Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
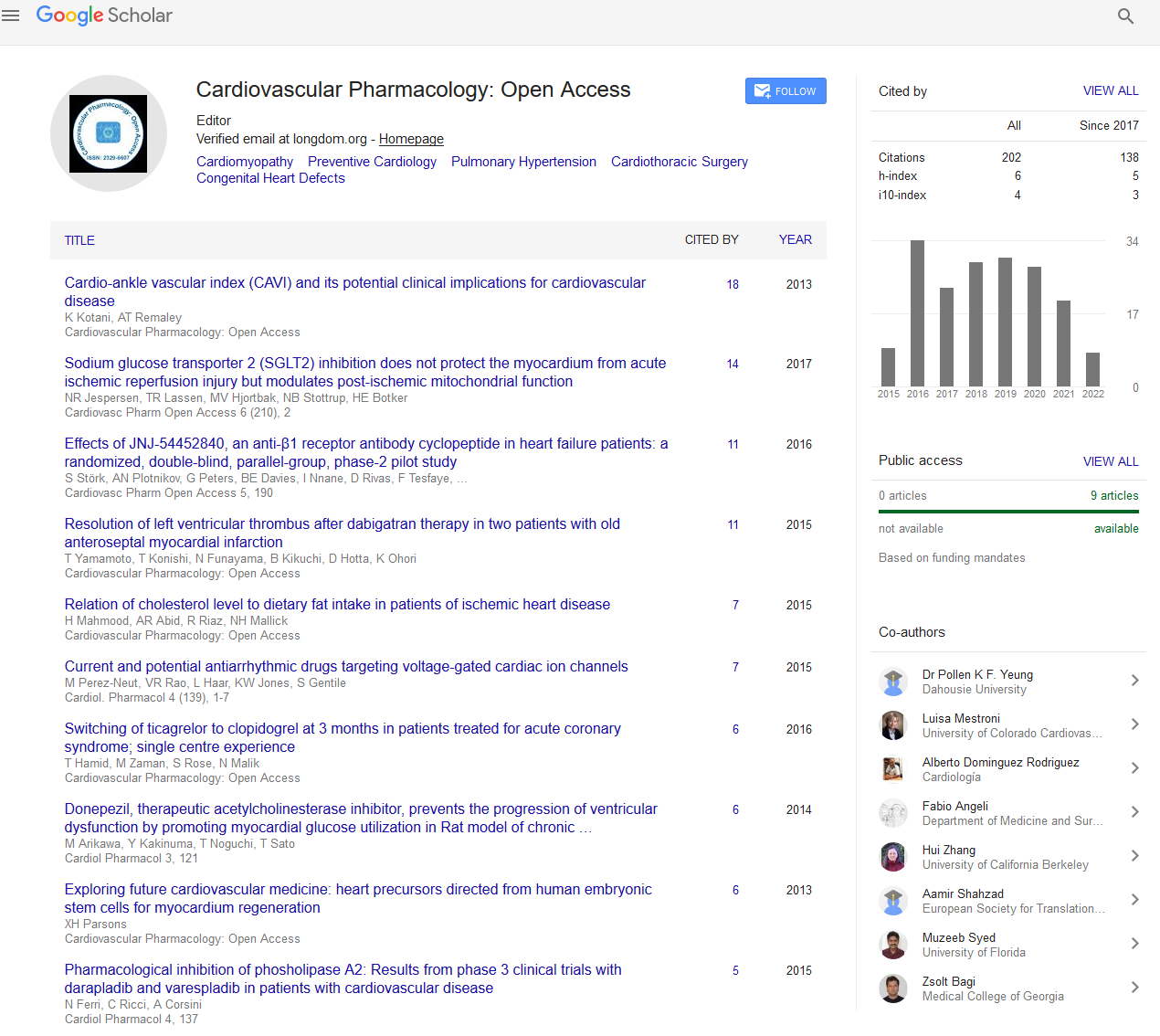
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
A sick rhythm alerts onset of serious vascular disease
15th International Conference on Pediatrics and Pediatric Cardiology
February 19-20, 2018 | Paris, France
Guillermo Torres Viera
University of Puerto Rico, Puerto Rico
Scientific Tracks Abstracts: Cardiovasc Pharm Open Access
Abstract:
Early detection of cardiac allograft vasculopathy (CAV) presents a challenge to pediatricians since symptoms of myocardial ischemia (e.g., classic angina pectoris symptoms) are typically absent or atypical. Although rhythm disturbances are related to CAV, Sick Sinus Syndrome (SSS) remains an elusive sign of vasculopathy. An 18 year old male with history of heart transplant in 2011 secondary to myocarditis and associated dilated cardiomyopathy, presented to our pediatric emergency room due to chest tightness and shoulder pain on exertion without associated fevers, cough, leg swelling, or increased abdominal girth. Cardiac enzymes and electrocardiography (ECG) performed at that time were found within normal limits and patient was discharged home. Three days later, patient awoke from sleep with shortness of breath and dizziness, stating episodes of slow beats and near-syncope during the previous days precipitated during hot showers. He returned to ER where cardiac monitoring placed and noted with tachycardia/ bradycardia paroxysms without ST segment changes on ECG. BNP and panel reactive antibodies were sent and found elevated, therefore patient was transferred to Cardiovascular Center for suspected transplant rejection, allograft vasculopathy, and associated sick sinus syndrome. He was taken to cardiac angiography which revealed severe (>90%) stenosis of multiple segments of right coronary artery requiring bare-metal stent placement with immediate evidence of appropriate revascularization. SSS is defined by ECG abnormalities (e.g., bradycardia, sinus pauses, sinus arrest) that occur in association with clinical signs and symptoms. It should be widely recognized and alarm primary physicians of serious underlying vasculopathies, particularly in the pediatric population
Biography :
Guillermo Torres Viera is a Medical Resident in the Combined Internal Medicine-Pediatrics Residency Program of the University of Puerto Rico School of Medicine. He has completed his MD at the University of Puerto Rico in 2014 and entered the first class of this combined specialty program to be created in Puerto Rico for the advancement of knowledge and skill in the effective transition from youth to adulthood. He is currently also pursuing his Masters in Clinical and Translational Research focused towards the identification and prevention of early-onset cardiovascular disease