Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
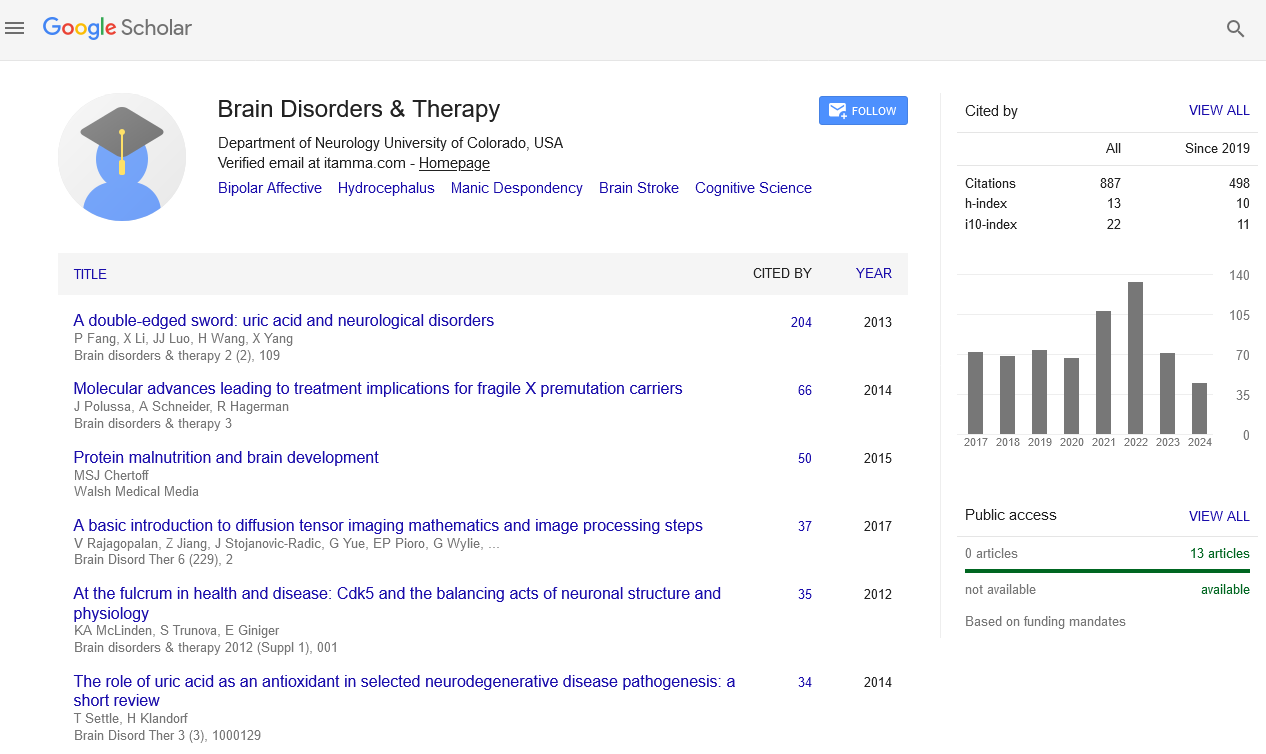
- Publons
- Geneva Foundation for Medical Education and Research
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Inhibition of monocyte recruitment does not impair recovery from traumatic brain injury in mice treated with granulocyte colony- stimulating factor
Joint Event on 3rd International Conference on Neuropsychiatry and Sleep Medicine & 8th International Conference on Neurology and Brain Disorders
September 21-22, 2018 | Philadelphia, USA
Shijie Song
James A Haley VAH Research Service, University of South Florida, USA
Posters & Accepted Abstracts: Brain Disord Ther
Abstract:
Introduction: Granulocyte colony-stimulating factor (G-CSF) has direct effects on brain in addition to its well know stimulation of hematopoiesis. To further understand the mechanisms for the beneficial effects of G-CSF in models of TBI, the present study was designed to determine the extent to which recruitment of bone marrow-derived cells (BMDC) from the blood into the brain is responsible for enhanced recovery from TBI. Methods: Chimeric mice were prepared from C57BL/6 mice transplanted with green fluorescent protein-expressing (GFP+) bone marrow. GFP+ leukocytes that infiltrate the brain and differentiate into microglia were visualized and measured with immunofluorescence microscopy. A selective chemokine receptor antagonist RS504393 (Tocris, Inc) of monocyte chemoattractant protein-1 (MCP-1) was administered to inhibit infiltration of monocytes into the CNS. Animals underwent controlled cortical impact on the right side of the brain. The behavioral endpoint was a performance in the radial arm water maze (RAWM). Hippocampal neurogenesis was determined by analysis of Doublecortin (DCX) expression by new-born neurons. Results: Two weeks after TBI, the cohort of mice treated with G-CSF exhibited a six- and a three-fold increase in GFP+ signal, respectively, in the right frontal cortex and striatum. G-CSF also increased microglial activation in those regions. Co-administration of the CCR2 antagonist (0.5 and 2.0 mg/kg) blocked infiltration of GFP+ to both cortex and striatum. However, CCR2 antagonist co-administration with G-CSF did not prevent improved performance associated with G-CSF treatment. G-CSF treatment, with or without CCR2 antagonist co-administration, triggered an increase in hippocampal DCX expression, a marker of immature neurons. Unexpectedly, the CCR2 antagonist administered alone at the low dose also significantly increased hippocampal neurogenesis (p<0.05). Summary: In conclusion, the present study supports the hypothesis that the direct action of G-CSF on neural cells, independent of its hematopoietic effects, is primarily responsible for enhanced recovery from TBI. In addition, this study confirms the importance of CCR2 and its ligand MCP-1 in mediating the inflammatory response following TBI. More importantly, administration of a drug that blocks MCP-1 actions (without the need for co-administration of G-CF) appears to be enough to enhance recovery of cognitive performance in the RAWM. Going forward, it will be important to study the mechanism by which mitigation of the inflammatory response, by interfering with chemokine signaling, results in stimulation of hippocampal neurogenesis.
Biography :
E-mail: ssong@health.usf.edu