Indexed In
- Open J Gate
- Academic Keys
- JournalTOCs
- ResearchBible
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 9, Issue 2
Aging and Oral Care: An Observational Study of Characteristics and Prevalence of Oral Diseases in an Italian Cohort
Dorina Lauritano1*, Giulia Moreo1, Francesco Carinci2, Raffaele Borgia1, Alberta Lucchese3, Maria Contaldo3, Fedora Della Vella4, Patrizia Bernardelli5 and Guido Moreo62Department of Morphology, Surgery and Experimental medicine, University of Ferrara, 44121 Ferrara, Italy
3Department of Medical-Surgical and Dental Specialties, University of Campania-Luigi Vanvitelli, 80138 Naples, Italy
4Department of Medicine, University of Bari, 70121 Bari, Italy
5San Carlo-RSA Bernardelli Hospital, 20037 Paderno Dugnano (MI), Italy
6Department of Internal Medicine, San Carlo Hospital, 20037 Paderno Dugnano (MI), Italy
Received: 27-Feb-2021 Published: 23-Mar-2021, DOI: 10.35248/2329-8847.21.9.248
Abstract
Background: Poor oral health is a common condition in patients suffering from dementia. Several aspects of thissystemic pathology contribute to causing oral problems: cognitive impairment, behavior disorders, communicationand, motor skills deterioration, low levels of cooperation and medical-nursing staff incompetency in the dental field.Objectives: The objectives of this study were to evaluate the prevalence and the characteristics of oral pathology in ademented elderly population, as well as to check the association between the different degree of dementia and theoral health condition of each patientMaterials and methods: In this observational study (with cross-sectional design) two groups of elderly patientssuffering from dementia, living in two different residential care institutions were recruited. The diagnosis of dementiaof each included patient was performed using the Clinical Dementia Rating Scale. In order to evaluate the oralhealth condition of the included subjects, each patient underwent a physical examination of the oral cavity, duringwhich different clinical parameters were analyzed (number of remaining teeth, oral mucosa, periodontal tissues, bonecrests). To each parameter, a score was assigned. Spearman’s Rho test was used.Results: Regarding the prevalence of oral pathology in elderly suffering from dementia, it emerged that 20.58% ofthe included patients had mucosal lesions and/or new mucosal formations (in most cases undiagnosed and thereforeuntreated). The prevalence of periodontal disease was equal to 82.35% and a marked clinically detectablereabsorption of bone crests was found in almost all patients (88.23%). 24.13% of patients, who underwent the oralexamination, had totally edentulous maxillae and/or with retained roots, without prosthetic rehabilitations. Thecorrelation index r showed the presence of a linear correlation (inverse relationship) between the degree of dementiaand the state of health of the oral cavity of each patientConclusion: Several factors contribute to poor oral health in the elderly suffering from dementia: cognitivefunctions deterioration, behavioral disorders and inadequate medical-staff nursing training on oral hygiene. Thisstudy also demonstrated that the lower the dementia degree is, the lower tends to be the oral health status. In orderto guarantee a complete assistance to these patients, residential care institutions should include in their healthcareprogram specific dental protocols
Keywords
Oral health; Edentulism; Dementia; Geriatric; Elderly patients
Introduction
Oral health is an essential component of general systemic health: it contributes to physical and mental well-being. To ensure each patient the most appropriate care, the dentist’s practice should not be exclusively focused on the teeth and supporting structures, but it should be extended to cover the oral health needs of patients in a holistic approach. Besides the treatment of specific oral pathologies, the dentist of the future should have the ability to diagnose and treat oral mucosal lesions, orofacial traumas, infections, pain symptoms, manifestations of systemic, genetic and congenital diseases [1]. Dentists should not only be perfectly updated on techniques and materials, but should also know how dental treatments can affect the individual's state of health/disease and how, at best, dental care should be conducted in subjects suffering from systemic diseases. In fact, medical and surgical conditions could influence oral health and oral healthcare, which could conversely have an impact on general health and healthcare [2].
