Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2023) Volume 14, Issue 4
Unmasking Uncommon Melanoma Variants: Strategies for Accurate Diagnosis
Verche Todorovska*Received: 14-Aug-2023, Manuscript No. JCM-23-22594; Editor assigned: 16-Aug-2023, Pre QC No. JCM-23-22594(PQ); Reviewed: 31-Aug-2023, QC No. JCM-23-22594; Revised: 07-Sep-2023, Manuscript No. JCM-23-22594(R); Published: 14-Sep-2023, DOI: 10.35248/ 2157-2518.23.14.422
Description
The aim of this article is to improve the early detection and diagnosis of melanoma, ultimately increasing the survival rate for patients.
Melanoma is a potentially dangerous skin tumor responsible for 90% of all skin cancer-related deaths. If diagnosed and treated early survival rate is very high, almost 99%. Dermatoscopy is a diagnostic method enabling the detection of morphological chaos even in early-stage melanomas, long before it becomes clinically evident. “Chaos and Clues” is a decision-making algorithm designed for pigmented skin lesions, indicating biopsy in order to confirm or discard possible malignancy if there is chaos in one of 3 aspects (distribution of colors, patterns, and border abruptness) and at least one clue to malignancy [1]. The diagnosis seems feasible and easy. Nevertheless, some challenging melanomas exist and might be easily overlooked, displaying harmony of all 3 aspects, often resembling a wide range of benign tumors. In order to avoid missing a melanoma, we present a series of challenging cases and peculiar clinical scenarios but also provide solutions to overcome these diagnostic pitfalls:
When the lesion does not look like a melanoma-do sequential digital monitoring!
Chaos and clues can’t help us detect featureless melanomas, there are no clinical or dermoscopic clues present, and the lesion is indistinguishable from a nevus [2]. It can be recognized only by change over time, nevi are stable, and melanomas grow asymmetrically. Featureless melanomas can be caught only with sequential digital imaging/digital monitoring.
When all the lesions look like a melanoma-comparative approach is the answer!
One of the most difficult scenarios, is a patient with AMS, with multiple nevi showing suspicious features. We must apply the Comparative approach, to evaluate the lesions not individually but in the context of other nevi [3]. Only then we can confirm the suspicious features as repetitive and state with confidence that they are in fact atypical nevi. This leads to lower rates of unnecessary excisions, and by proceeding with short and longterm follow-up, detecting the real suspects.
When we don't see the lesion-undress your patients and make a thorough skin examination!
To recognize it, we must see it first! Undress your patients, do a total body skin examination, and tend to check even the hidden areas, in between the fingers, intergluteal areas, soles of the feet, retro auricular area, scalp covered with hairs, oral mucosa, and genitalia, if the patient refuses, ask him if he has spotted anything unusual on his skin recently. Only 30% of all dermatologists are doing the opportune screening. Figure 1 illustrates the importance of a thorough skin examination, regardless of the motive for the visit (Figure 1).
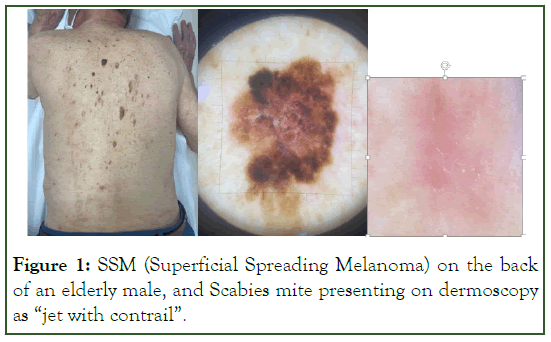
Figure 1: SSM (Superficial Spreading Melanoma) on the back of an elderly male, and Scabies mite presenting on dermoscopy as “jet with contrail”.
When the pathologist doesn't recognize it-apply the new standard for diagnosing skin cancer, integration of clinic, dermatoscopy, and pathology!
You must have in mind that pathology has its limits, there is very low interobserver agreement and a high level of subjectivity in assessing melanocytic lesions. Always evaluate the correlation of the pathology report with the dermatoscopy findings [4]. If they do not match ask for a second opinion or a revision with additional stainings. A nevoid melanoma (Figure 2), was initially reported as a Nevus with massive Ly infiltration. This emphasizes the importance of interdisciplinary collaboration between clinicians, dermatoscopists, and pathologists. Effective communication and sharing of information between these specialists are critical for accurate diagnosis and treatment (Figure 2).
