Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2021) Volume 11, Issue 10
A Case Study on the Specific Oral Tolerance Milk Induction in 2-YearOld Child
Oksana Matsyura1*, Nándor Takács2, Lesya Besh1, Natalia Lukyanenko3, Livia Simon Sarkadi2 and Sandor G. Vari42Department of Food Chemistry and Nutrition, Institute of Food Quality, Safety and Nutrition; Faculty of Food Science, Szent István University, Budapest, Hungary
3Department of Propaedeutic Pediatrics and Medical Genetics,, Danylo Halytsky Lviv National Medical University, Lviv, Ukraine
4International Research and Innovation in Medicine Program, Cedars - Sinai Medical Center, Los Angeles, CA, USA
Received: 12-Dec-2020 Published: 26-Oct-2021, DOI: 10.35248/2161-0509.21.11.157
Abstract
Cow’s milk allergy is the most common food allergies in toddlers. Therapeutic approach of cow’s milk allergy consists of eliminating milk and its derivatives from the diet or specific oral tolerance induction. Use of an elimination diet deprives children of the nutrients and minerals they need for harmonious physical development. Specific oral tolerance induction is an alternative treatment option to gradually expose children to the food that is causing the allergy and let their bodies adapt, so that children can still get the beneficial nutrients.
Introduction
Milk is an important source of energy and calcium content and plays prominent role in growing of young organism [1-7]. The assessment of anthropometric measurements represents a key point of nutritional assessment, because growth is a sensitive indicator of adequate intake of energy and proteins [8,9].
Most studies have shown the prognosis of developing tolerance to cow's milk to be favourable, with the majority outgrowing their allergy throughout childhood and early adolescence. However, a minority of milk-allergic children become milk-allergic, and they can develop atopic march, which classically begins with atopic dermatitis, and progresses to IgE-mediated food allergy, asthma, allergic rhinitis [10]. Persistent cow’s milk allergy may become heavier with significant psychological and nutritional implications [11,12].
An ingestion of milk products is solely a marker of effective specific oral tolerance milk induction [13].
Case Report
Patient history
A 2-year-old girl had been born from a first pregnancy. The neonatal period passed without any complications. Manifestations of atopic dermatitis began to appear at the third month of life. Approximately at that time, the infant was introduced to milk formula and showed adaptation to it. A paediatrician appointed complex treatment and replaced the formula with complete hydrolysed protein; the infant’s condition was stable. At 1 year of age, the parents ceased feeding this mixture. They changed the diet and began feeding vegetables, fruits, cereals, meat and a small amount of dairy products.
At the age of 1.5 years, the child was given porridge cooked with cow’s milk. After 4 hours, she experienced continual abdominal pain with the appearance of an isolated, spotted and popular rash. At this time, the girl was with her grandmother but a possible association between her condition and milk porridge had not been considered. The girl continued to consume dairy products and was given symptomatic anti-histamine treatment. On the 5th day, she was anxious and developed a generalized and itching rash on her body (Figures 1 and 2). With these symptoms, she was taken to a paediatric hospital.

Figure 1: Skin changes in the leg, ankle and hand after consumption of dairy products.

Figure 2: Skin changes in the heel area after consumption of dairy products.
After careful analysis of the child’s diet over the previous 3 days, the doctor appointed a dairy-free diet and gave complex therapy that included glucocorticoids, antihistamines and enter sorbents. The condition of the girl was stable for 3 days during her hospital stay.
The recommended home care was a diet of dairy-free products, a course of antihistamines and use of topical emollients with frequent examinations at the hospital.
Allergology
The child was examined at age 2 years and 1 month and her condition was close to satisfactory. There were no rashes but dryness of the skin was noted. A repeated rash appeared periodically but regressed after a short course of antihistamines. The cause of the rash according to the parents is the consumption of dairy products. But the question remains unanswered: Why doesn’t the rash always appear after ingesting milk if it depends on milk?
Skin prick test results after the examination were: histamine 4 × 4 mm, control 2 × 2 mm, cow’s milk casein 6 × 7 mm (positive), egg white 2 × 2 mm, egg yolk 2 × 2 mm, and wheat 2 × 3 mm.
Diagnostic procedures were performed during remission. The results of skin prick test: histamine 4 × 4 mm, control 2 × 2 mm, cow’s milk casein 6 × 7 mm (positive).
Total IgE–340 kU/L. A comprehensive allergen screening (ALEX Allergy test) provides a clear picture of the patient’s sensitisation profile to milk and its components: Bos d 4 (α-Lactalbumin)–1.26 kUA/L, Bos d 5 (β-Lactoglobulin)–5.2 kUA/L, Bos d 8 (Casein)–1.93 kUA/L.
Oral food challenge test
Four weeks before the challenge test was performed, the product (milk and its derivatives) was eliminated from the diet. Drugs that may affect the response to the test were discontinued, such as antihistamines (for 10 days) and glucocorticosteroids (for 3 weeks).
