Indexed In
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Access to Global Online Research in Agriculture (AGORA)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Scholarsteer
- SWB online catalog
- Publons
- Euro Pub
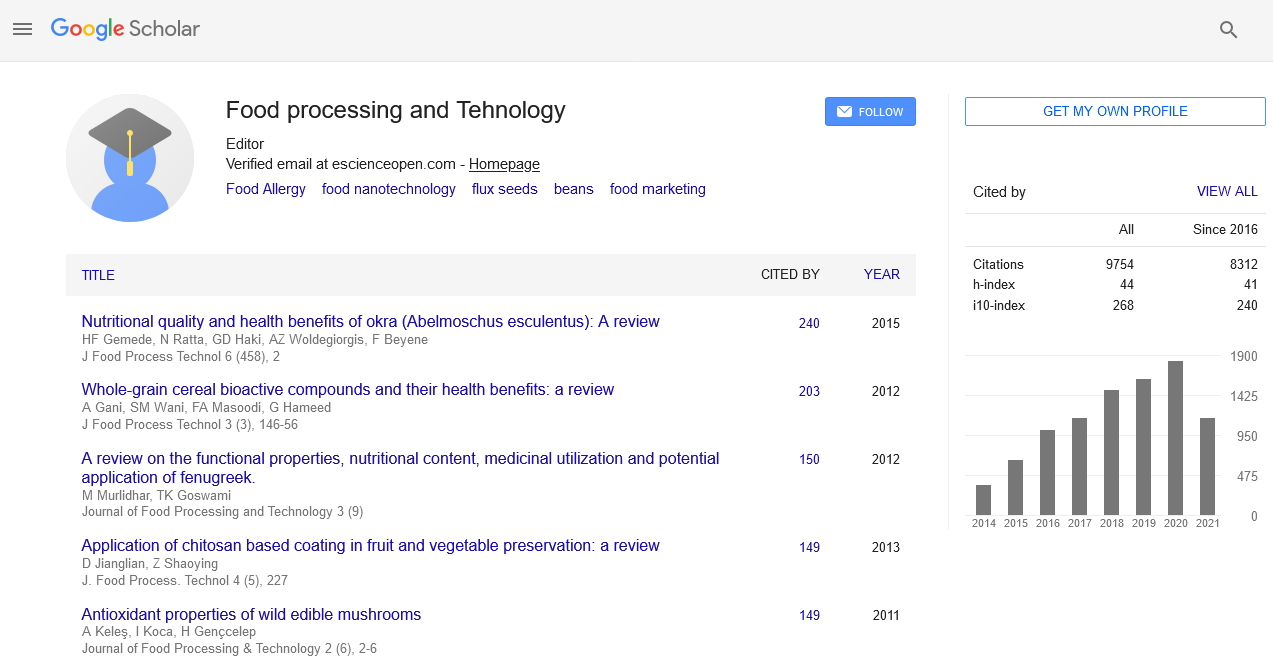
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2022) Volume 13, Issue 10
Changing Scenario of Diabetes Mellitus in India
Tanya Kesar*Received: 27-Jul-2022, Manuscript No. JFPT-22-17574; Editor assigned: 29-Jul-2022, Pre QC No. JFPT-22-17574; Reviewed: 03-Aug-2022, QC No. JFPT-22-17574; Revised: 26-Sep-2022, Manuscript No. JFPT-22-17574; Published: 03-Oct-2022, DOI: 10.35248/2157-7110.22.13.961
Abstract
Diabetes Mellitus is a multi-factorial chronic health disorder that influences a considerable portion of the population and the number of diabetes patient is predicted to rise, as stated by the World Health Organization (WHO). Because Type-2 Diabetes Mellitus (T2DM) affects the vast diabetic patients in the majority (roughly 90%-95%) and mono target treatment frequently fails to regulate blood glucose levels and associated comorbidities. The review focuses on the major systems that are directly related to T2DM or diabetic comorbidities. The glucagon and incretin systems, as well as the peroxisome proliferation activated receptors, are all considered agonists. Aldose reductase and tyrosine phosphatase 1B inhibitors, as well as sodium glucose transporters 1 and 2, are considered. Furthermore, several phytocomplexes are explored with a vision to multiple methods for Type 2 Diabetes Mellitus (T2DM).