Le Bars et al. [3] confirmed this theory, reviewing the dental literature concerning the impact of the removable prosthesis on the health status of medically compromised patients. The author showed that patient with dentures, suffering from certain systemic disease (diabetes mellitus, cancer, cardiovascular disease etc.), has higher levels of the organism Candida albicans in the oral flora compared to healthy patients. As a recent prospective study underlined, the age of the patients, the presence of one or more chronic disorders and the patients' drug regimens can influence dental treatment and oral health [4]. For this reason, the treatment approach in dentistry should always include medical history, in order to obtain the greatest possible number of information on the patient's state of health. Collecting medical history has the objective of defining whether or not it is appropriate to proceed with a therapy, to verify whether the patient is able to sustain the treatment and if some drugs are contraindicated [5]. Jainkittivong et al. highlighted that medical consultations could reduce the medical risk associated with dental procedures and unnecessary antibiotic prophylaxis. Therefore, for many dental patients, a good communication between dentists and physicians is essential for inappropriate care [6]. Unfortunately, the importance of medical history in oral care is often underestimated and it is consequently often neglected [4]. Among systemic pathologies an important role is covered by dementia, a mental condition, characterized by the evidence of cognitive decline in one or more domains (memory, language, executive functions, social cognition etc.), which have an impact on functional autonomy of the subject. One of the most important risk factors associated with the onset of dementia is age and, in an aging society, the impact of the phenomenon is projected to become overwhelming: it is easy to foresee that these pathologies will become, in a short time, one of the most important problems in terms of public health. In support of this, Rizzi et al. showed that dementia prevalence increases from 2-3% among people aged 70-75 years to 20–25% among elderly aged 85 years or more. Studies included in two recent systematic suggested that poor oral health is a common condition among the elderly with dementia. Compared to nondemented elderly, people with dementia have a higher prevalence of periodontal disease, mucosal lesions, caries, plaque, reduced salivary flow, outlining an association between poor oral health and dementia. Functional limitations associated with impairment in different cognitive domains, such as, difficulty in holding information in mind, in organizing or planning, inability in following directions, loss of judgment and inappropriate-aggressive behavior could explain the higher prevalence of oral health problems in dementia subjects. The demented may have problems in communicating, remembering, and performing the simplest actions. In the initial stage the most common symptom is the short-term memory failure; the patient can forget a specific word and use elaborate peripheral compensations; even the daily activities previously mastered (money management, driving a car, housekeeping) can become difficult. Personality changes, emotional frailty is possible. As patients progress to the intermediate stage of dementia, their ability to perform basic daily activities (washing, dressing) is reduced. Patients with severe dementia are no longer able to perform daily activities and become totally dependent on others for food, personal hygiene and movements. Due to cognitive impairment elderly with dementia are no longer able to take care of their oral hygiene, they rarely manage to communicate pain or discomfort related to the mouth and they sometimes show resistance aggressive behavior, making the treatment approach complicated. Moreover, several studies demonstrated the evidence of an association between periodontal disease and the onset/progression of dementia although the specific mechanisms of this relationship need further investigation.
Methods
For this observational study we used a cross-sectional design, in order to analyze oral health condition in elderly suffering from dementia at a specific point in time. This type of study is appropriate to investigate the prevalence of oral pathologies relationship between the cognitive deterioration and the oral hygiene of the population taken into consideration. The study was conducted according to the Declaration of Helsinki and independently approved and reviewed by the Institution’s Ethical Committee (#689/2014). A signed and written informed consent form was obtained from each patient, and if the patients would have been unable to do so, an informed written consent was obtained from their next of kin.
which provides a semi-structured interview with the patient and the caregiver/families, in order to rate the cognitive deterioration of the subject. The interview investigates six domains: memory, orientation, judgment/problem solving (cognitive domains), social activities, domestic activities/hobbies and personal care (functional domains). At the end of the interview, a score was assigned based on the impairment degree: 0=normal, 0.5=questionable/very mild, 1=mild, 2=moderate, 3=severe, 4=very severe, 5=terminal. The sample of population included one subject with mild cognitive impairment (CDR=1), nine subjects with moderate dementia (CDR=2), fifteen elderly with severe dementia (CDR=3), eleven patients with CDR=4 and three patients with CDR=5.