The open oral food challenge test was performed to confirm the diagnosis of cow's milk allergy. Cow’s milk was gradually offered in portions up every 15 minutes to the onset of symptoms (Table 1). The challenge test was discontinued when the patients developed pathologic symptoms (skin and gastrointestinal) [14].
| Step | Volume of lactose-free milk, mla | Amount of protein, g |
|---|---|---|
| 1 | 0,1 | 0,0028 |
| 2 | 0,5 | 0,014 |
| 3 | 1 | 0,028 |
| 4 | 3,0 | 0,084 |
| 5 | 5,0 | 0,14 |
| 6 | 8,0 | 0,224 |
| 7 | 10,0 | 0,28 |
| 8 | 20,0 | 0,56 |
| 9 | 40,0 | 1,12 |
| 10 | 60,0 | 1,68 |
| Total volume – 147,6 ml | Total amount of protein – 4,1328 g | |
Table 1: Scheme of oral food challenge test.
The oral tolerance test was ended by consuming a total of 74,8 ml of milk (2,0944 g of protein). The child was given an antihistamine (first generation) and dexamethasone.
The recommendation for everyday milk consumption is 10 ml (0.28 g) of protein, which does not cause clinical symptoms. In the absence of exacerbation of any symptoms, a gradual increase in volume of the product under the control of a physician is planned within 2 months. Thus, an oral tolerance test provided the reason why this girl does not always develop symptoms after consuming milk or dairy products. That is why it is recommended to use 10 ml of milk daily in order to create tolerance to this product.
It is known that before making any correction to the diet it is always necessary to assess the physical development of the child, which will directly depend on the recommendations for the diet. We analysed the physical development of the girl: age (2 years 1 month), body weight (13 kg 800 g) and height (90 cm).
The formula for calculating proper body weight from 2 to 10 years is M (kg)=10+2n, where n is the age of the child in years. Thus, for this girl the calculated proper body weight is M (kg)=10+2 × 2=14 kg. The formula for calculating the body weight deficit=[(proper body weight - actual body weight)/proper body weight] × 100%. Thus, the body mass deficiency=[(14-13.8)/14] × 100%=1.43%. Consequently, the deviation of the indicators from the average is within the range of 1.43%, which is a variant of the norm.
By sigma tables, the physical development of the child is harmonious and corresponds to the average level according to age. According to the centile method, the growth rates of the child are within the median centile (75th centile).
The diet for our patient was appointed by the dietician and completely covered the nutritional needs of the child in terms of proteins, fats, carbohydrates and daily energy value. The recommendations for daily consumption of products for oral desensitization in the case of allergy to cow's milk protein are given in Table 2.
| Product | Standard consumption, | Recommended |
|---|---|---|
| G | consumption for patient, g | |
| Kefir, milk, yogurt | 600 | 10 (kefir only) |
| White cheese | 40 | - |
| Saw cream | 10 | - |
| Yellow cheese | 5 | - |
| Butter | 15 | 15 |
| Rabbit meat | 70 | 130 |
| Fish | 25 | 50 |
| Egg | 20 | 40 |
| Rye bread | 10 | 10 |
| Wheat bread | 60 | 60 |
| Vegetable oil | 7 | 10 |
| Fruits | 200 | 200 |
| Berries | 20 | 20 |
| Confectionery (sweets made from dry fruits, apple puree) | 40 | 40 |
| Porridge and pasta in prepared form | 150 | 250 |
| Potato | 100 | 100 |
| Vegetables | 200 | 300 |
Table 2: Recommendations for daily consumption of products during oral desensitization.
Given the fact that the child’s diet almost completely removes dairy products, it is necessary to increase the volume of other products to cover the daily requirements for proteins, fats, carbohydrates, vitamins and minerals [15]. The amount of meat and fish need to be increased from 70 g and 25 g to a recommended 130 g and 50 g, respectively. Increasing the amount of meat products requires an increase in the proportion of plant food. The quantity of vegetables in raw and cooked form should be up to 300 g (standard=200 g), and porridge up to 250 g in the finished form (standard=150 g). Increasing the volume of products should be tailored to the individual and only include products that do not provoke an allergic reaction.
At 7 months and 2 weeks after the start of oral tolerance induction, the patient was prescribed a liberal milk diet (amount of milk protein reached 4 g, 143 ml of milk). The levels of calcium and iron were increased (Figure 3).
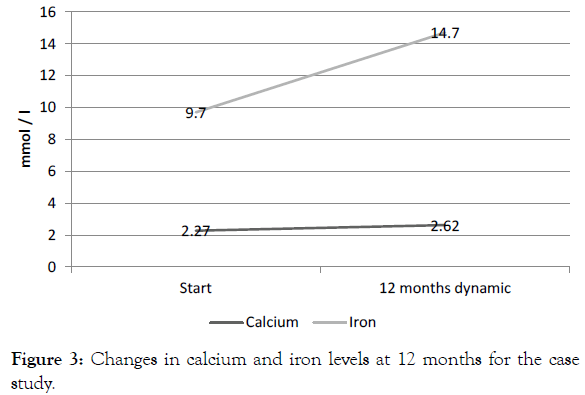
Figure 3: Changes in calcium and iron levels at 12 months for the case study.
