Indexed In
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 10, Issue 3
An Open-Label Pilot Study Using Contingency Management to Decelerate Risky Behaviors Among People Who Inject Drugs in Albania
Arian Boci*, Roland Bani, Alketa Zazo, Dritan Kamani and Ervin TociReceived: 25-Mar-2021 Published: 15-May-2021, DOI: 10.35248/2319-5584.21.10.108
Abstract
Introduction: Even though needle exchange programmes (NEP) are considered the single most important HIV prevention strategy for People Who Inject Drugs (PWID), yet the irregular uptake of services remains a challenge. To mitigate the harms of injecting drug use and increase access to prevention services, the approach of Contingency Management (CM) was implemented as an adjunct to the current NEP in Tirana, Albania. CM provides tangible rewards for clients to increase/decrease the frequency of target behaviours. The intervention hypothesized that using the reward system via CM might help to ensure regular use of prevention services.
Method: Eighty clients who were currently injecting drug users were equally divided in experimental and control groups. The intervention was conducted for eight months: two months were dedicated to the development and validation of the research protocol and six ones for the implementation phase.
Results: Compared with the control group, participants of the experimental ones had higher rates (up to threefolds) of daily attendance of the NEP. All of them, have been tested for HIV and Hepatitis Viral B&C (HVB&C), compared with 35% of those from the control group. One-third, introduced the sexual/injecting partner and the number of new female PWID introduced by clients of experimental group was significantly higher than the other one.
Conclusion: This intervention indicated the need for using innovative approaches to motivate PWID in using on regular bases prevention services. Regular uptake of NEP implies reduction in injection-related drug-taking behaviours and lesser risks for getting or transmitting HIV/HVB&C.
Keywords
Contingency Management, HIV, Hepatis Viral B&C, Needle Exchange Programs, People Who Inject Drugs.
Introduction
According to UNODC World Drug Report, the number of people who use and abuse with drugs is increasing, where nearly 150 states all over the world provide data on substance abuse in their countries [1]. At the end of 2018 it is estimated that worldwide there are nearly 269 million people who have used drugs at least once in the previous year, or said differently, 5.4 per cent of the global population aged 15 to 64. 5. The market trend on types of available substances has changed during the last decade. In addition to marijuana, heroine or cocaine, nowadays, people who use drugs user are prone to experiment with the new and more potent drugs, such as synthetic and non-medical use of pharmaceutical drugs. Polydrug use, increase number of young or occasional users and involvement in risky behaviors, pose a significant challenge to education, prevention and treatment of drug use disorders.
On the other hand, the number of People Who Inject Drugs (PWID), mainly opioids and non-medical use of prescription opioids is being increased [2]. Involvement in high-risk practices, such as needle/ syringe-sharing or other drug paraphernalia, practicing unsafe sex with their injecting or sexual partners, frequent incarceration or lack of access to prevention and treatment services put PWID at high risk for acquiring and transmitting human immunodeficiency virus (HIV) and hepatitis B and C virus (HCB/HCV) and Syphilis infection [3,4].
It is estimated that worldwide, nearly half of PWID were living with hepatitis C virus (HCV); one in eight was living with HIV, and 82.4% were co-infected with both HIV and HCV [5,6]. Moreover, due to frequent and unsafe injections, PWID have a complex set of health-related problems, including high rates of skin and soft tissue infections as well as high rates of fatal overdose [7].
The illicit drug use and abuse phenomenon emerged after 90-s in Albania, after the fall of iron curtain. Data from the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) and Institute of Public Health (IPH) show that the number of drug users in Albania is estimated to be around 60.000, of whom up to 8.000 them reported to have injected at least once in their life [8].
Albania, continues to be a low HIV prevalence country with nearly 1.400 cumulative cases diagnosed by the end of 2019 (the first case was diagnosed in 1993) [8,9]. The HIV prevalence among PWID remains low, where closed to 1% of PWID are living with HIV infection. However, the prevalence of hepatitis is significantly increasing among them, counting for 12% for HVB and closed to 40% for HCV. On the other hand, frequent injection and needle/syringe sharing, condomless sex and multiple partners is common among PWID [10]. Harm reduction, psycho-social and rehabilitation programs are lacking and those existent are mostly focused in capital city or main urban areas. Therefore, a great number of PWID, particularly those living in sub-urban or remote areas remain out of such services and face socio-health and economic challenges.
