Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
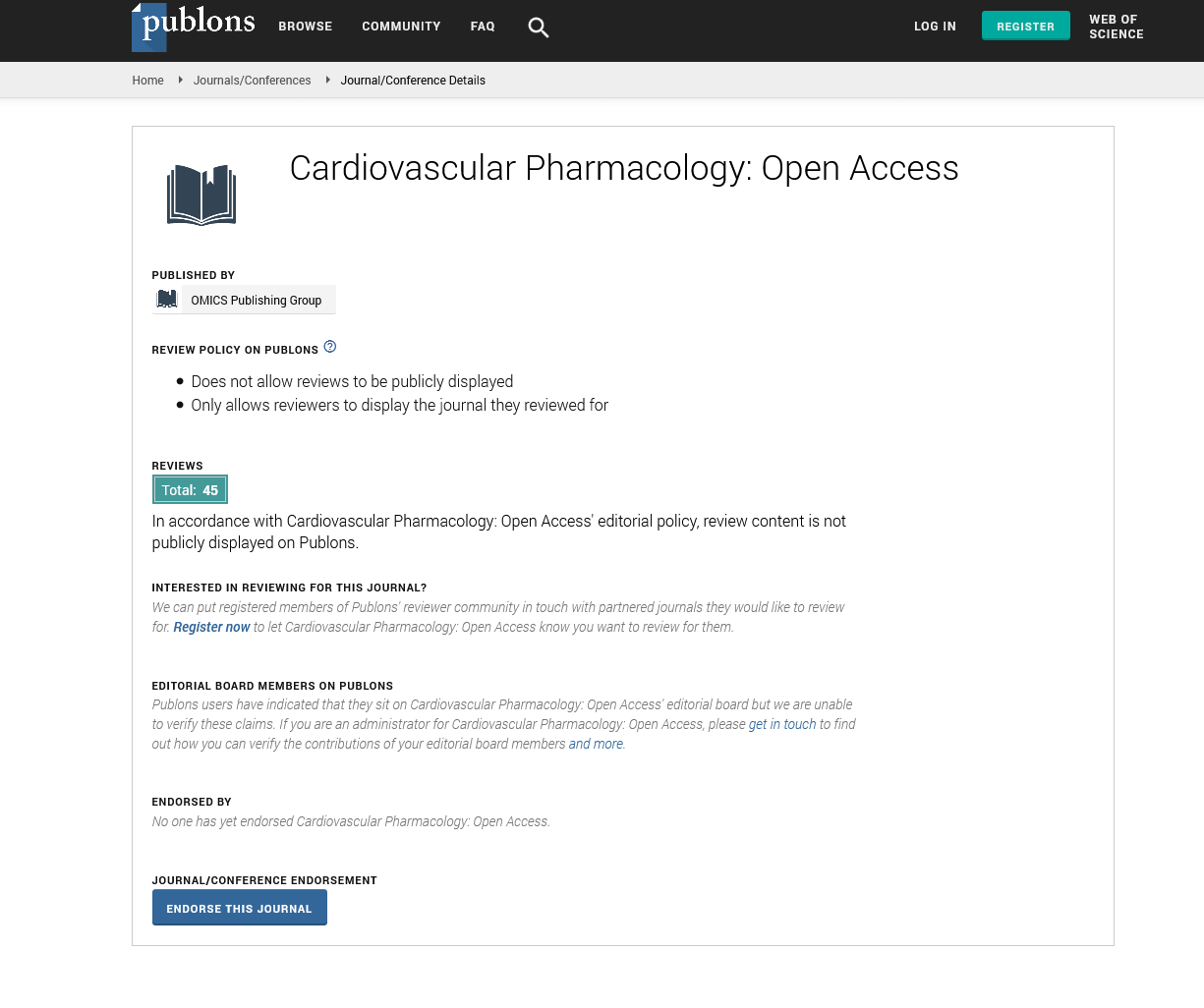
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
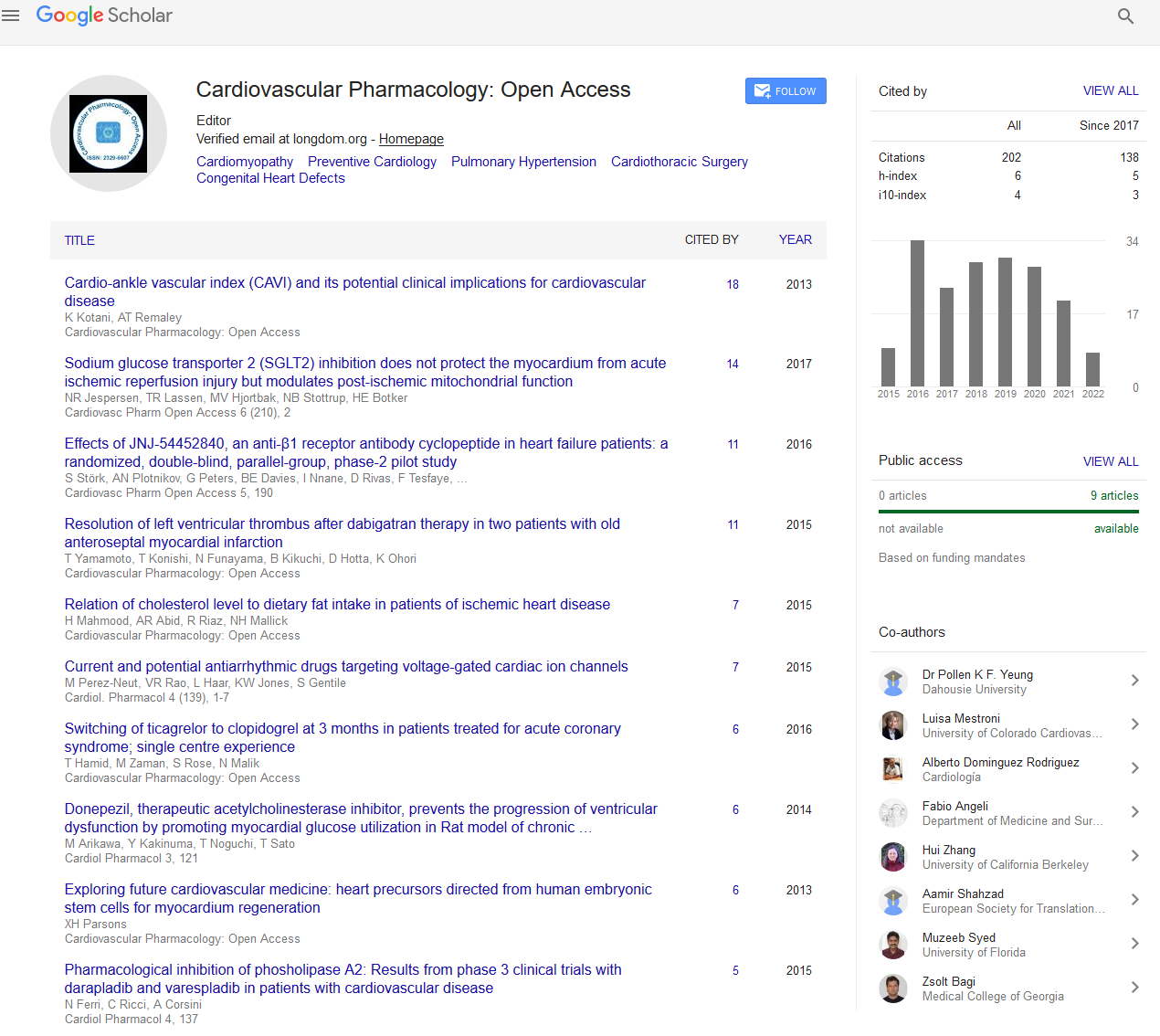
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Uptake and outcomes of multidisciplinary team (MDT) decision making approach for patient undergoing elective coronary revascularization in a tertiary cardiology center
Joint Event on Heart Failure, Pediatric Cardiology & Nursing Education
February 18-19, 2019 | Amsterdam, Netherlands
Fatima Bangash, Rosemary Grain, Karthik Chandrasekharan and Andrew Wragg
St. Bartholomew‚??s Hospital, UK
Posters & Accepted Abstracts: Cardiovasc Pharm Open Access
Abstract:
Background: Decisions regarding the preferred revascularization options for elective patients with complex coronary artery disease (CAD) i.e. left main stem, chronic total occlusion (CTO) or multi-vessel can be challenging especially in patients with co-morbidities. Anatomic considerations are also important, and lesion location, severity and extent may influence decisions on revascularization. All such elective cases need to be presented to a dedicated MDT so that the most optimal therapy (including no intervention) can be considered. These meetings involve interventional cardiologist, surgeons and non-interventional consultant. Suggested benefits with these meeting include coordinated patient care, better communications between teams, and evidence-based approach with better transparency in decision making process and great platform for education and training. BCIS and ESC guidelines also support “heart team” approach for decision making regarding coronary revascularization. MDT meetings at St. Bartholomew’s Hospital occur twice weekly with electronic MDT database to discuss complex cases and this study looks into the uptake of these patients for these MDT meetings and assesses the outcomes.
