Indexed In
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Access to Global Online Research in Agriculture (AGORA)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Scholarsteer
- SWB online catalog
- Publons
- Euro Pub
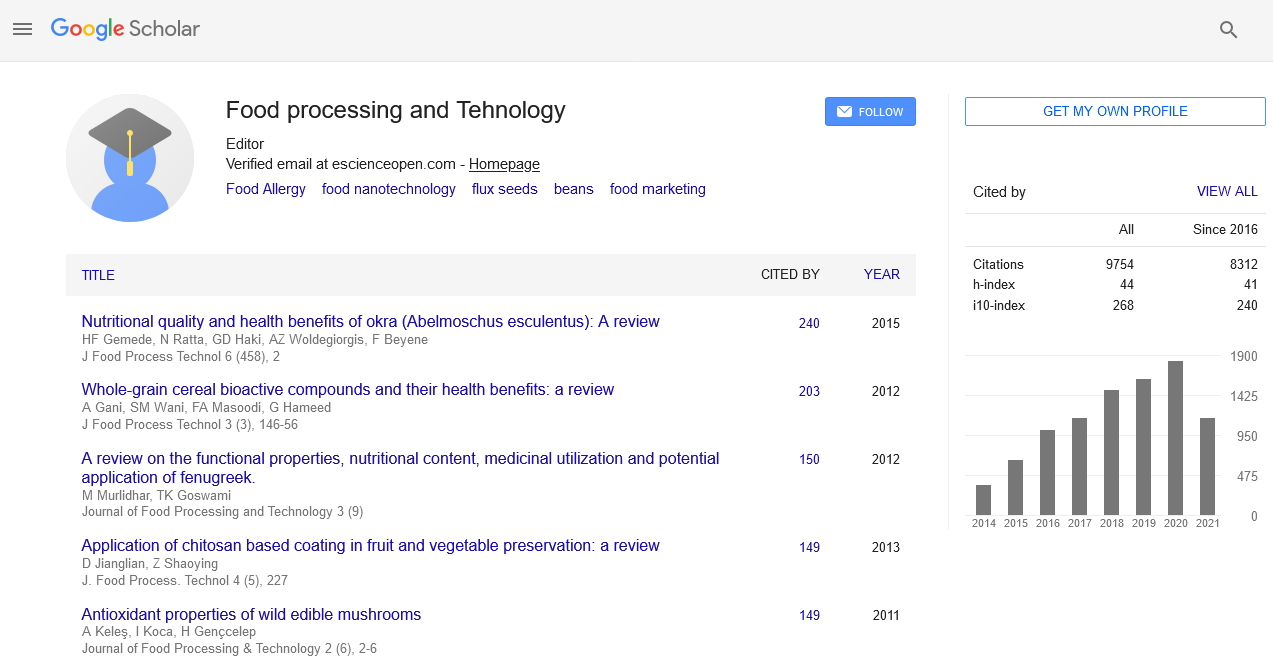
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Editorial - (2022) Volume 13, Issue 10
Clinical approaches to the diagnosis and causes of food allergy
Sehgal Shruti*Received: 13-Jun-2022, Manuscript No. JFPT-22-17110JFPT-22-17110; Editor assigned: 15-Jun-2022, Pre QC No. JFPT-22-17110(PQ); Reviewed: 29-Jun-2022, QC No. JFPT-22-17110; Revised: 12-Aug-2022, Manuscript No. JFPT-22-17110(R); Published: 19-Aug-2022, DOI: 10.35248/2157-7110.23.14.1023
Editorial
A food allergy is a type of immunological response to food that is abnormal. The allergic reaction's response symptoms might range from moderate to severe. Itching, swelling of the tongue, diarrhea, hives, difficulty breathing, and low blood pressure are some of the symptoms. This can be happening anywhere from a several hours after exposure. Anaphylaxis is the term used when the symptoms are severe. Food intolerance and food poisoning are two different diseases that are not caused by an immunological response.
Common possibilities include cow's milk, peanuts, eggs, shellfish, fish, tree nuts, soy, wheat, sesame, rice, and fruit. The most frequent disinclinations differ by nation. A family history of disinclinations, vitamin D insufficiency, rotundity, and a high position of hygiene are all threat factors. Immunoglobulin (IgE), a component of the body specific server, binds to the food particle and causes allergy. The problem is constantly a protein in the food. Seditious like histamine are released. A medical history, elimination diet, skin burrow test, blood testing for foodspecific IgE antibodies.
Causes of food allergy
Common food allergy are like milk, eggs, peanuts, tree nuts, fish, shellfish, soy, and wheat are the most current food though perceptivity situations vary by nation. The" big eight" are frequently appertained to as similar. Seed disinclinations, particularly sesame disinclinations, appear to be on the rise in numerous nations. Rice allergy is an example of a regional allergy that is more common in East Asia, where rice is a big part of the diet. Sensitivity to peanuts, a member of the bean family, is one of the most frequent food allergies. Peanut allergies can be severe, although they can sometimes be outgrown by children. A common allergy is tree nuts, which include almonds, Brazil nuts, cashews, coconuts, hazelnuts, macadamia nuts, pecans, pistachios, pine nuts, and walnuts. Sufferers may be allergic to only one type of tree nut or a variety of them. Although oils can be extracted from peanuts and seeds, such as sesame seeds and poppy seeds, minute amounts of protein may remain, causing an allergic reaction. Proteins in the white, rather than the yolk, are usually the source of sensitivity.
Another common food allergen is milk from cows, goats, or sheep, and many people can't tolerate dairy products like cheese. Because beef includes minute levels of protein that are also present in cow's milk, a small percentage of children with a milk allergy, about 10%, develop a reaction to it.
People may be allergic to proteins found in fish or to different proteins found in shellfish, which makes seafood one of the most prevalent sources of food allergens.
Diagnosis of food allergy
A medical history, elimination diet, skin prick test, blood testing for food specific IgE antibodies, or an oral food challenge are commonly used to make the diagnosis.
A little board with protruding needles is used for skin prick tests. The allergens are either placed on the board or on the skin directly. After that, the board is placed on the skin to puncture it and allow allergens to enter the body. If a hive develops, the person is suspected of having an allergy. This test can only detect IgE antibodies. Skin-prick tests cannot detect allergic reactions produced by other antibodies.
Skin prick testing is simple to do and provides results in minutes. Different allergists may utilize various testing devices. A "bifurcated needle," which resembles a fork with two prongs, is used by some. Others employ a "multitask," which resembles a little board with multiple pins protruding from it. A small amount of the suspected allergen is applied to the skin or placed in a testing instrument, which is then placed on the skin to prick, or break through, the top layer of skin. A little amount of the allergen is then injected beneath the skin. Anywhere the person is allergic, a hive will form. A positive or negative result is usually obtained from this test. Because it detects IgE, it is useful for promptly determining whether or not a person is allergic to a specific food. Skin testing can't tell you if you'll have an allergic reaction or what kind of reaction you'll have if you eat that allergen. They can, however, confirm an allergy based on a patient's previous reactions to a specific food. This approach is unable to detect non-IgE-mediated allergies.
Citation: Shruti S (2022) Clinical Approaches to the Diagnosis and Causes of Food Allergy. J Food Process Technol. 13:957.
Copyright: © 2022 Shruti S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.