Keywords
Diabetes mellitus; Type 2 diabetes mellitus; Health, Annual check-up; Symptoms
Introduction
Diabetes Mellitus (DM) is a complex chronic health disorder caused by the combination of environmental factors and hereditary [1,2]. Indeed, this illness is marked by a high level of familiarity and diabetes prevalence varies by ethnicity, such as black and Hispanic peoples and certain little numbers of America-Indians and Alaska natives, are more likely to develop diabetes due to a distinct genetic make-up. According to the WHO’s report on diabetes, the quantity of individuals with diabetes has nearly doubled to 422 million since, 1980 [3]. By 2045, the population is predicted to reach 693 million [4]. A sign of the illness is high blood sugar levels, which is caused by a lack of insulin concentration and/or activity, a pancreatic hormone are involve in the glycemic control. Diabetes has no remedy at the moment, it can, however, be treated and controlled. It's possible that you'll need medication and/or insulin to keep blood glucose levels as close to normal as feasible and to postpone or prevent the onset of diabetes related health issues. Healthy food and physical activity, on the other hand, may aid illness management. The kind of diabetes involved is important in choosing the appropriate treatment and the American Diabetes Association (ADA) established the categorization in 2018 [5].
Type 2 diabetes mellitus: Because of a progressive reduction of cell insulin synthesis, which often occurs in the context of insulin resistance.
Type 1 diabetes mellitus: Due to autoimmune cell death, complete insulin deficiency is common;
Other causes of diabetes include monogenic diabetes syndromes (such as neonatal diabetes and Maturity Onset Diabetes of the Young (MODY)), exocrine pancreas diseases (such as cystic fibrosis and pancreatitis) and drug or chemical-induced diabetes (such as with glucocorticoid use, in the third trimester of pregnancy).
Because T2DM affects the vast diabetic patients in the majority (about 90%-95%), this analysis focuses on possible medications that target several targets implicated in T2DM therapy.
Literature Review
T2DM (Type 2 Diabetes Mellitus)
T2DM may be characterized by resistance to insulin with relative insulin shortage or by an insulin resistance and a deficiency in insulin secretion. T2DM may strike anybody at any age. Adults, on the other hand, are the most affected. This type of diabetes, which affects 90-95 % of people with diabetes was previously known as type 2 diabetes, adult onset diabetes or non-insulin dependent diabetes Insulin resistance and relative (instead of absolute) insulin insufficiency symptoms. These individuals do not need insulin medication to survive, at least at first and frequently throughout their lifetime. Although the particular etiology of the illness is unknown, there are likely several possible reasons for this kind of diabetes [6]. The majority of people with this kind of diabetes are obese and obesity induces insulin resistance. Patients who may not meet the standard definition of obesity may have a higher proportion of body fat distributed mostly in the abdominal area. With a population of 183 million people, many individuals are unaware that they have diabetes. Type 2 Diabetes Mellitus (T2DM) accounts for more than 90% of cases [7,8].
Risk factors for diabetes
Diabetes may be caused by a variety of reasons, with the environment and lifestyle playing a significant impact; nonetheless, over half of diabetic individuals have at least one parent or family member who has the illness. The genes responsible have yet to be identified, although there is a significant link. Stress in our lives, such as frequent quarreling, life threatening situations, job pressure and so on, has been linked to diabetes owing to the produced chemicals adrenaline and cortisol. Both hereditary and environmental variables have the ability to significantly raise blood glucose levels [9]. Many research have looked at the links between various risk factors and the development of T2DM. The often established risk factor for developing T2DM are lipids, BMI, smoking, physical inactivity, inadequate education, dietary habits, vitamin D deficiency, family history and more recently, particular gene variants [9,10]. A higher BMI is a significant risk factor for T2DM, according to several longitudinal studies [11,12]. Obesity and T2DM have a strong positive relationship in both men and women In one research, smoking cigarettes was linked to a modest increase in diabetes risk, whereas drinking alcohol was linked to a lower risk of diabetes. The single most important predictor of diabetes is being overweight or obese. Lack of exercise, a bad diet, current smoking and alcohol abstinence have all been related to an increased risk of diabetes [13]. Currently smoking is a risk factor for T2DM development. According to many prospective studies [14].