Aims: The aims of this study were to evaluate uptake of patients for MDT meetings for discussion of all interventional and conservative options and to measure six monthly outcomes of these patients in terms of repeat revascularization, non-fatal MI and mortality.
Methods: The study evaluated decision making process of the coronary multidisciplinary team in a tertiary care center over a six-month period. Retrospective review of 200 patients who had elective angiogram and coronary artery by-pass grafting from 01 Feb 2018 was conducted and gathered data for six monthly outcomes on repeat revascularization, non-fatal myocardial infarction and mortality. Data on patient demographics, angiographic findings especially for involvement of left main stem disease, proximal left anterior descending artery lesions, CTO and triple-vessel disease and information on co-morbidities, left ventricular function and presence of valvular lesions were collected from the clinical notes and imaging studies.
Result: Out of the 195 patients who underwent elective coronary revascularization in Feb and March, 99 patients were in the PCI cohort and 96 patients in the CABG cohort. Uptake of the complex patients for MDT meetings was about 60%.
Conclusion: MDT approach is a great treatment strategy for patient assessment and management. This study provides useful information on the uptake of complex patients for MDT decision making approach. However, there is limited evidence on the impact on survival outcomes. This study helps in identifying areas to improve the uptake of patients for these MDT discussions. Future studies are required to assess the impact of MDT on patient satisfaction and quality of life.