [17,18,22-30]. In contrast, the findings of two studies were not in line with the findings of these studies [31,32]. A pragmatic randomised trial showed a significant improvement in wound healing in patients receiving standard nutrition supplement compared to wound-specific supplement, although there was a clinically relevant improvement in quality of life and patient satisfaction in the wound-specific ONS group [31]. The other study, a placebo-controlled randomised controlled trial (RCT), showed that the use of specialised amino acids did not appear to reduce PU wound size [32]. However, the OligoElement Sore Trial (OEST), a level 1 study, confirmed that the additional provision of arginine, zinc, and antioxydants in the nutritional support in malnourished PU patients improved PU healing [33]. Strength of this multicenter, double-blinded, placebo-controlled RCT study was that specific micronutrients were given within the content of appropriate nutritional care and both groups received a similar high-protein, highcalorie support to promote new tissue synthesis.
From these case series, it may be assumed that this positive effect also counts for the healing of chronic wounds, other than PUs. Actually, the arginine-enriched ONS is a nutritionally complete supplement, also enriched with arginine, Zinc and vitamin C.
The potential mechanisms involved in the improvement of the wound healing process by arginine, zinc and antioxidants e.g. vitamin C are the following: arginine improves protein anabolism and cellular growth, is a donor of nitric oxide, which increases blood flow to the wound area and acts as an immune response mediator. Zinc contributes to protein and DNA synthesis, immune function, and cellular proliferation. Vitamin C is involved in collagen synthesis, fibroblast proliferation, and cellular immunity [34,35].
Case series focus on the clinical course of events in terms of patient’s response to therapy and therefore they represent real-life care and provide a rationale for future high-quality clinical studies. On the other hand, case series are non-comparative by lacking a control arm so that treatment outcomes in the selected cases cannot be compared with those that did not receive treatment. A case series study involves first experiences as a rationale for future more in depth research.” It is therefore recommended that more prospective randomized controlled studies on arginine-enriched ONS are undertaken in patients with chronic wounds other than PUs.
References
- http://ewma.org/fileadmin/user_upload/EWMA.org/Position_documents_2002-2008/EWMA_08_Eng_final.pdf
- Enoch S, Leaper D (2005) Basic science of wound healing journal. Surgery 23: 37-42.
- Lazarus G, Cooper D, Knighton D, Margolis D, Pecoraro R (1994) Definitions and guidelines for the assessment of wounds and evaluation of healing. Arch Dermatol 130; 489-493.
- Robson M (1997) Wound infection: A failure of wound healing caused by an imbalance of bacteria. SurgClin North Am 77: 637-650.
- Demling R (2009) Nutrition, anabolism, and the wound healing process: An overview. Eplasty.
- Eming S, Krieg T, Davidson J (2007) Inflammation in wound repair: Molecular and cellular mechanisms. J Invest Dermatol 127: 514-525.
- Russo C, Steiner C, Spector W (2008) Hospitalizations related to pressure ulcers among adults 18 years and older in 2006.Healthcare Cost and Utilization Project (HCUP) Statistical Briefs.
- Franks PJ, Morgan PA (2003) Health-related quality of life with chronic leg ulceration. Expert Rev Pharmacoecon Outcomes Res 3: 611-622.
- Posnett, J, Franks P (2008) The burden of chronic wounds in the UK. Nursing Times. 104: 44-45.
- International Consensus (2012) Optimising wellbeing in people living with a wound. An expert working group review. London: Wounds International 2012.
- Ashcroft G, Mills S, Ashworth J (2002) Ageing and wound healing. Biogerontology 3: 337-345.
- Minimas D (2007) Ageing and its influence on wound healing. Wounds-UK 3: 42-50.
- Rondas AA, Schols JM, Stobberingh EE, Halfens RJ (2013) Prevalence of chronic wounds and structural quality indicators of chronic wound care in Dutch nursing homes. Int Wound J 12: 630-635.
