Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
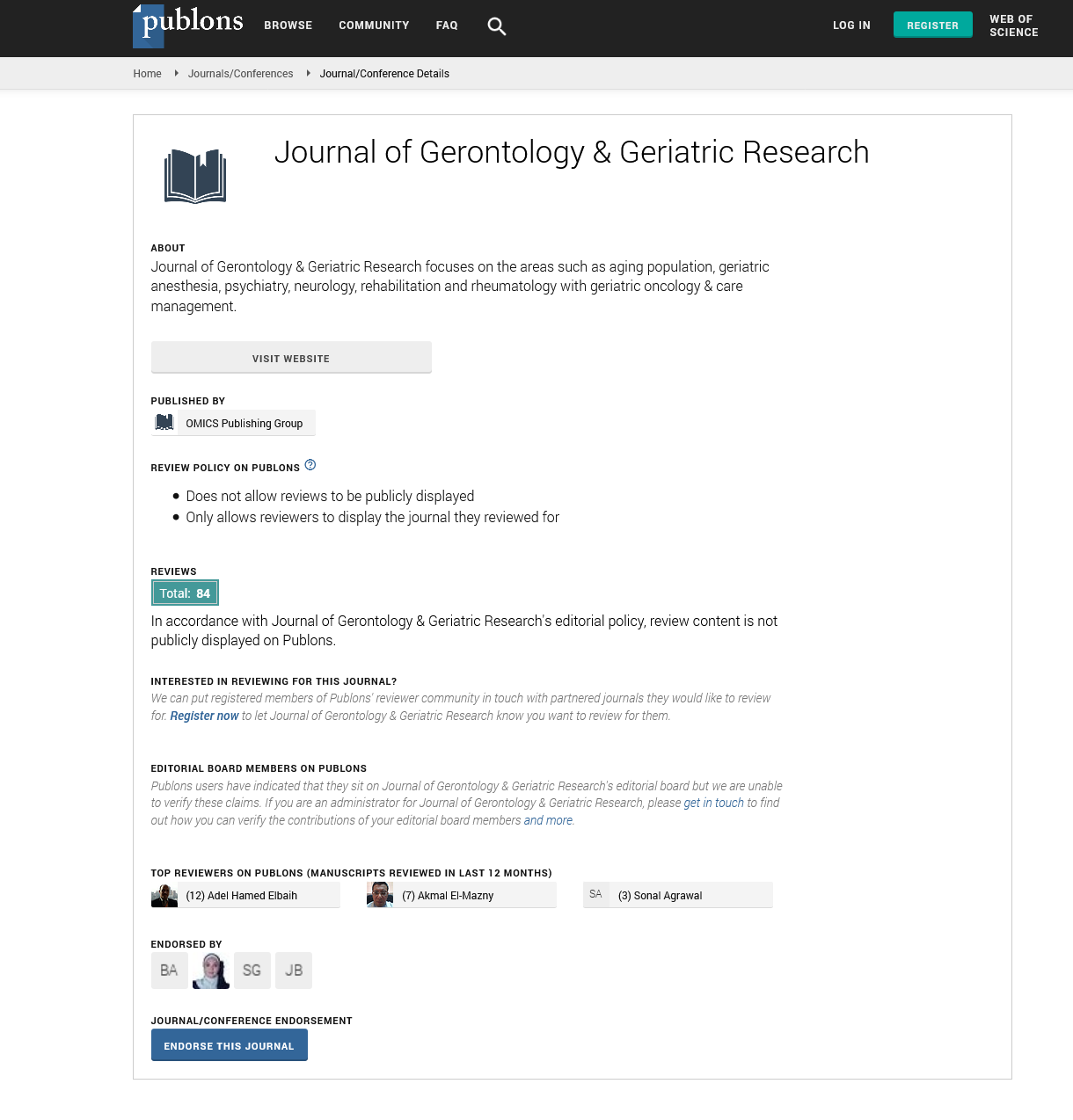
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2021) Volume 10, Issue 7
Diabetes Mellitus Type 2: Age-Related Risk Factors and Etiologic Factors
Suresh Babu G*Received: 14-Jul-2021 Published: 30-Jul-2021, DOI: 10.35248/2167-7182.21.10.564
Commentary
Poor nutrition, hereditary factors, obesity, and lack of exercise may all have a role in the rising prevalence of glucose intolerance and type 2 diabetes as people become older. The most major complicating variables for the development of type 2 diabetes linked with age are increasing body adiposity and decreased lean body mass. These alterations are typical of the ageing process, but they can also be observed in a variety of disease conditions with comparable unfavourable metabolic implications. The coexistence of these body composition changes and ageing in general is likely to have a significant influence on the development of type 2 diabetes in the elderly.