This study recruited two groups of elderly patients suffering from dementia, living in two different residential care institutions the first group had 18 subjects, of whom 14 were women and four were men and the second one consisted of 21 elderly, of whom 20 were women and one was a man, for a total of 39 patients, aged between 76 and 99 years (median age=89.92 years old ± 5.3 SD).
Results
This research aimed at defining the prevalence of oral disease in a population of elderly patients with dementia and describing the possible presence of a linear correlation between the degree of dementia and the oral health status
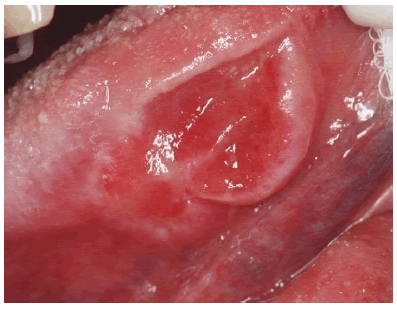
Regarding the prevalence of oral pathology, it emerged that 20.58% of the included patients (7/34) had mucosal lesions and/or new mucosal formations (in most cases undiagnosed and therefore untreated) and that, among these subjects, 8.82% (3/34) of the elderly presented potentially malignant lesions and/or new mucosal formations (ulcerated, bleeding lesions) (Figure 1).
Figure 1: Ulcerative lesion of the border of the tongue: a biopsy was performed with histological examination that confirmed the suspicion of oral squamous cell carcinoma.
A marked clinically detectable reabsorption of bone crests was found in almost all patients (88.23%: 30/34), which may be associated with edentulism or the presence of severe periodontal disease.
24.13% (7/29) of patients, who underwent the oral examination, had totally edentulous maxillae and/or with retained roots, without prosthetic rehabilitations
According to the obtained results, the degree of poor oral health status tended to decrease as the degree of dementia increased, showing the presence of an inverse linear relationship between the two quantitative variables. The comparison between the average state of health in the different degrees of dementia confirmed the linear nature of the relationship between the two variables: in patients with CDR = 2 the average health status was 5.8, in patients with severe dementia - very severe (CDR=3–4) was, respectively, equal to 4.9 and 4.4, while the terminal dementias (CDR=5) reached an average equal to 3.5.
The deterioration of the oral health conditions could also be associated with the level of collaboration, which varied, in most cases, in relation to the dementia degree. Patients with CDR equal to 2 were able to follow simple instructions (open your mouth, pull out the tongue, turn your head, report symptoms) for a more or less limited period of time (33.3%: 3/9 with level of cooperation=4; 66.67%: 6/9 with level of cooperation=3) and none of them showed a level of cooperation of less than 3. In 20% (3/15) of the patients with severe dementia (CDR=3) there was a level of cooperation equal to 2 (they transposed but partially followed/didn’t follow simple instructions, due to motor skills deterioration, abnormal and inappropriate reactions to the request), while 13.3% (2/15) transposed but had no reaction to requests. Out of 11 patients with very severe dementia, 3 (27.2%) did not transpose and therefore did not follow simple instructions (level of cooperation=0). The totality of patients with terminal dementia did not exceed the level of cooperation=0.
