Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- The Global Impact Factor (GIF)
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
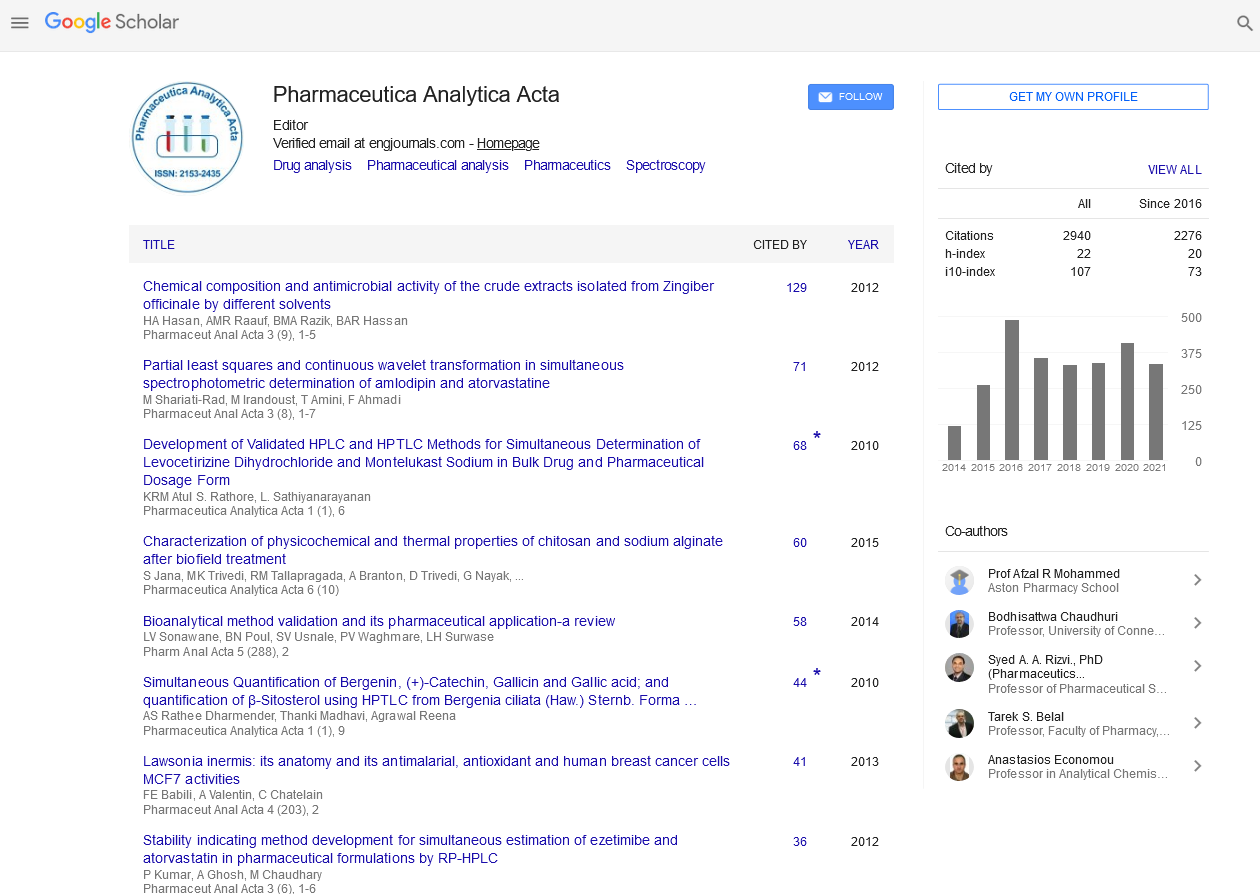
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentry - (2022) Volume 13, Issue 6
Sterilizing Process and Applications of Autoclave
Gee Szu*Received: 01-Jul-2022, Manuscript No. PAA-22-17348; Editor assigned: 05-Jul-2022, Pre QC No. PAA-22-17348 (PQ); Reviewed: 20-Jul-2022, QC No. PAA-22-17348; Revised: 28-Jul-2022, Manuscript No. PAA-22-17348 (R); Published: 05-Aug-2022, DOI: 10.35248/2153-2435.22.13.677
Description
An autoclave is a pressurized chamber that combines three parameters to sterilise and disinfect factors time, pressure, and steam. The sterilization agent in autoclaves is steam the basic principle of an autoclave is that all of the materials inside come into direct contact with the steam for a specific period of time. The amount of time and temperature required depends on the type of material to be sterilised, and increasing the cycle's temperature allows for shorter periods. Autoclaves are mostly used for the sterilization medical or laboratory equipment, and they may sterilize a large number of materials at once.
They are commonly used in the laboratory to preparation of culture media during laboratory applications. An autoclave is a machine that kills harmful bacteria, viruses, fungus, and spores on items that are placed inside a pressure vessel using steam under pressure [1]. The items are heated to a sterilizing temperature and held there for a set amount of time. Using saturated steam at a pressure of at least 15 psi, the autoclave must reach and maintain a temperature of 121°C for at least 30 minutes. The most common type of testing is using commercially available test indication kits with spore strips. The spore strips are inserted in the middle of a normal load before being sterilized and the non-autoclaved strips are used to incubate the spore strips.
Sterilization indicators, such as spore strips and indicator tape, provide for routine steam sterilization process monitoring, qualification, and load monitoring. They show if the parameters in a steam autoclave cycle were sufficient for achieving a specified level of microbial inactivation. Gravity, pre-vacuum, liquids, and flash sterilization are the four standard sterilization cycles (also known as immediate use) Light should be kept out of all prepared culture medium and their components, and direct sunlight should be avoided at all times [2]. Normal laboratory humidity has no effect on humidity-sealed glass and plastic containers. High humidity will harm dehydrated powder packages that have been opened. Containers of culture media should not be stored in hot, humid media preparation rooms, especially those that are regularly opened and closed [3]. Storage should be in an adjacent cold room or a large enough storage cupboard is preferable storage areas. Culture medium and its components are subjected to a wide range of temperature and time storage conditions. The following product classifications will aid in separating the various requirements. Media, Culture, Sealed, unopened containers should be kept at room temperature, between 40-45 degrees Celsius. The cap or lid on an open container should be reinstalled gently and securely. It is critical to store opened containers in a dry, room-temperature environment 1 to 5 years on the shelf Media for Broth Preparation, Temperatures should be kept between 2 and 8 degrees Celsius. Allowing the items to freeze is not a good idea [4]. 6 months to 2 years on the shelf Prepared Infection, dehydration, and chemical degradation are particularly vulnerable to Culture Media plates and poured plates of agar media. To prevent plates against microbial infection, aseptic preparation and storage are required. Water losses during storage can be reduced by using impermeable wrapping and/or storing at a temperature of 2°C-8°C. Protection from light, heat, and dryness can delay chemical breakdown, such as oxidation or antimicrobial loss [5]. However, quality control tests should be used to monitor the storage period accurately determined. The rate of moisture loss will be determined by simple weighing tests on freshly made and stored plates.
REFERENCES
- Yingming Xu. Effect of sterilization on cadmium immobilization and bacterial community in alkaline soil remediated by mercapto-palygorskite. Environ. Pollut. 2021; 345-350.
[Crossref] [Google Scholar] [PubMed]
- P. Galvez-Martin. Development, characterization and sterilisation of Nanocellulose-alginate-(hyaluronic acid)- bioinks and 3D bioprinted scaffolds for tissue engineering. Mater. Sci. Eng. C. 2021; 45-54.
[Crossref] [Google Scholar] [PubMed]
- Renhe Yang. Application zinc silicate-potassium silicate coating for anticorrosion of steel bar in autoclaved aerated concrete. Constr Build Mater. 2020; 56-61.
- Marvin Scherzinger. Autoclave pre-treatment of foliage - Effects of temperature, residence time and water content on solid biofuel properties. Renew. Energy. 2021; 43-53.
- Zoran Bergant. Investigation of the durability and performance of autoclave-cured, woven carbon fiber-reinforced polymer composite gears in mesh with a steel pinion. Compos. Struct. 2021; 23-34.
Citation: Szu G (2022) Sterilizing Process and Applications of Autoclave. Pharm Anal Acta. 13:677.
Copyright: © 2022 Szu G. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.