Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
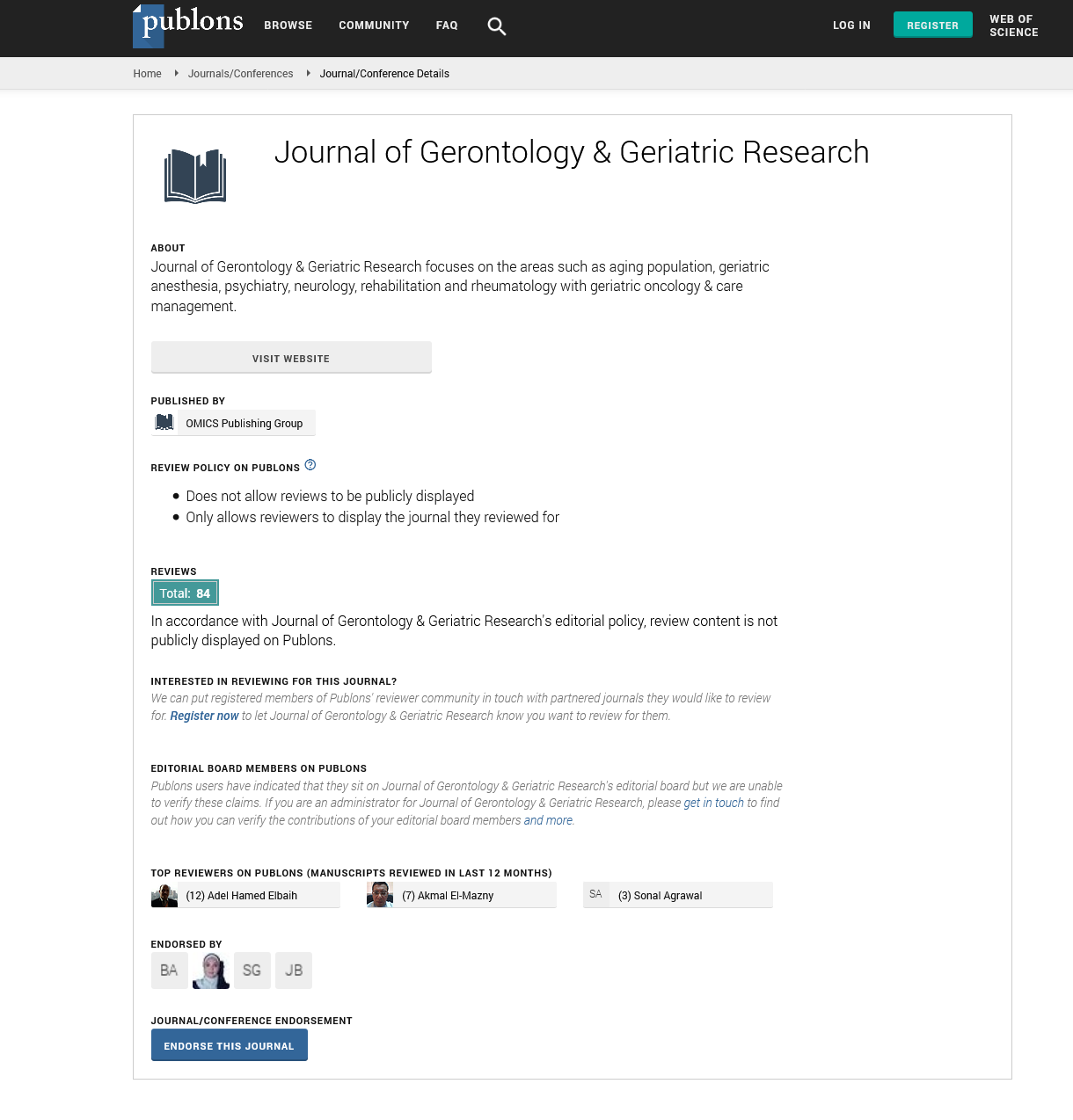
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Preventing falls in In-Patient Older Adult Mental Health Services: Different Causative Factors in Mental and Neurocognitive Disorders
Karen Heslop, Dianne Wynaden and Jenny Tohotoa
Aims: To compare falls sustained in two groups of patients (one with mental disorders and the other neurocognitive disorders), in two acute inpatient older adult mental health services in Western Australia (WA).
Background: Falls are the most common adverse event experienced during inpatient care. Older people with mental disorders and neurocognitive disorders constitute a high-risk group for accidental falls in hospitals.
Methods: Data relating to 207 fall events from 2010-2011 reported in medical records and incident reports were collected. Individuals who sustained a fall were grouped as having a mental disorder (n=73) or neurocognitive disorder (n=134) according to their primary ICD10 diagnosis.
Results: Significant differences in the factors that contributed to the fall between the two groups were highlighted. Falls sustained by those with a neurocognitive disorder were due to confusion and disorientation, and psychotropic medication effects. Their falls were more likely to be unwitnessed and injuries were generally less severe. Falls sustained by older adults with mental disorders were attributed to symptoms of their illness or medication side effects and tended to result in more severe injuries requiring medical treatment or further investigation.
Conclusions: Older adults with neurocognitive disorders and behavioural and psychological symptoms associated to dementia have different falls risk factors related to their specific illness and cognitive functioning. There is a need for health professionals to receive training to assess, manage and provide appropriate interventions to reduce the specific falls risks in patients with both mental disorders and neurocognitive disorders.