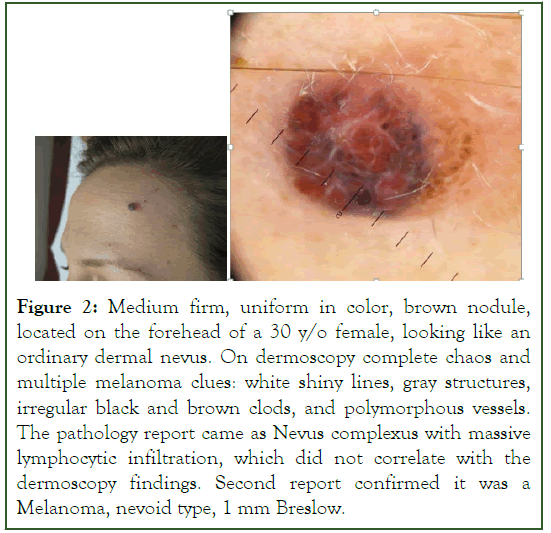
Figure 2: Medium firm, uniform in color, brown nodule, located on the forehead of a 30 y/o female, looking like an ordinary dermal nevus. On dermoscopy complete chaos and multiple melanoma clues: white shiny lines, gray structures, irregular black and brown clods, and polymorphous vessels. The pathology report came as Nevus complexus with massive lymphocytic infiltration, which did not correlate with the dermoscopy findings. Second report confirmed it was a Melanoma, nevoid type, 1 mm Breslow.
When it is an uncommon variant of melanoma-follow the rules and clues!
The uncommon melanomas are usually symmetric, lacking the classical melanoma criteria, often smaller than 6 mm, and might simulate a benign tumor [5,6]. In order to recognize them we must apply additional rules, already established based on multiple clinical studies and our experience. Figures 3-5 represent three cases of less common melanoma variants, and the rules applied that lead to the correct diagnosis (Figures 3-5).
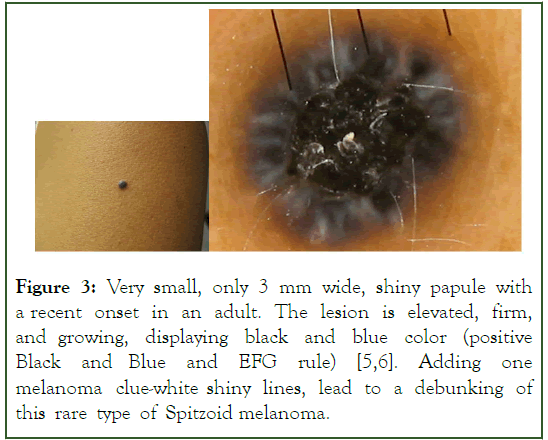
Figure 3: Very small, only 3 mm wide, shiny papule with a recent onset in an adult. The lesion is elevated, firm, and growing, displaying black and blue color (positive Black and Blue and EFG rule) [5,6]. Adding one melanoma clue-white shiny lines, lead to a debunking of this rare type of Spitzoid melanoma.
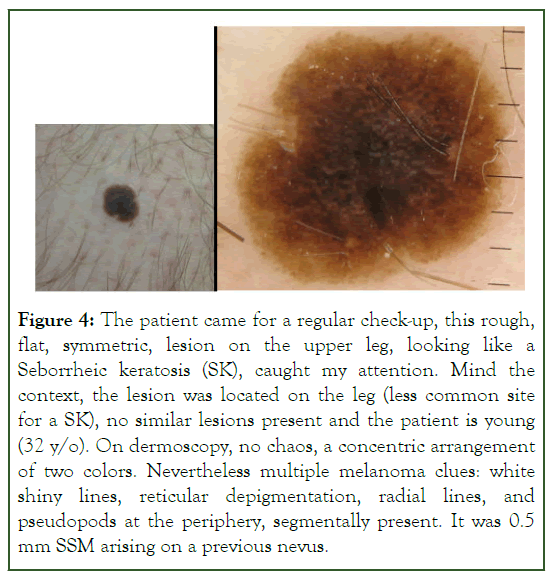
Figure 4: The patient came for a regular check-up, this rough, flat, symmetric, lesion on the upper leg, looking like a Seborrheic keratosis (SK), caught my attention. Mind the context, the lesion was located on the leg (less common site for a SK), no similar lesions present and the patient is young (32 y/o). On dermoscopy, no chaos, a concentric arrangement of two colors. Nevertheless multiple melanoma clues: white shiny lines, reticular depigmentation, radial lines, and pseudopods at the periphery, segmentally present. It was 0.5 mm SSM arising on a previous nevus.
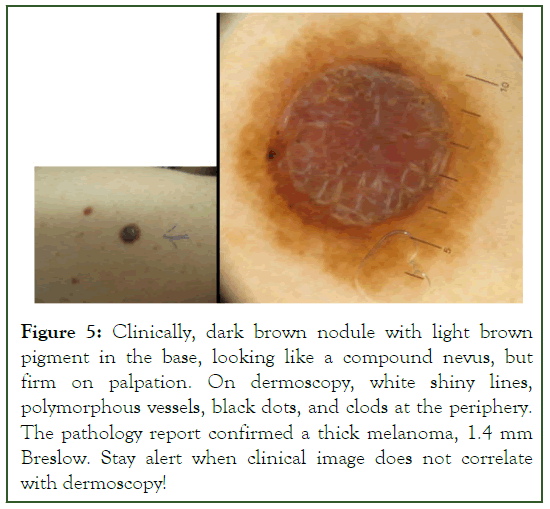
Figure 5:Clinically, dark brown nodule with light brown pigment in the base, looking like a compound nevus, but firm on palpation. On dermoscopy, white shiny lines, polymorphous vessels, black dots, and clods at the periphery. The pathology report confirmed a thick melanoma, 1.4 mm Breslow. Stay alert when clinical image does not correlate with dermoscopy!
We do acknowledge the limitations. Melanoma diagnosis can be complex, and some cases may still present challenges even with these approaches.
Conclusion
In conclusion, this article highlights the critical goal of enhancing early detection and diagnosis of melanoma to improve patient survival rates. It emphasizes the significance of dermatoscopy and the "Chaos and Clues" algorithm for identifying potential malignancies in pigmented skin lesions. The article also underscores the necessity of comprehensive approaches such as sequential digital monitoring, comparative evaluation, thorough skin examinations, and interdisciplinary collaboration among clinicians, dermatoscopists, and pathologists to address challenges posed by featureless melanomas, uncommon variants, and limitations in pathology interpretation. Implementing these solutions would help clinicians to overcome the most difficult diagnostic pitfalls and avoid missing the deadliest skin cancer.
References
- Rosendahl C, Cameron A, McColl I, Wilkinson D. Dermatoscopy in routine practice: Chaos and clues. Aust Fam Physician. 2012; 41(7):482-487.
[Google Scholar] [PubMed]
- Kittler H, Guitera P, Riedl E, Avramidis M, Teban L, Fiebiger M, et al. Identification of clinically featureless incipient melanoma using sequential dermoscopy imaging. Arch Dermatol. 2006; 142(9):1113-1119.
[Crossref] [Google Scholar] [PubMed]
- Argenziano G, Catricala C, Ardigo M, Buccini P, De Simone P, Eibenschutz L, et al. Dermoscopy of patients with multiple nevi: Improved management recommendations using a comparative diagnostic approach. Archives of dermatology. 2011; 147(1):46-49.
[Crossref] [Google Scholar] [PubMed]
- Soyer HP, Massone C, Ferrara G, Argenziano G. Limitations of histopathologic analysis in the recognition of melanoma: A plea for a combined diagnostic approach of histopathologic and dermoscopic evaluation. Arch Dermatol. 2005; 141(2):209-211.
[Crossref] [Google Scholar] [PubMed]
- Argenziano G, Longo C, Cameron A, Cavicchini S, Gourhant JY, Lallas A, et al. Blue-black rule: A simple dermoscopic clue to recognize pigmented nodular melanoma. Br J Dermatol. 2011; 165(6):1251-1255.
[Crossref] [Google Scholar] [PubMed]
- Pampena R, Lai M, Lombardi M, Mirra M, Raucci M, Lallas A, et al. Clinical and dermoscopic features associated with difficult-to-recognize variants of cutaneous melanoma: A systematic review. JAMA Dermatol. 2020; 156(4):430-439.
[Crossref] [Google Scholar] [PubMed]
Citation: Todorovska V (2023) Unmasking Uncommon Melanoma Variants: Strategies for Accurate Diagnosis. J Carcinog Mutagen. 14:422.
Copyright: © 2023 Todorovska V. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