Prevention and treatment of drug addiction requires a multi-faceted approach, including application of psychosocial interventions as an adjunct to harm reduction programs. One of such promising interventions is the application of contingency management (CM) that use financial incentives to improve linkage to care of vulnerable groups [11]. This approach has found application among drug dependance clients, by using behavioral interventions and financial incentives to weaken drug use and strengthen abstinence [12,13]. The main elements of CM interventions are targeted contingency, behavioral reinforcers and monitoring aiming to promote social reintegration by sustaining compliance, abstinence and/or attendance [14,15]. Reinforces vary and could be cash, voucher, prizes or other financial/goods incentives [16,17]. In general, CM has shown promises result to increase linkage to care services among PWID by providing an immediate gain in financial resources tied to engagement in health care services [18].
In order to increase the number of PWID to attend prevention services and empower them to practice healthy behaviors, a contingency management intervention was piloted among PWID, living in Tirana, Albania. The goal of this prospective pilot study was to assess the effectiveness of contingency management (CM) in promoting attendance and adherence to Needle Exchange Program (NEP), linkage and referral to other socio-health treatment, as well as encouraging other drug users to be part of prevention programs. In case that study findings show promising results, this intervention will be used as a model to desing interventions or programs to improve the entire cascade of care for PWID.
Objectives
General objective
Evaluate the preliminary efficacy of reducing risky behaviors among people who inject drugs through piloting the contingency management intervention.
Specific objectives
Explore the effectiveness of contingency management approach in engaging people who inject drugs to practice healthy behaviors;
Evaluate whether the aplication of psycho-social interventions as an adjunct to harm reduction programs influences positive behavior change among people who use drugs and beyond.
Methodology
A case-control study was used to evaluate the effect of CM intervention among PWID. Case–control studies provide a statistically powerful, logistically manageable, and ethically acceptable alternative1 and are based on the identification of two groups: a) clients who volunteered to be part of the CM intervention would be identified and enrolled as cases; and b) those who won’t be part of the intervention would be enrolled as controls.
Recruitment settings and eligibility criteria
From April to May 2012, study participants were recruited among clients of the Needle Exchange Program (community-based and Drop-in Center), run by the “STOP AIDS” NGO, in Tirana, Albania.
The program team organized several group information sessions with outreach workers and prospective participants to distribute the information sheet and describe the nature of intervention, explain the consent form and procedure of CM activities. During these meetings was emphasized the importance of identifying and inviting female drug users to join the intervention.
To participate in the CM intervention, the prospective clients must met the following eligibility criteria:
- Be over 18 years old
- Be injecting drug user at least the last month (show visible needle tracks)
- Sign the consent form
- Complete the screening questionnaire
Those who didn’t meet the above criteria were not eligible to participate in the CM intervention.
All participants, regardless of group, ccompleted the baseline questionnaire which assessed their risky behaviors and previous history on attendance of harm reduction programs/activities.
The implementation of the intervention followed Three steps:
1. Development CM Intervention Protocol to Guide the Intervention and Help the Staff Step by Step through:
(i) Identification of a desired behaviour that a client should change and maintain during the intervention:
The main targeted behaviours were those related with the attendance and receive of the program services and activities offered by the program, such as: receiving clean needle/syringes (either in the field or in Drop in Centre); collecting used needles and storing to the collector site; testing for HIV/HVB&C, outpatient wound treatment; bringing new PWID (male/female) to the program, home visit to the clients’ family, participating in training and outdoor activities, switching from injection to OST or other rehabilitation programs, etc.
(ii) Establishment of the reward system whenever the desired behaviour occurs:
In this intervention, the standard reward for CM clients started from one point (equivalent to 1$) for receiving needle/syringes, up to five points (5$) for those who introduces a new client to the program. For attending all visits and achieving all desired behaviours, participants could receive up to $300 for a one-month regimen.