Heavy smokers (those who smoke more than 20 cigarettes per day) had a greater link to T2DM than light smokers or exsmokers [15]. Furthermore, several studies have shown an elevated risk of Type 2DM in the first 2 to 3 years following quitting smoking [16]. Type 2 diabetes is caused by a combination of inherited and environmental factors. According to the findings, genes are considered to have a significant influence in the genesis of type 2 diabetes. Sedentary behavior, is regarded as a major risk factor for DM-II. Long term television viewing, as a proxy for a sedentary lifestyle, in both men and women, has been related to an increased risk of diabetes. Physical exercise, both moderate and vigorous, was linked to a decreased incidence of T2DM [17]. Physical activity, both directly and indirectly through beneficial changes in body mass and body composition, plays an important role in delaying or preventing insulin resistance and reducing it. T2DM in people at risk is prevented both directly and indirectly by enhancing insulin sensitivity. For a better understanding of the biochemical and molecular processes underlying the aetiopathogenesis of diabetes, genetic variables that control body fat distribution and glucose metabolism must be extensively explained. In one research of the Muslim population of Manipur, it was discovered that the majority of diabetic patients had stress, which was recognized as one of the diabetes risk factors. T2DM is a multifaceted illness that is triggered by several genetic variations interacting with environmental variables. If one parent has T2DM, the lifetime risk of T2DM is projected to be 38% (at the age of 80). If both parents have T2DM, the offspring's risk of developing the disease is predicted to be about 60% by the age of 60.
COVID-19 risk factor: Type 2 diabetes mellitus
In COVID-19, T2DM (Type 2 Diabetes Mellitus) is linked to a bad prognosis. Many mechanisms have been proposed to explain why diabetics have a worse prognosis for COVID-19, but they are still speculative at the time of writing. Some of these mechanisms include impaired neutrophil degranulation and complement activation, increased glucose concentration in airway secretion, which promotes viral replication, an exaggerated proinflammatory cytokine response in diabetes, reduced viral clearance and a higher prevalence of associated comorbidities.
One of the most important elements of the COVID-19- T2DM association is that information on for predictive purposes, hyperglycemia at the time of hospital admission is more important than HbA1c. COVID-19 is hypothesised to predispose infected persons to hyperglycemia, which leads to hyperglycosylation of the native viral receptor on the host cell surface, Angiotensin Converting Enzyme 2 (ACE2). Acute hyperglycemia causes inflammation, endothelial dysfunction and thrombosis in these individuals by causing oxidative stress. This might improve pathogenicity, viral virulence and vulnerability to serious infections by increasing tissue tropism and viral cell penetration. COVID-19 may alter the ability of pancreatic ‘B’ cells to manufacture insulin, a worsening of T2DM's underlying lack of glycemic control. By increasing viral tissue tropism and cell penetration, this might make viruses more virulent, pathogenic and susceptible to severe infections. COVID-19 may impair pancreatic B-cell insulin production, exacerbating T2DM's underlying lack of glycemic control. There is some evidence that newly diagnosed diabetes might cause complications is related with a greater rate of ICU admissions, invasive mechanical ventilation and diabetes related mortality that has already been diagnosed.
Methodology
Current scenario of T2DM
Diabetes has already been diagnosed in approximately 30 million people in India. In India's Crude Prevalence Rate (CPR) in metropolitan zones is predicted to be 9 percent. The frequency is around 3 percent of the whole population in rural areas. India now has a population of over 1000 million people, which serves to illustrate the magnitude of the issue. The true number of diabetes in India is estimated to be approximately 40 million. This indicates that India has the greatest proportion of diabetes of any nation on the planet. In India, Impaired Glucose Tolerance (IGT) is also becoming more prevalent. IGT is expected to affect 8.7% of people in cities and 7.9% of those in rural regions; however this figure might be conservative. Around 35% of IGT patients go on to acquire type 2 DM, indicating that India is in the midst of a healthcare catastrophe. The sort of diabetes that exists in India varies significantly from that which exists in the western world (Table 1).
| Anti-diabetic medication | Potential advantages |
|---|---|
| Pioglitazone | Inflammatory indicators might be reduced. |
| Metformin | It has been regarded as a powerful medicine that can help individuals with Type 2 diabetes with Covid-19 infection live longer. |
| Sulfonylureas | Possible improvement in illness severity |
| DPP-4 inhibitors | It's been suggested that DPP-4 is connected with SARS receptorbinding CoV-2's domain. It may also have immunomodulatory, anti-inflammatory and anti-fibrotic properties. Several studies have proposed using it as a COVID-19 agent repurposed. |
| SLGT-2 inhibitors A | Dapagliflozin has anti-inflammatory characteristics and reduces lactic acidosis, which might help to restore acid-base balance in hypoxia. |
| GLP-1 receptor agonists | During acute lung damage, there is an improvement in right ventricular function as well as anti-inflammatory benefits. |
Table 1: Non-insulin antidiabetics, both oral and injectable as well as insulin, are discussed in connection to COVID-19 treatment and results.
