Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
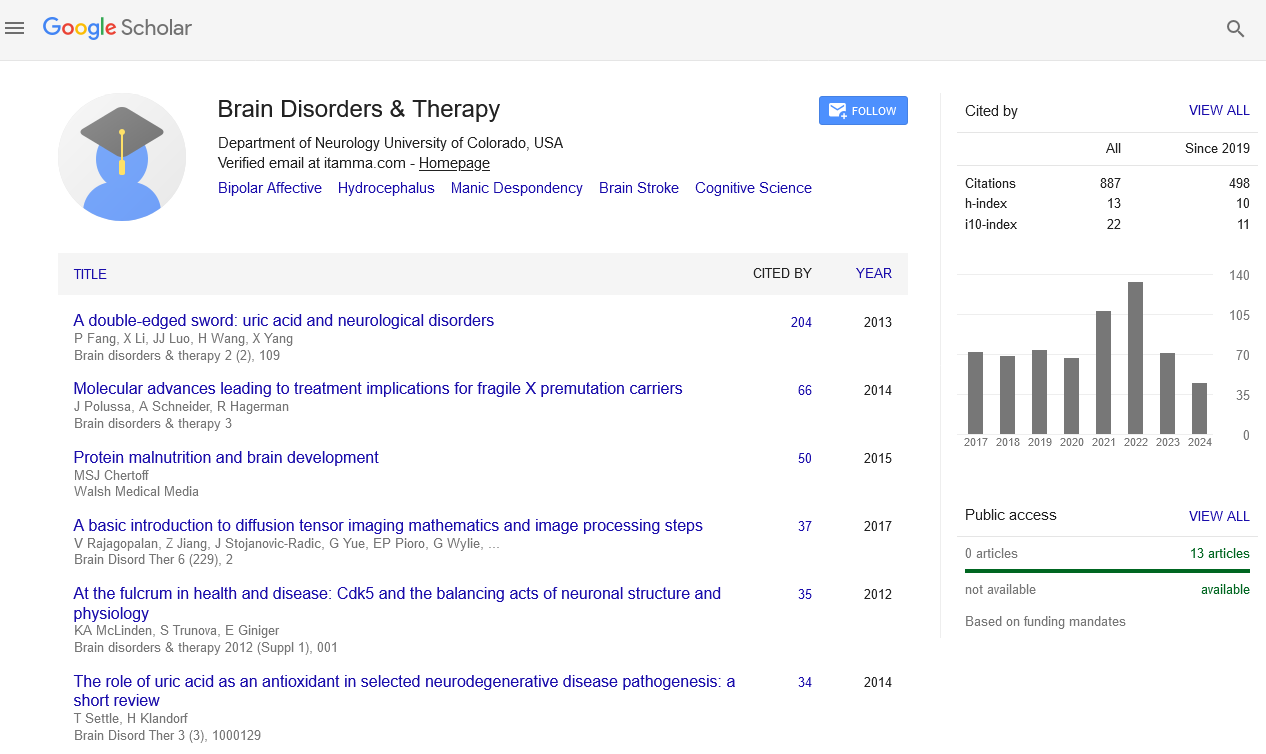
- Publons
- Geneva Foundation for Medical Education and Research
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Body dysmorphic disorder
2nd International Conference on Brain Disorders and Therapeutics
Chicago, USA October 26-28, 2016
Amir Mufaddel
Al Ain Hospital, UAE
Scientific Tracks Abstracts: Brain Disord Ther
Abstract:
Background: Body Dysmorphic Disorder (BDD) is a relatively common psychiatric disorder characterized by preoccupations with perceived defects in physical appearance. Objectives: This review aimed to explore epidemiology, clinical features, co morbidities and treatment options for BDD in different clinical settings. We reviewed the literature written between 1985 and 2012 using the key words body dysmorphic disorder, dysmorphophobia, Psychodermatology. Results: BDD occurs in 0.7%â??2.4% of community samples and 13% of psychiatric inpatients. Etiology is multi-factorial with recent findings indicating deficits in visual information processing. There is considerable overlap between BDD and Obsessive Compulsive Disorder (OCD) in symptoms etiology and response to treatment which led to suggestions that BDD can be classified with anxiety disorders and OCD. A recent finding indicated genetic overlap between BDD and OCD. Over 60 % of BDD patients had a lifetime anxiety disorder, 38% had social phobia which tends to predate the onset of BDD. Studies reported a high level of co-morbidity with depression and social phobia occurring in >70% of BDD patients. BDD individuals present frequently to dermatologists (about 9%â??14% of dermatologic patients have BDD). BDD co-occurs with pathological skin picking in 26-44.9% of cases. BDD has currently two variants: delusional and non-delusional and both variants respond similarly to Serotonin Reuptake Inhibitors (SRIs) which may have effect on obsessive thoughts and rituals. Cognitive behavioral therapy (CBT) has the best established treatment results. Conclusion: A considerable overlap exists between BDD and other psychiatric disorders such as obsessive compulsive disorder (OCD), anxiety and delusional disorder and this comorbidity should be considered in evaluation, management and long term follow up of the disorder. Individuals with BDD usually consult dermatologists and cosmetic surgeons rather than psychiatrist. Collaboration between different specialties (such as primary care, dermatology, cosmetic surgery and psychiatry) is required for better treatment outcome.
Biography :
Amir Mufaddel has graduated from Khartoum University and did his MD in Psychiatry from Sudan Medical Specialization Board in 2008. Currently he is working in Al Ain Hospital, Community Mental Health Services. He is also an Adjunct Lecturer in United Arab Emirates University. He has published several papers in reputed journals mostly reflecting the psychiatric aspects of physical conditions such as neurology, infectious diseases and dermatology.
Email: khalifaamir@yahoo.co.uk