(iii) Evaluation instruments and development of indicators:
To evaluate their risky practices before and after participation in CM intervention, a questionnaire was developed to measure not only their involvement in risky behaviours, but also to assess their knowledge, attitude and practice regarding drug use and other risky behaviours. Results of both questionnaires (prior and post intervention) coupled with measurement indicators for each client were the base of measuring the success of CM intervention.
1. Validation of the Protocol
In order to validate the instruments tool, two weeks after the initiation of intervention CM participants, were invited in a focus group discussion to discuss and share with program team their experiences about the intervention. This period served as a pre-tested one and suggestions helped program team to adapt the intervention to better respond to participants’s needs and increase their motivation to continuing participation in this intervention.
2. Daily Managing, Monitoring and Evaluation of the Intervention
Based on the target behaviors and indicators, a database was developed to monitor and manage clients’ performance.
Data Collection and Analysis
Initially, one-hundred and five people responded positively to be part of the intervention. After the screening process, eighty people who were qualified to be part of the intervention were equally divided in two groups (case-control) with participation of forty people in each group. Both groups were evaluated before and after the intervention through a structured questionnaire, in addition to data collection instruments measuring clients’ attendance in the intervention.
Collected data were filtered out and analized using the SPSS 19 software, and for specific variables of interests a deeper statistical analysis was carried out to better understand the exposure factors that might have impacted the behavior change of study participants.
Discussions
During the six months of the intervention, there were recorded more than 2.260 client’s visits at Needle Exchange Program sites. Clients who were part of the experimental group, received needle exchange supplies (NES)2, with an average of 18-25 individual visits/per month (grouped median 15.3 individual visits per month) compared with the control one with an average of up to ten visits per month. While in respect of getting back the used needles, the number of individual visits by both groups was considerably lower (grouped median: 1.5 individual visits/per month). There are many reasons why the frequency of this service was low. The main reason was fear from the police, because if someone is caught with used needles for drug injecting purpose, according to Albanian Penal Code is considered an offence (Penal Code, Article 283 a and b). The other ones are related with the uncomfortability of transporting such items from place of injecting to collecting places, due to lack of small safe box/sharp containers, etc.
92.7% (n=38) of CM participants volunteered to be tested for HIV/HVB&C, compared with 45% (N=14) of the experimental ones. Nearly fifty percent of them received the second test after six months of participation in the intervention (as it was specified in CM intervention protocol). All clients who performed HIV testing received pre and post HIV test counseling, compared with 60% of the experimental group who attended both counseling sessions.
Although injecting drug users may have information regarding harm caused by injecting drugs, they often are not able to practice safe injection behaviours. Bearing in mind this fact, during the implementation phase of CM intervention, each week were organized trainings regarding prevention measures, safe injection practices, breaking the cycle and alternatives of injections, copying skills, etc. Therefore, 95% of clients (n=39) attended at least once a training or group counselling session (with a minimum of 1 training session and maximum 7 training session’s attendance; grouped median: 4.4 training sessions).
During the study period, there was only one active NEP operating in capital only, reaching around 150-200 urban street PWID, where a vast majority of them are male. Hence, a considerable number of PWID, including female ones remain unreached and uncovered with prevention services for a variety of reasons. One of the target behavior indicators was encouraging participants to introduce and bring new PWID clients to the program. On purpose, the bonus was higher in comparison with other behaviors (5 points- equivalent with 500 Albanian Lek/ALL). As results, during a six-month period were reached 106 new PWIDs (94 male and 12 female) and all of them were introduced to the program by the CM participants.
Out of 106 new clients, 81% (n=86) received the HIV testing, followed by pre and post HIV counseling (Figure 1).
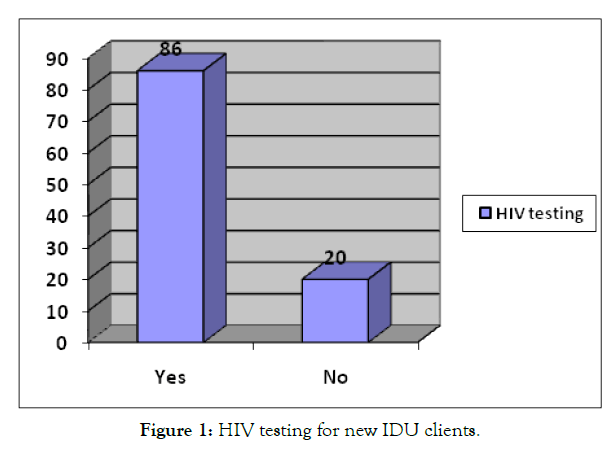
Figure 1: HIV testing for new IDU clients.