Discussion and Conclusion
• Cow’s milk allergy is the most common food allergies in toddlers.
• Milk is an important source of energy and calcium content and plays prominent role in growing of young organism.
• Use of an elimination diet deprives children of the nutrients and minerals they need for harmonious physical development
• Specific oral tolerance induction is an alternative treatment option to gradually expose children to the food that is causing the allergy and let their bodies adapt, so that children can still get the beneficial nutrients.
• The example of this particular clinical case shows the importance of an individual approach to the prescription of a diet while taking into account the patient's age, physical development and particularities of the disease.
Funding Declaration
This work was supported by the Association for Regional Cooperation in the Fields of Health, the Science and Technology (RECOOP HST Association) and the participating Cedars – Sinai Medical Center - RECOOP Research Centers (CRRCs). RECOOP Grant # 009 BMYS RG 2019-2020. The funder played no part in the direction or execution of this research.
Conflict of Interest
The authors do not report any financial or personal connections with other persons or organizations that might negatively affect the content of this publication and/or claim authorship rights thereto.
Acknowledgements
We would like to express gratitude to individuals who assisted the authors in creating this article: head of Communal Nonprofit Enterprise “City Children’s Clinical Hospital of Lviv” – Dmytro Kvit and head of Allergy department – Valeriy Lygovskoy for their comprehensive help and encouragement.
REFERENCES
- Laemmli UK. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature. 1970;227(5259):680-685.
- Brusic V, Rudy G, Honeyman G, Hammer J, Harrison L, et al. Prediction of MHC class II-binding peptides using an evolutionary algorithm and artificial neural network. Bioinformatics (Oxford, England). 1998;14(2):121-130
- Doroshenko V, Airich L, Vitushkina M, Kolokolova A, Livshits V,et al. YddG from Escherichia coli promotes export of aromatic amino acids. FEMS Microbiology Letters. 2007;275(2):312-318.
- Fiocchi A, Schunemann H, Ansotegui I, Assaâ??ad A, Bahna S, et al. The global impact of the DRACMA guidelines cowâ??s milk allergy clinical practice. World Allergy Organ J. 2018 Dec;11(1):1-7.
- Flammarion S, Santos C, Guimber D, Jouannic L, Thumerelle C, et al. Diet and nutritional status of children with food allergies. Pediatr Allergy Immunol. 2011 Mar;22(2):161-165.
- Flom JD, Sicherer SH. Epidemiology of cowâ??s milk allergy. Nutrients. 2019;11(5):1051.
- Groetch M, Nowakâ?Wegrzyn A. Practical approach to nutrition and dietary intervention in pediatric food allergy. Pediatr Allergy Immunol. 2013; 24(3):212-221.
- Kvammen JA, Thomassen RA, Eskerud MB, Rugtveit J, Henriksen C. Micronutrient status and nutritional intake in 0-to 2-year-old children consuming a cowsâ?? milk exclusion diet. J Pediatr Gastroenterol Nutr. 2018;66(5):831.
- Luyt D, Bravin K, Luyt J. Implementing specific oral tolerance induction to milk into routine clinical practice: experience from first 50 patients. J Asthma Allergy. 2014;7:1.
- Maslin K, Oliver EM, Scally KS, Atkinson J, Foote K, et al. Nutritional adequacy of a cowsâ?? milk exclusion diet in infancy. Clin Transl Allergy. 2016;6(1):1-8.
- Meyer R, De Koker C, Dziubak R, Godwin H, Dominguez-Ortega G, et al. The impact of the elimination diet on growth and nutrient intake in children with food protein induced gastrointestinal allergies. Clinical and translational allergy. 2016;6(1):1-7.
- Muraro A, Halken S, Arshad SH, Beyer K, Dubois AE, et al. EAACI food allergy and anaphylaxis guidelines. Primary prevention of food allergy. Allergy. 2014;69(5):590-601.
- Alba LM, Lindor K. Nonâ?alcoholic fatty liver disease. Aliment Pharmacol Ther. 2003;17(8):977-986
- Rowicka G, StruciÅ?ska M, Riahi A, Weker H. Diet and nutritional status of children with cowâ??s milk protein allergy, treated with a milk-free diet. Int J Aller Medications. 2017;3:025.
- Black RE, Williams SM, Jones IE, Goulding A. Children who avoid drinking cow milk have low dietary calcium intakes and poor bone health. Am J Clin Nutr.2002;76(3):675-680.
Citation: Matsyura O, Takács N, Besh L, Lukyanenko N, Sarkadi LS, Vari SG (2021) A Case Study on the Specific Oral Tolerance Milk Induction in 2-Year-Old Child. J Nutr Disorders Ther. vol 11: 157.
Copyright: © 2021 Matsyura O, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

