Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
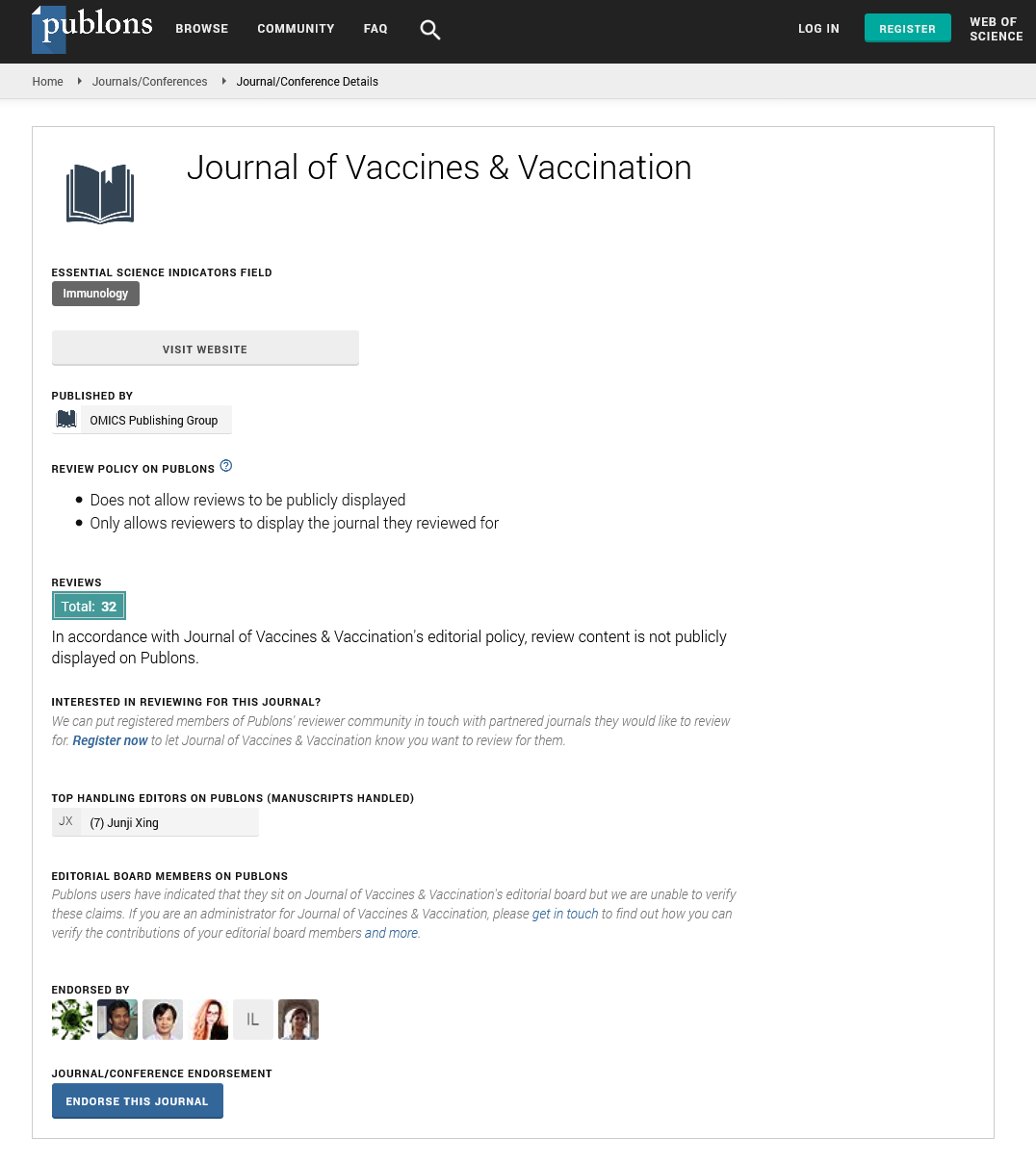
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Development of an anti-bath salt vaccine using a microparticulate delivery system
Joint Event on 32nd International Conference on Vaccines and Immunization & 4th Annual Summit on Infancy, Child Nutrition & Development
November 09-10, 2018 | Atlanta, USA
Keegan Braz Gomes, Kevin Murnane and Martin J D Souza
Mercer University, USA
Scientific Tracks Abstracts: J Vaccines Vaccin
Abstract:
Introduction: Drug addiction is a serious epidemic in the United States, resulting in over thousands of deaths a day. In recent years, there has been an increased prevalence of individuals turning to synthetic cathinones or ???bath salts??? because they are often marketed as cheap substitutes to more expensive drugs such as cocaine and methamphetamine. Hence, to combat this health issue, an anti-stimulant microparticulate vaccine is proposed. In the past, microparticulate systems have been shown to enhance and prolong adaptive immunity when used to delivery vaccines. The vaccine will be formulated to target a synthetic cathinone, alpha-pyrrolidinopropiophenone (?-PPP), therefore resulting in the body building up an adaptive immunity to the drug. Therefore, a microparticulate system was developed and tested to determine whether it could be safe and efficacious in potentially delivering an anti-stimulant drug vaccine in the future. Method: A microparticulate matrix was formulated by crosslinking BSA overnight with gluteraldehyde. Unreacted gluteraldehyde was neutralized before adding the surfactant, Tween 80, and the drug, ?-PPP, at 10% loading. Next, the formulation was spray dried using a Buchi Spray Dryer apparatus. Physiochemical characterizations of the microparticles such as shape, charge, and size were then assessed. A nitric oxide assay was then carried out to qualitatively determine the immunogenicity of the blank and vaccine particles in vitro. For the vivo study, 17 Swiss Webster mice were divided into the following groups: 1) Drug MP (?-PPP drug in microparticles) 2) Blank MP (blank microparticles) and 3) Control (saline). For all microparticle groups, the particles were suspended in saline with tween and administered subcutaneously at Week 0 (prime), Week 3 (booster #1), Week 6 (booster #2), and Week 29 (booster #3). The Control group received only saline for the same timeline listed prior. Concurrent with receiving their respective treatments, each mouse was administered a range of doses (mg/kg) of ?