Drug therapy of diabetes mellitus among COVID-19 patients
Diabetic symptoms:
• Polyuria and polydipsia osmotic symptoms.
• Weight loss despite polyphagia.
• Tiredness and fatigue.
• Generalized pruritus.
• Recurrent urogenital infections.
Wounds that takes longer to heal more than half of all diabetic individuals will have no symptoms at all.
Medical Nutrition Therapy (MNT) is a mix of nutritional, behavioral and physical activity for people with diabetes.
A four pronged strategy is required:
• Nutritional evaluation that takes into account metabolic, nutritional and lifestyle factors.
• Setting objectives that are realistic, attainable and agreeable to the patients.
• Nutritional intervention, including nutritional education and customized meal planning depending on the family's eating habits.
Discussion
Evaluation determining whether or not the objectives have been met and making appropriate adjustments. The diet is tailored to the individual's age, gender, height, weight, BMI and cultural preferences are all factors to consider. The diet should be tailored to the patient's needs, follow a family pattern, be adaptable, provide variety and be timed according to the patient's daily routine.
Recommendations for diet
Energy: Sufficient to achieve or maintain a healthy body weight in adults, to promote correct growth and development in children and adolescents and to fulfill the increased demands of pregnancy and sickness recovery. Daily physical activity and exercise should be prioritised.
(Height in cm 100)* 0.9=Ideal Body Weight (IBW).
A moderately active diabetic patient may be given around 25 kcals/kg ideal body weight per day. The daily calories decrease should be progressive and not exceed 500 calories/day.
Carbohydrates
The affinations regarding an appropriate carbohydrate consumption in diabetic individuals is ambiguous. As a result, shared objectives for people with diabetes should be defined. The best guideline is to get 55%-60% of your energy from carbs. Carbohydrates should have a variety of properties. Although various carbs generate distinct glycemic reactions, overall carbohydrate management is crucial from a therapeutic standpoint. Carbohydrates from high fiber foods, such as oats, legumes, beans, barley, peas, unpolished grains and millets, Low Glycemic Index (LGI) in fruits are recommended. All T2DM patients should be urged to eat six modest meals each day. The food exchange method may be used to provide diversity and personalization to a diet plan.
Fibre
The overall population's fiber recommendation is 40 grams per day (2000 Kcals). Traditional Indian diets are recommended, which contain full grains, entire grams, soy, green leafy vegetables and sometimes fruits are examples of pulses mosambi, papaya, guava, apples, pears, oranges in moderation.
Proteins
In diabetics, protein should contribute for 12% to 15% of total calorie diet, which is comparable to the general population's guidelines. Proteins from pulses, grams, soya bean and peas, as well as low fat dairy products, fish and meats are recommended. Foods like cereals and pulses (4:1) may be supplemented to boost protein content while also providing satiety.
Fats
For persons with diabetes, fats should account for 20%-30% of total calorie consumption. Because the evidence for an appropriate quantity of total fat consumption for persons with diabetes is ambiguous, objectives should be tailored to the individual. The quality of fat is just as essential as its amount.
Trans-fats (less than 1% energy) should be avoided like the plague. Glycemic management and CVD risk variables may be improved in patients with type 2 diabetes who consume moderate amount of MUFA rich cooking oils and nuts as a result, this may be advised as a viable option to a low fat, high carbohydrate diet. Oils high in MUFAs, such as groundnut, mustard, rice bran and gingelly, are excellent choices. To keep the N6:N3 ratio between 5 to 10, oils high in n6 PUFA, such as safflower, cotton seed, sunflower and safflower should be blended with oils high in n3, such as soy and mustard. It's best to use a combination of oils or alternate them.
Salt
Recommendations for sodium consumption for persons with diabetes affect the overall population in the same way. Added (iodized) salt should not exceed 5 g/day. If anyone have hypertension or diabetes, you should limit your consumption to less than 3 g/day. Sodium limitation is essential in hypertensive and edematous individuals with nephropathy. Pickles, chutneys, packaged namkeens/savouries and sauces are all examples of preserved and processed foods that should be avoided.
Alcohol
Alcohol should be avoided whenever possible, but if it must be consumed, it should be consumed in moderation. Alcohol should not be included in the meal plan if it is eaten. However, it's important to remember that alcohol contains 7 kcal/g, which are referred to as "empty calories." Alcohol might cause hypoglycemia while you're fasting. Alcohol may increase dyslipidemia, fatty liver disease and obesity, neuropathy and blood glucose levels.