Discussion
The results of this study showed that the higher the dementia degree is, the lower is the patient’s cooperation and lower the oral health status. Evidence of poor oral hygiene in elderly patients with dementia are reported in literature by several studies. which demonstrated a greater decline in the salivary glands function, an increase in the prevalence of edentulism (up to about 65%), of the accumulation of plaque and tartar, of periodontal sites with gingival bleeding and a greater incidence of coronal and root caries, compared to elderly subjects with normal cognitive functions. Moreover, most of the patients included in our study suffers from arterial hypertension, condition that could have an impact on oral health. Antihypertensive medications may cause oral dryness, that could contribute to several oral diseases. The study demonstrated that xerostomia, hyposalivation and increasing number of oral microbiota were more common in patients who underwent antihypertensive treatment. On the other hand, oral chronic inflammatory diseases, such as periodontal disease, may have a role in the onset of the mechanism for pro-hypertensive immune activation The medical–nursing teams of the residential care institutions included in this research stated that, in the management of their patients, dental care is, in most cases, overlooked and that the maintenance of the oral health of the subjects is carried out almost exclusively by family members. Literature reports a general reluctance by medical – nursing team to give priority to oral assistance, due to limited knowledge in the dental field and to psychological barriers regarding “working in the mouth of another person. Furthermore, due to behavioral problems associated with dementia, patients often neglect oral hygiene, by refusing assistance from the facility staff. However, the management program of elderly patients suffering from dementia does not include any oral healthcare system, perpetuating the “oral abandonment” tendency. Although doctors and nurses of residential care institution don’t have specific skills to guarantee basic dental management of patients, the figure of the dentist is not included in the medical team of these facilities. On the other hand, the possibility of performing specific dental therapies in patients with dementia is very low. Dental therapies always require certain compliance by the patient, in order to guarantee their maintenance over time; in fact, before proceeding with any type of treatment, the level of cooperation must be evaluated, which, if considered insufficient, makes the therapeutic act itself contraindicated. Moreover, the objectives of a dental intervention in the health of patients with dementia are limited by their high mortality. However, in order to guarantee even to the elderly with dementia the right to live free from pain or discomfort caused by the oral condition, the healthcare for residents in residential care institutions should include specific dental protocols, to maintain adequate parameters of oral health and, therefore, to improve the quality of the patient’s life. Dentist and dental hygienist should cooperate, ensuring periodic checks and intervention to the patients suffering from dementia, according to individual needs. Dental care protocol for patients with dementia should include mechanical removal of plaque and food residue using toothbrushes, interproximal brushes, dental floss and fluoride-based toothpaste.
Conclusion
The recent increase in life expectancy has led to an increase in the number of people living in old age, a phenomenon that will result in a growth in the number of elderly people with dementia by the middle of our century The deterioration of cognitive functions and that of motor and communication skills in dementia patients makes the correct execution of daily oral hygiene maneuvers difficult. The elderly with dementia may present behavioral disorders, with aggressive or opposing attitudes towards the medical–nursing staff of the residential care institutions, preventing the possibility of being assisted. A common condition among subjects suffering from dementia is, therefore, a poor oral hygiene. In the elderly with dementia there is a high prevalence of oral soft tissue pathologies, such as moderate–severe periodontal disease and gingivitis, which are rarely diagnosed and, therefore, rarely treated. Most patients with dementia have partially or totally edentulous arches, with marked bone reabsorption and the residual dental elements, if present, are often compromised (coronal/root caries, gingival recessions, periodontal disease). Retained roots may be source of painful symptoms, which is not always showed by dementia patients. The presence of a tendentially linear correlation between the degree of dementia and the oral health status has also been demonstrated: the greater the severity of dementia is, the lower is the level of oral health. Finally, one of the main obstacles that prevent adequate oral care for these patients in residential care institutions is the inadequate medical-nursing staff training on oral hygiene. It is therefore of primary importance to educate the nursing staff, in order to meet the special dental needs of patients with dementia.
REFERENCES
- Wilson NHF, Luo, J, Jain RK. Dentists of the Future. Prim Dent J. 2019;8:30–3.
- Highfield J. Diagnosis and classification of periodontal disease. Aust Dent J. 2009; 54:S11–S26.
- Hazra A, Gogtay N. Biostatistics Series Module 6: Correlation and Linear Regression. Indian J. Dermatol. 2016; 61:593–601
- Kawas CH, Corrada MM. Alzheimer’s and dementia in the oldest-old: A century of challenges. Curr. Alzheimer Res. 2006;3:411-19.
- Pearson A,Chalmers J. Oral hygiene care for adults with dementia in residential aged care facilities. JBI Rep. 2004;2:65–113.
- Cawood JI, Howell RA. A classification of the edentulous jaws. J Oral Maxillofac Surg. 1988; 17:232-236.
Citation: Lauritano D, Moreo G, Carinci F, Borgia R, Lucchese A, Contaldo M, et al. (2021) Aging and Oral Care: An Observational Study ofCharacteristics and Prevalence of Oral Diseases in an Italian Cohort. J Aging Sci.9:248.
Copyright: © 2021 Lauritano D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License,which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited