Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Special Issue - (2020) Volume 0, Issue 0
Virological Profile of Acute Respiratory Infections in Children at Dakar CHU
Ba ID1*, Diagne G1, Diallo AI2,3, Dia N4, Fall E4, Mbaye A1, Kane A1, Coundoul AM1, Sow S1, Bop K1 and Ndiaye O12Department of Preventive Medicine and Public Health, Albert Royer National Children's Hospital in Dakar, Dakar, Senegal, West Africa
3Institute for Health and Development, Albert Royer National Children's Hospital in Dakar, Dakar, Senegal, West Africa
4Department of Microbiology of The Laboratory of the ¨Pasteur de Dakar Institute, Albert Royer National Children's Hospital in Dakar, Dakar, Senegal, West Africa
Received: 16-Oct-2020 Published: 06-Nov-2020
Abstract
Introduction: Acute respiratory infections (ARIs) are a global public health priority. They are the leading cause of morbidity and mortality in children, especially in developing countries. The main objective of this study was to see mainly the virological aspects in ARI in children in Senegalese hospitals
Methodology: We had conducted a prospective descriptive mono-centric study over a period of one year (from July 01, 2017 to June 30, 2018) at the Albert Royer National Children's Hospital in Dakar.
Results: The hospital frequency for acute respiratory infections in children was 3.7%. The average age was 23.7 months with extremes between 1 month and 144 months. The peaks of consultations were found in August, March and April with respectively 22%, 15.6% and 12.8%. Fever, respiratory distress and pulmonary condensation syndrome were the main signs found on examination in our patients. Virologic tests were positive in 80.7%. The viruses most frequently found in the samples were the Rhinovirus in 33% of the samples, the respiratory syncytial virus in 24.8% and the coronavirus in 15.6%. Among the diagnoses retained, pneumonia was predominant and found in 61 of the cases, or a prevalence of 59.9%, followed by acute bronchiolitis with a prevalence of 16.51%. The average length of hospital stay was 10 days.
Conclusion: Acute respiratory infections in children are still a public health problem in developing countries; children under the age of five years are the most affected, hence the need to strengthen programs to fight ARI. The identification of germs is essential in the treatment and epidemiological surveillance in our regions.
Keywords
Respiratory infections; Child; Virology; Senegal
Introduction
Acute Respiratory Infections (ARI) is a public health priority around the world. They are the main cause of morbidity and mortality in children under five (05) years old, especially in developing countries, behind neonatal causes [1]. The majority of deaths occur in low-income countries [2,3]. The etiologies are multiple (bacteria, viruses, parasites or fungi). The diagnosis of bronchopulmonary infections requires extreme rigor of semiological, clinical and radiological analysis.
The main objective of this study was to identify the main viruses found in acute respiratory infections in children.
The secondary objectives were to describe the epidemiological, diagnostic and progressive aspects of ARI in children hospitalized at Albert Royer hospital in Dakar.
Methodology
This was a single-center descriptive prospective study over a period of one year (from July 01, 2017 to June 30, 2018), carried out at the Albert Royer National Children's Hospital (CHNEAR) in Dakar. We included children aged 0 to 15 years hospitalized for a respiratory symptomatology associated with a fever or a history of fever progressing for less than ten (10) days who had received a nasopharyngeal swab to allow viral research using the multiplex PCR technique.
Acute respiratory infection is defined by the presence of fever associated with respiratory symptoms (cough and/or dyspnea and/or pleuropulmonary examination abnormalities) evolving less than ten (10) days before admission. All incomplete files and non-compliant samples were excluded from the study.
The studied parameters were epidemiological, clinical, paraclinical especially virological, therapeutic and evolutionary. Data were collected and analyzed with Epi Info software version 7.2. A p<0.05 is considered significant.
Results
During the study period 2946 patients were hospitalized. The hospital frequency of ARI was 3.7% or 109 patients. The sex ratio was 1.8. The average age of the children was 23.7 months. Of these children, 55.1% came from the urban area. The peaks of consultations were found during the months of August, March and April with 22%, 15.6% and 12.8% respectively. The entire study population had been fully immunized according to the expanded immunization program underway in Senegal. The co-morbidities found were malnutrition in 3 cases, heart disease in 4 cases, sickle cell disease in 1 case and asthma in 5 cases. The reasons for consulting our patients were fever in 94.5% of cases, cough in 94.5% and rhinitis in 52.3% of cases as shown in Figure 1.