Sweetener
• Fructose, honey, corn syrup, molasses, fruit juice or fruit juice concentrates, dextrose, maltose, mannitol, sorbitol and xylitol are examples of nutritive sweeteners. All of them must be avoided at all costs.
• Non nutritive sweetener are now allowed for usage, including aspartame, acesulfame K, stevia, sucralose and saccharin. Pregnant women should be used in moderation amount.
Prevention of diabetes
Apart from treating diabetes and its effects, there is an immediate requirement for ways to avoid or at the very least, curb the diabetes epidemic. Several variables are assumed to play a role in the epidemic's escalation, the most significant of which being the fast epidemiological shift caused by urbanization and lifestyle changes. Individuals at risk must be identified before preventative actions may be implemented. There are various windows of opportunity for diabetes prevention (Figure 1).

Figure 1: Levels of prevention of diabetes.
Conclusion
Because T2DM has a complex pathogenic nature, interactions between many possible modulators at the same time seem to hold future prospects therapeutics. This could be accomplished by a novel strategy, especially the synthesis of multimodal chemicals. Unfortunately, numerous multifunctional ligands have had their clinical development halted owing to unfavorable side effects, perhaps as a result of their unbalanced and/or supratherapeutic activity. Given this, the promise of molecules that may modify the activity of many targets still needs to be explored further.
References
- Sun X, Yu W, Hu C. Genetics of type 2 diabetes: Insights into the pathogenesis and its clinical application. Bio Med Res Int. 2014:926713.
- Kaul N, Ali S. Genes, genetics and environment in type 2 diabetes: Implication in personalized medicine. DNA Cell Biol. 2016;35(1):1-12.
- WHO Diabetes Programme. WHO. 2019.
- Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, et al. IDF Diabetes atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271-281.
- Association AD. Classification and diagnosis of diabetes: Standards of medical care in diabetesd 2018. Diabetes Care. 2018;41(1):13-27.
[Crossref]
- American Diabetes Association. Definition and description of Diabetes mellitus. 2010.
- Lyssenko V, Laakso M. Genetic screening for the risk of type 2 diabetes: Worthless or valuable. Diabetes Care. 2013;36(Suppl 2):S120-S126.
- Chhajer: Cure Diabetes. Fusion Books. 2009.
- Valdés S, Botas P, Delgado E, Álvarez F, Cadórniga FD. Population-based incidence of T2D in northern Spain: The Asturias Study. Diabetes Care. 2007;30(9):2258-2263.
- Skarfors ET, Selinus KI, Lithell HO. Risk factors for developing non-insulin dependent diabetes: A 10 year follow up of men in Uppsala. BMJ. 1991;303(6805):755-760.
- Meisinger C, Thorand B, Schneider A, Stieber J, Döring A, Löwel H, et al. Gender differences in risk factors for incident type 2 diabetes mellitus: The MONICA Augsburg cohort study. Arch Intern Med. 2002;162(1):82-89.
- Almdal T, Scharling H, Jensen JS, Vestergaard H. Higher prevalence of risk factors for type 2 diabetes mellitus and subsequent higher incidence in men. Eur J Intern Med. 2008;19(1):40-45.
- Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, et al. Diet, lifestyle and the risk of type 2 diabetes melliyus in women. N Engl J Med. 2001;345(11):
- Esteghamati A, Hassabi M, Halabchi F, Bagheri M. Exercise Prescription in Patients with Diabetes Type 2. J Diabetes Metab Disord. 2008;l8:1-15.
- Nagaya T, Yoshida H, Takahashi H, Kawai M. Heavy smoking raises risk for T2D mellitus in obese men; but, light smoking reduces the risk in lean men: A follow-up study in Japan. Ann Epidemiol. 2008;18(2):113-118.
- Hur NW, Kim HC, Mo Nam C, Ha Jee S, Lee HC, Suh I, et al. Smoking cessation and risk of T2D mellitus: Korea medical insurance corporation study. Eur J Cardiovasc Prev Rehabil. 2007;14(2):244-249.
- Krishnan S, Rosenberg L, Palmer JR. Physical activity and television watching in relation to risk of type 2 diabetes, the black women's health study. Am J Epidemiol. 2009;169(4):428-434.
Citation: Kesar T (2022) Changing Scenario of Diabetes Mellitus in India. J Food Process Technol. 13:961.
Copyright: © 2022 Kesar T. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.