- Mathus-Vliegen E (2001) Nutritional status, nutrition and pressure ulcers. NutrClinPract. 16: 286-291.
- Posthauer M (2006) The role of nutrition in wound care.Adv Skin Wound Care 19: 43-52.
- Schols J (2007) Dietary supplements are useful in the prevention and treatment of pressure sores. Ned TijdschGeneeskd 151: 1014.
- Van Anholt R, Sobotka L, Meijer E, Heyman H, Groen H (2010) Specific nutritional support accelerates pressure ulcer healing and reduces wound care intensity in non-malnourished patients. Nutrition 26: 867-872.
- Cereda E, Klersy C, Crespi A, D’Andrea F (2013) Disease-specific nutritional support in malnourished pressure ulcer patients: A randomized controlled trial. ClinNutr 32: 14.
- National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance (2014) Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. Emily Haesler (Ed.). Cambridge Media: Perth, Australia.
- www.npuap.org
- Wagner FW, Levin M, O’Neal L (1983) Supplement: Algorithms of foot care.The diabetic foot 3: 291-302.
- Frias Soriano L, LageVázquez M, Pérez-Potabella C, XandrlGraupera J, Wouters-Wesseling et al. (2004) The effectiveness of oral nutritional supplementation in the healing of pressure ulcers. J Wound Care 13: 319-322.
- Desneves K, Todorovic B, Cassar A, Crowe T (2005) Treatment with supplementary arginine, vitamin C and zinc in patients with pressure ulcers: a randomized controlled trial. ClinNutr 24: 979-987.
- Heyman H, Van De Looverbosch D, Meijer E, Schols J (2008) Benefits of an oral nutritional supplement on pressure ulcer healing in long-term care residents. J Wound Care 17: 476-478.
- Cereda E, Gini A, Pedrolli C, Vanotti A (2009) Disease-specific versus standard nutritional support for the treatment of pressure ulcers in institutionalized older adults: a randomized controlled trial. J Am GeriatrSoc 57: 1395-1402.
- Debats I, Wolfs T, Gotoh T, Cleutjens J, Peutz‐Kootstra C, et al. (2009) Role of arginine in superficial wound healing in man. Nitric Oxide 21: 175-183.
- Benati, G, Delvecchio D, Cilla D, Pedone V (2001) Impact on pressure ulcer healing of an arginine-enriched nutritional solution in patients with severe cognitive impairment. Arch GerontolGeriatr 1: 43-47.
- Brewer S, Desneves K, Pearce L, Mills K, Dunn L, et al. (2010) Effect of an arginine-containing nutritional supplement on pressure ulcer healing in community spinal cord patients. J Wound Care 19: 311-316.
- Chapman B, Mills K, Pearce L, Crowe T (2011) Use of an arginine-enriched oral nutritional supplement in the healing of pressure ulcers in patients with spinal cord injuries: An observational study. Nutrition & Dietetics 68: 208-213.
- LeighB, Desneves K, Rafferty J, Pearce L, Woodward M, et al. (2012) The effect of different doses of an arginine-containing supplement on the healing of pressure ulcers. J Wound Care 31: 150-156.
- Bauer J, Isenring E, Waterhouse M (2013) The effectiveness of a specialised oral nutrition supplement on outcomes in patients with chronic wounds: a pragmatic randomised study. J Hum Nutr Diets26: 452-458.
- Wong A, Chew A, Ong L, Zhang S, Young S (2014) The use of a specialised amino acid mixture for pressure ulcers: a placebo-controlled trial. J Wound Care 23:259-269.
- Cereda E, Klersy C, Serioli, M, Crespi A, D’Andrea F (2015) A nutritional formula enriched with arginine, zinc, and antioxidants for the healing of pressure ulcers. Ann Intern Med 162: 167-174.
- Doley J (2010) Nutrition management of pressure ulcers. NutrClinPract 25: 50-60.
- StechmillerJ (2010) Understanding the role of nutrition and wound healing. NutrClinPract 25: 61-68.
Copyright: © 2017 Neyens J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.