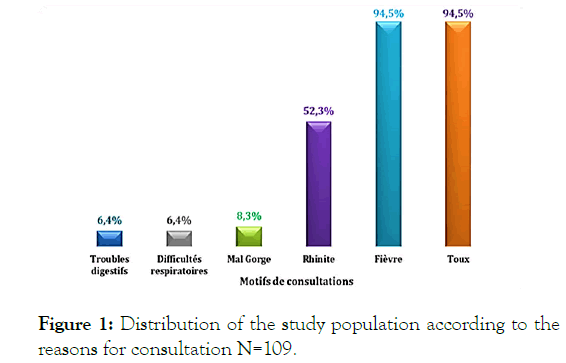
Figure 1: Distribution of the study population according to the reasons for consultation N=109.
The complete blood count carried out in all the children revealed hyper leukocytosis predominantly in 73.4% of the population. Age distribution of hemoglobin confirmed anemia in 55% of children.
Thrombocytopenia was found in 7 children. The C-reactive protein was positive in 97.3% of cases with an average of 96 mg/l. The multiplex PCR technique was used to analyze nasopharyngeal swabs and allowed us to identify the viruses responsible for these ARIs
The majority of virological tests were positive in 80.7% of samples (i.e. 88 samples). Among them, samples showing a single virus were predominant with 59.1%. The numbers of viruses present per sample were shown in Figure 2.
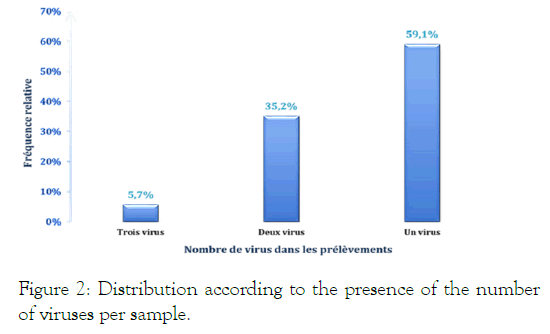
Figure 2: Distribution according to the presence of the number of viruses per sample.
The viruses most found in the samples were the Rhinovirus in 33% of the samples, the respiratory syncitial virus in 24.8% and the coronavirus (HKU1 and OC43) in 15.6% (Table 1).
| Diagnostic Virologique | Effectif (n) | Pourcentage (%) |
|---|---|---|
| Rhinovirus | 36 | 33,0 |
| VRS | 27 | 24,8 |
| Coronavirus (hku1et oc43) | 17 | 15,6 |
| Influenza A et B | 13 | 11,9 |
| Papillomavirus 1 et 3 | 13 | 11,9 |
| Adénovirus | 11 | 10,1 |
| Bocavirus | 6 | 5,5 |
| Entérovirus | 5 | 4,6 |
| Parechovirus | 2 | 1,8 |
| Métapneumovirus | 1 | 0,9 |
Table 1: Breakdown according to the presence of virus in the samples.
The distribution of the different viruses according to the months of consultation was shown in Figures 3 and 4.
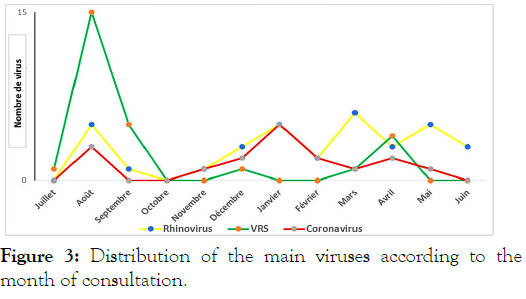
Figure 3: Distribution of the main viruses according to the month of consultation.
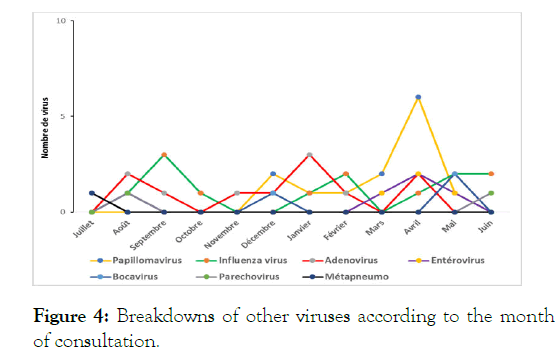
Figure 4: Breakdowns of other viruses according to the month of consultation.
From a diagnostic standpoint, the main diagnoses found were pneumonia, which was found in 56% of cases, followed by acute bronchiolitis which was found in 31%.
On the therapeutic level, antibiotic therapy was administered in 58.7% of the study population, i.e. 64 children, corticosteroid therapy was administered in 39.5%, oxygen therapy in 34.9% and physiotherapy in 15, 6%. The average length of hospital stay was 10 days; the main complications noted were atelectasis in 04 cases. The outcome was favorable in 98.2% (or 107 cases). The lethality was 1.8% (or 2 cases).
Discussion
The prevalence found in our study is relatively low. Higher prevalence is found in other countries in sub-Saharan Africa. In the Democratic Republic of Congo, Ngombé [4] in 2014 found a hospital prevalence of 26.11% high and low ARI. In Congo, Moyen [5] noted 19.8%. In the West, in Brazil in 2008, Prietsch [6] reported a community prevalence of 23.9% of low ARI in children under 5 years old.
In North America, an incidence of 30 to 45 cases per 1000 in children under 05 years and 6 to 12 cases per 1000 in children over 5 years [7]. The average age of our children was 23.7 months. Superimposable mean ages have been described by other authors [8].
Acute respiratory infections can occur at any age. Young children, particularly those under the age of 5, are the most vulnerable [9]. This justifies the fact that most of the global infant morbidity and mortality programs focus on this age group. The vulnerability of this age group is believed to be linked to the immaturity of their immune system and the nasopharyngeal carriage of certain germs [10]. In our study, children under 5 represent 88% of the total workforce.
The sex ratio 1.8 was largely in favor of boys. This male predominance is described by most authors both in Senegal and in the world. Krishnan, in 2012 in India found a frequency of hospitalizations for ARI in boys 2.4 times higher than in girls [11].
Our study shows an uneven distribution between the months of hospitalization with peaks in the occurrence of ARIs during the months of March and April, corresponding to the period of transition between coolness and the period of high heat. This climate favors ENT infections, which weakens the respiratory mucosa and facilitates the spread of germs. During this period we also note phenomena of particulate pollution (PM10 and PM2.5) linked to the wind coming from the Sahara desert [12].
In addition, a significant peak was observed in August (with 22%) in our series. We have no plausible explanations because during this period the particulate phenomenon fades with the rainy season. It could be the effect of humidity. Studies are needed to assess the impact of climatic factors (humidity, temperature, etc.) on the occurrence of ARI.
In developed countries, a seasonal distribution of ARIs is noted especially in the fall and winter [13,14].
All of our patients had received a nasopharyngeal swab which had been studied using the multiplex PCR technique. This technique (viral RNA transcribed into DNA, and then the DNA of the different pathogens is amplified simultaneously in the same tube by Fast-tract® PCR, multiplex) allowed us to isolate viruses. This technique was positive in 100% of cases.
Virologically, multiplex PCR isolated one or more viruses in 88 samples (i.e. a positivity rate of 80.7%).
Lower detection rates are reported: 28.5% in India by Mummidi [15] and 24% in Saudi Arabia by Albogami [16].
In the majority of cases, viral mono-infection was found in 52 cases, ie 59.1% of cases and co-infection in 40.9%. This same profile has been found in several studies. In Central Africa, Bobossi [17] in his series (using the same technique) found this mono-infection in 92.1%.
The main viruses found in our children were rhinovirus in 33% of cases followed by RSV in 24.8% and coronavirus in 15.6%. The influenza virus (Influenza A and B) accounted for 11.9%. In 2016, Tran found in Vietnam a predominance of Rhinovirus in 30%, followed by RSV in 23.8% and Bocavirus in 7.2% [18]. In this same work, he noted a predominance of RSV during the rainy season, as the rhinovirus occurred and was detected throughout the year. This finding is similar to ours where we noticed peaks of RSV during the rainy season.
The results of the 5S network surveillance also show that peak RSV cases in Senegal occur mainly during the rainy season [19]. This probably explains the fact that we find cases of bronchiolitis throughout the year, particularly during the rainy season.
In temperate countries, viruses are the leading cause of ARI in children under 5 years old. RSV is the main virus found with seasonality in winter and autumn [8], i.e., during the period of freshness.
In fact, in the series by Fraymouth [5] in France, RSV was found in 64.1%, followed by rhinovirus (26%) and metapneumovirus.
In Saudi Arabia RSV was the most predominant with peaks from December to February [1].
In addition, our results show a viral co-infection in 40.1%. This could be explained by the carriage of certain viruses such as the rhinovirus which is found throughout the year. Other authors like Nitsch have reported cases of coinfection in the literature [20].
Death was found in two (2) children or 1.8% of cases and this can be explained by the fact that his children presented a severe sepsis picture with multiple organ failure.
In Africa our death rate remains lower compared to that of Moyen el al in Congo Brazzaville (16.25%), and that of Bakondé 7.5% in Togo [21].
Conclusion
Childhood Acute Respiratory Infections (ARIs) are a major contributor to morbidity and mortality in children under five in Senegal and around the world, despite WHO guidelines in the management of ARI the child.
This study is a first and allowed us to know the virological profile of ARIs in children hospitalized in our structure.
REFERENCES
- Albogami SS, Alotaibi MR, Alsahli SA, Masuadi E, Alshaalan M. Seasonal variations of respiratory viruses detected from children with respiratory tract infections in Riyadh, Saudi Arabia. J Infect Public Health. 2018;11(2) :183-186.
- Bakonde B, Tatagan K, Kessie K, Kafechina ABL, Assimadi K, Paupe J. Epidémiologie hospitalière des infections respiratoires aigües (ira) basses chez le nourrisson et l’enfant togolais. Médecine d’Afrique Noire. 1998;45(7):435-439.
- Bobossi G, Gody JC, Fioboy R, Nakoune E. Viral etiology of acute respiratory infections in children in Bangui. Arch Pediatr .2015;22(3):324-325.
- Boyd K. Back to the Basics: Community-Acquired Pneumonia in Children. Pediatr Ann 2017;46(7):257-261
- Freymuth F, Vabret A, Dina J, Nimal CD. Les virus des bronchiolites aiguës. Archives de Pédiatrie 2010;17(8):1192-201.
- Krishnan A, Amarchand R, Gupta V, Lafond KE, Suliankatchi RA, Saha S. Epidemiology of acute respiratory infections in children: Preliminary results of a cohort in a rural north Indian community. BMC Infect Dis. 2015;15:462.
- Leowski J. Mortality from acute respiratory infections in children under 5 years of age: Global estimates. World Health Statistics Quarterly 1986;39(2):138-144.
- Leung AKC, Wong AHC, Hon KL. Community-Acquired Pneumonia in Children. Recent Pat Inflamm Allergy Drug Discov. 2018; 12(2):136-144.
- Levels and Trends in Child Mortality, Report 2014. United Nations Inter-Agency Group for Child Mortality Estimation. UNICEF, WHO, The World Bank, United Nations Population Division. New York. 2014.
- Moyen E, Kambourou J, Okoko AR, Nguelongo LB, Bomel VB, Nkounkou KG, et al. Child Acute Lower Respiratory Tract Infection in Pediatrics Intensive Care Unit at University Hospital of Brazzaville (Congo). Open Journal of Pediatrics 2018;8(1):32-41.
- Mummidi PS, Trpathy R, DwibediB, Mahapatra A, Baraha S. Viral aetiology of wheezing in children under five.Indian J Med Res. 2017;145(2):189-193.
- Ba I, Drame MS, Diagne G, Ndiaye T, Fall AL, Faye PM, et al. Impact of particulate pollution (PM10 and PM2.5) on the occurrence of cases of acute exacerbations of childhood asthma Albert Royer hospital in Dakar. Respiratory Disease Review. 2019;36:A63-A64.
- Ngombe LK, Mbombo D, Kameya N, Malingo AA, Kayomb NK, Ngolomba JN, et al. Acute respiratory infection and nutritional status in children 0-5 years: Case of university clinics of Lubumbashi, Democratic Republic of Congo. Pan Afr Med J. 2014;19:393.
- Nitsh OA, Kuchar E, Cabanek TA, Wardyn K, Życińska K, Brydak L, et al. Incidence in clinical course of respiratory viral coinfections in children aged 0-59 months. Adv Exp Med Biol. 2016;905:17-23.
- O’Leary. Defining normal ranges and centiles for heart and respiratory rates in infants and children: A cross sectional study of patients attending an Australian tertiary hospital pediatric emergency department. Arch Dis Child. 2015 ;100:733-737.
- Oliveira TG, Moraes JSB, Moreira FT, Arrelaro RC, Ricardi VA, Bertagnon JB, et al. Evaluation of hospitalization of children aged 0 to 5 years admitted for respiratory infections at a large hospital. Einstein (São Paulo). 2011;9(4):514-517.
- Prietsch SOM, Fischer GB, César JA, Lempek BS, Barbosa LV, Zogbi L, et al. Acute lower respiratory illness in under-five children in Rio Grande, Rio Grande do Sul State, Brazil: Prevalence and risk factors. Cad Saude Publica. 2008;24(6):1429-1438.
- Rasmussen Z, Pio A, Enarson P. Case management of childhood pneumonia in developing countries: Recent relevant research and current initiatives. Int J Tuberc Lung Dis. 2000;4:807-826.
- Stein RT, Marostica PJ. Community-acquired pneumonia: A review and recent advances. Pediatr Pulmonol. 2007;42(12):1095-1103.
- Thiam D, Niang M, Dia N, Sarr FD, Goudiab D, Senghor ML, et al. Strengthening of the influenza sentinel surveillance network in Senegal and results. Public Health. 2015;108 :21-24.
- Tran DN, Trinf QD, Pham NT, Vu MP, Ha MT, Nguyen TQN, et al. Clinical and epidemiological characteristics of acute respiratory virus infections in Vietnamese children. Epidemiol Infect. 2016;144(3):527-536.
Citation: Ba ID, Diagne G, Diallo AI, Dia N, Fall E, Mbaye A, et al. (2020) Virological Profile of Acute Respiratory Infections in Children at Dakar CHU. Clinics Mother Child Health. 17:367.
Copyright: © 2020 Ba ID, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