-PPP: 18, 30, 56, 78, and 100 mg/kg (over several weeks) and placed in an Open Field monitoring locomotor system with light beam arrays in the X, Y and Z axes. The Open Field monitoring system recorded many components of locomotor activity. For locomotor analysis, peak activity (in response to drug) of each mouse was recorded as well as activity over an extended period using parameters such as ambulatory, stereotypic, and vertical counts. The results were then used to extrapolate trends and statistical differences between the groups. Psychosis behavior was also observed with a 78 mg/kg dose through the use of a video camera. Results: The microparticles produced were on average 3 um in diameter with a negative zeta potential. Additionally, it was determined that the microparticle matrix (for both MP groups) itself was not immunogenic. In vivo, after establishing the dose response curve in all the mice, the effects of ?-PPP in different groups were extrapolated. Within the control, a typical ambulatory peak dose-effect curve was observed for the range of doses. It was also observed that the peak activity for the Control group at 56 mg/kg was only slightly different than the peak activity of the Blank MP and Drug MP groups, which was seen at 30 mg/kg. Additionally, ambulatory, vertical, and stereotypic counts were compared across multiple doses. Also, the groups showed similar psychosis at higher doses. Conclusion: Therefore, it was determined that the microparticulate delivery system is an appropriate approach for potentially delivering an anti-?-PPP vaccine. This is primarily due to the lack of significant differences in the behavioral outcomes between the groups which did and do not receive the microparticulate system treatment. Hence, the microparticulate system with encapsulated drug does not alter the behavior or produce any atypical or adverse affects in the mice when concurrently administered with pure drug. Therefore, this safety assessment will aid in developing this formulation into an anti-?-PPP vaccine in the future for conjugating ?-PPP to a BSA carrier, encapsulating it into a microparticulate matrix, and then administering it to treat addiction to the drug.
Biography :