Aging is marked by a significant change in body composition. Lean body mass is declining as expected, but fat cell mass is rising. The loss of muscle mass, known as sarcopenia, explains majority of the decrease in lean body mass. Between the ages of 30 and 80, muscle mass is thought to decrease at a rate of around 6% each decade. Although the precise origin of this loss is unknown, neuroendocrine mechanisms decreased spontaneous and intentional physical activity, and intrinsic protein metabolic alterations in muscles all contribute to sarcopenia.
Reduced mitochondrial activity in muscle, as well as reduced ATP generation, is thought to play an essential role in the pathophysiology of age-related sarcopenia. It is also worth noting that decreased ATP generation in muscle occurs very early in young, insulinresistant children of type 2 diabetes patients, implying a connection between mitochondrial malfunction and muscle insulin resistance. However, aerobic exercise improves mitochondrial dysfunction and biogenesis but not insulin sensitivity in the elderly. Because muscle is the major location for insulin-mediated glucose clearance, muscle mass loss with age may have a significant impact on glucose metabolism.
The frailty syndrome in the elderly is defined by a frailty phenotype that includes sarcopenia, making it a risk factor for insulin resistance. Furthermore, as previously stated a reduction in protein and energy supply in utero and throughout the first year of life is a risk factor for IGT and type 2 diabetes. These risk factors for frailty are also related with low birth weight. Thus, early growth retardation is a risk factor for frailty as well as type 2 diabetes mellitus, possibly through the development of sarcopenia with age.
Most notably, not only is there an increase in fat cell mass, but its distribution is shifting as a result of an enrichment at the abdominal location (central distribution). This central shift of fat cell mass has significant metabolic implications and is a risk factor for numerous obesity and age-related metabolic disorders. The line between ageing and fat is razor thin. Surprisingly, the usual connection between total body fat mass and circulating leptin levels appears to be disturbed in the elderly, indicating that aberrant production of this adipose tissue may play a role in body fat alterations with age. Increased visceral and central fat cell mass, with or without decreased peripheral fat mass, has severe repercussions for the metabolic environment and is a risk factor for numerous obesity and age-related metabolic disorders, such as hypertension and hyperlipidemia.
Weight increase or central fat redistribution has definitely been linked to the development of type 2 diabetes. This anatomical distribution is associated with a rise in plasma free fatty acid (FFA) levels and appearance rate, a decrease in adiponectin secretion, and an increase in pro-inflammatory molecule secretion (e.g., TNF- and interleukin-6). Thus, these alterations encourage the emergence of insulin resistance and may have an adverse effect on beta cell function over time. Consequently, euglycemia will be maintained as long as the pancreatic beta cell insulin secretory response can compensate for this rise in insulin resistance. Once this compensatory mechanism is exhausted, insulin resistance leads to a gradual lack of glucose tolerance and, eventually, type 2 diabetes.
Citation: Suresh Babu G (2021) Diabetes Mellitus Type 2: Age-Related Risk Factors and Etiologic Factors. J Gerontol Geriatr Res. 10: 564.
Copyright: © 2021 Suresh Babu G. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.