All female drug users accepted to be tested for HIV/HVB&C and received pre and post counseling. In addition to receiving NEP services, female clients seemed to be keener to welcome NEP team to their families, as all of them introduced NEP team to their partners/family members. Another intriguing finding was that female clients were also willing to join social outdoor activities along with other NEP and CM clients. All of them not only have regularly attended monthly outdoor activities, but also have brought their sexual/injecting partners or friends.
In their daily life, drug users face “double” stigma: stigmatization by the society and rejection by the family or community. Therefore, they are enforced to socialize with their peers and often to be involved in criminal activities to finance the drugs. Family bond is still strong in Albania, and despite problems with drug use, yet family may play an important role in reducing harm related to drug use. To address this problem, part of targeted behaviors was family visits. The aim of these visits was to counsel family members how to deal with drug problems in their families, and increase their skills on how and where to seek practical assistance for themselves or they loved ones in case of attending prevention programs, overdose prevention and management, HIV/HVB&C testing, wound treatment, opioid substitution therapy, etc.
In a six-month period, there were reached twenty-one families of clients who belong to experimental group and eighteen family members were tested for HIV/HVB&C (Figure 2).
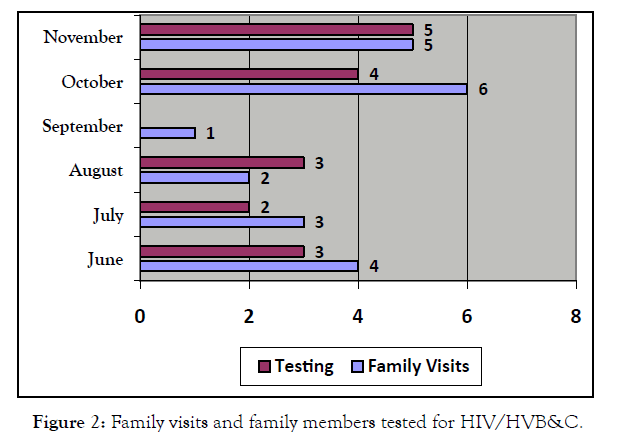
Figure 2: Family visits and family members tested for HIV/HVB&C.
Usually a person who injects drugs, due to several injections at the same place suffers from vascular and bacterial infections. A range of infections has been reported by our clients, starting from banal skin infections to necrosis of upper and lower extremities. Hence, part of the targeted behaviors under the CM intervention was to encourage PWID to seek and care for wounds caused by drug injection. At the end of intervention were carried out 61 wound treatment sessions for nearly thirty-two clients (12 of them were from control group), giving care and treatment for a variety of infections, such as: abscesses, bacterial infections, necrosis, inguinal hernia and thrombosis.
Although, the main objective of NEP is to provide clean needles/ syringes for each injection, yet helping drug users to consider or switch from injecting to non-injecting drugs or referral to opioid substation therapy (OST) is an objective to be considered. Therefore, under the CM component was assumed that encouraging drug users to reach the above objectives and reinforcing them to maintain positive behaviors by providing financial rewards would have been an influencing mechanism. As matter of fact, it was apparent that such approach did not work out, as only one participant switched from injection to non-injection drug administration route during the intervention. On the other hand, the referral to OST among the same group of clients was slightly higher, as nine CM clients were referred to the Methadone program.
Conclusion
In this intervention we assessed whether contingency management (CM) approach, in which PWID received financial incentives helped them to be engaged in healthy behaviours and increase attendance rates in the Needle Exchange Programs.
Data from this pilot study showed that CM could be a promising intervention for decelerating HIV risky behaviours and improve clients attendance and uptake of needle/syringe exchange services, especially those related to getting clean needles/syringes, HIV testing, introducing new clients (male and female) to get in contacts with NEP and also contacting partners/family members of injecting drug users.
Although the application of CM among Needle Exchange Program clients has a few published studies, findings from this study indicates the need for using innovative interventions to attract and motivate PWID in using on regular basis prevention and treatment programs, especially stigmatized or hard to reach subgroups, such as female drug users or their sexual partners. Regularly uptake of these services implies significant reductions in injection-related drug-taking behaviors and therefore lesser risk for getting or transmitting HIV/HVB&C.
As a conclusion, CM that target PWID who receive needle/syringe exchange services is a promising intervention can be used to reduce HIV risk behaviours and to improve the uptake of harm reduction services and may help to improve the design and implementation socio-healthcare programs for PWID in Albania and beyond.
1Schlesselman JJ. Case-control studies: design, conduct, analysis. New York: Oxford University Press; 1982. [Google Scholar]
2HR packages contained: 5 clean needles, 2 ampoules of distilled water, 1 condom, 2 alcohol swabs, 3 leaflets, 2 cotton filters.
REFERENCES
- United Nations on Drugs and Crime. World drug report. 2018.
- Banerjee G, Edelman JE, Barry DT, Becker CW, Cerda M, Crystal S et al. Non-medical use of prescription opioids is associated with heroin initiation among US veterans: a prospective cohort study. Addiction. 2016;111(11):2021–2031.
- Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health. 2017;5(12):e1192–e1207.
- UNAIDS. Health, rights and drugs-harm reduction, decriminalization, and zero discrimination for people who use drugs. Geneva: Joint United Nations Programme on HIV/AIDS. 2019.
- World Health Organization (WHO). Global Hepatitis Report. 2017.
- Center for Disease Control. Division of HIV/AIDS Prevention. 2018;30.
- EMCDDA. Albania National Report on Drugs. 2017.
- Institute of Public Health. HIV/AIDS in Albania. 2019.
- WHO. HIV in Albania. A National Programme Report. 2015.
- Institute of Public Health. Biological and Behavioural Surveillance of Injecting Drug Users, Albania. 2013.
- El-Sadr WM, Donnell D, Beauchamp G, Hall HI, Torian LV, Zingman B, et al. Financial incentives for linkage to care and viral suppression among HIV-Positive patients: A randomized clinical trial (HPTN 065). JAMA Int Med. 2017;177(8), 1083–1092.
- Griffith, JD, Rowan-Szal GA, Roark RR, Simpson DD. Contingency management in outpatient methadone treatment: a meta-analysis. Drug and Alcohol Dependence. 2000;58:55–66.
- Barry D, Sullivan B, Petry NM. Comparable efficacy of contingency management for cocaine dependence among African American, Hispanic, and White methadone maintenance clients. Psychol Addict Behav. 2009;23(1):168–174.
- Bickel WK, Amass L, Higgins ST, Badger GJ, Esch RA. Effects of adding behavioral treatment to opioid detoxification eith buprenorphine. J Consulting Clin Psych. 1997; 65(5):803–810.
- Bickel WK, Rizzuto P, Zielony RD, Klobas J, Pangiosonlis P, Mernit R et al. Combined behavioral and pharmacological treatment of alcoholic methadone patients. J Substance Abuse. 1988;1(2):161–171.
- Petry NM, Martin B, Simcic F. ‘Prize reinforcement contingency management for cocaine dependence: integration with group therapy in a methadone clinic’, J Consulting Clin Psych. 2005;73:354–359.
- Petry NM, Alessi SM, Hanson T, Sierra S. ‘Randomized trial of contingent prizes versus vouchers in cocaine-using methadone patients’. J Consulting ClinPsych. 2007; 75:983–991.
- Bassett IV, Wilson D, Taaffe J, Freedberg KA. Financial incentives to improve progression through the HIV treatment cascade. Current Opinion in HIV and AIDS. 2015;10(6):451–463.
Citation: Boci A, Bani R, Zazo A, Kamani D, Toci E (2021) An Open-Label Pilot Study Using Contingency Management to Decelerate Risky Behaviors Among People Who Inject Drugs in Albania. Glob J Agric Health Sci 10:108.
Copyright: © 2021 Boci A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

