Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2023) Volume 9, Issue 3
Spontaneous Coronary Artery Dissection in a Female with Hypertension: A Case Report and Discussion
Bhagwagar S1, Menon T1, Ameera C Mistry2* and Richard Pham32Independent Researcher, International American University College of Medicine, Vieux Fort, Saint Lucia, USA
3Department Interventional Cardiology, Abrazo Health Network, AZ, USA
Received: 21-Apr-2023, Manuscript No. JTCOA-23-21097; Editor assigned: 24-Apr-2023, Pre QC No. JTCOA-23-21097 (PQ); Reviewed: 02-May-2023, QC No. JTCOA-23-21097; Revised: 09-May-2023, Manuscript No. JTCOA-23-21097 (R); Published: 17-May-2023, DOI: 10.35248/2572-9462.23.9.221
Abstract
Spontaneous Coronary Artery Dissection (SCAD) has become a significant contributor to acute coronary syndrome, myocardial infarction, and sudden death especially in young women and individuals with minimal traditional atherosclerotic risk factors. This case of a 53-year-old female patient, with a past medical history of hypertension and multiple sclerosis, was readmitted to the hospital with a chief complaint of chest pain. She was ultimately diagnosed with SCAD of the left circumflex artery that originated in the distal left main artery, and terminated in the posterior descending artery and obtuse marginal branch artery. The most likely etiology of her SCAD was due to uncontrolled hypertension. She was managed non-operatively with medical management of her blood pressure and given a heparin drip. She was instructed to follow up closely with cardiology in the outpatient setting.
Keywords
Spontaneous coronary artery dissection; Non-atherosclerotic coronary artery disease; Acute coronary syndrome; Coronary angiography; Coronary aneurysm; Myocardial infarction
Introduction
One increasingly recognized cause of non-atherosclerotic acute coronary syndromes that result in myocardial infarction is Spontaneous Coronary Artery Dissection (SCAD). It is defined by the presence of blood entering and dividing the layers of the coronary artery wall to create a false lumen. This causes external compression of the real coronary lumen, which reduces coronary blood flow and results in coronary insufficiency [1]. In 0.1% to 0.4%of instances of Acute Coronary Syndrome (ACS) in the general population, spontaneous coronary artery dissection is to blame. It has been shown to account for roughly a quarter of ACS instances in women under the age of 50. There are also more and more reports of spontaneous coronary artery dissection in postmenopausal and older women. Less than 10% to 15% of instances affect men [2]. The risk factors for SCAD include female gender, intense mental stress, physical effort, pregnancy, fibromuscular dysplasia, and it is linked to genetic connective tissue diseases.
Coronary Angiography is commonly used for diagnosis. SCAD-related angiographic abnormalities include the appearance of a false lumen brought on by intimal disruption, also known as an intimal tear, and the development of an intramural hematoma as a result of bleeding from the vasa vasorum. The false lumen is linked to intramural hematoma, according to advanced intracoronary imaging, and both the real and false lumens may acutely have partial or total thrombosis [3]. With single-vessel dissection, without progression or hemodynamic compromise, without involvement of the left major coronary artery or any other significant portion of the myocardium at danger, the disease can be handled medically with standard therapy for coronary artery disease including aspirin, plavix, ACE inhibitors, beta-blockers and heparin. Stenting and angioplasty can be used to provide great therapeutic results if medical therapy is ineffective, particularly in single-vessel disease with short segment involvement. Other treatment methods include coronary artery bypass grafting and percutaneous transluminal coronary angioplasty [4].
Case Presentation
A 53 year-old female, with a past medical history of hypertension and multiple sclerosis, was recently discharged from the hospital on 11/30/2022 after presenting with a Non-ST Elevation Myocardial Infarction (NSTEMI) status post left heart cardiac catheterization that showed a SCAD of the left circumflex artery. She was being managed non-operatively and the patient remained stable until she was discharged home; however, she came back to the ER on 12/02/2022 complaining of chest pain again.
Cardiology discussed with the patient and her family extensively on her condition and initially started her on a nitro drip for aggressive blood pressure control, and then cleared the patient for discharge. Discharge was revoked when her second troponin levels increased, and the recommendation to have her admitted overnight for observation was given. She underwent cardiac catheterization again and was found to have extensive SCAD originating in the distal left main, extending into the left circumflex, and terminating in the posterior descending artery, as well as the obtuse marginal branch. The left circumflex artery remained patient at this time. Dissection appeared slightly worse from previous CTA from 11/26/2022. Etiology was most likely due to uncontrolled hypertension. The patient was then admitted to the ICU for 48 hours with a heparin drip and tight blood pressure control. At that the time of writing, the patient was cleared for discharged by cardiology and was advised to have close follow up via outpatient care (Figures 1-3).
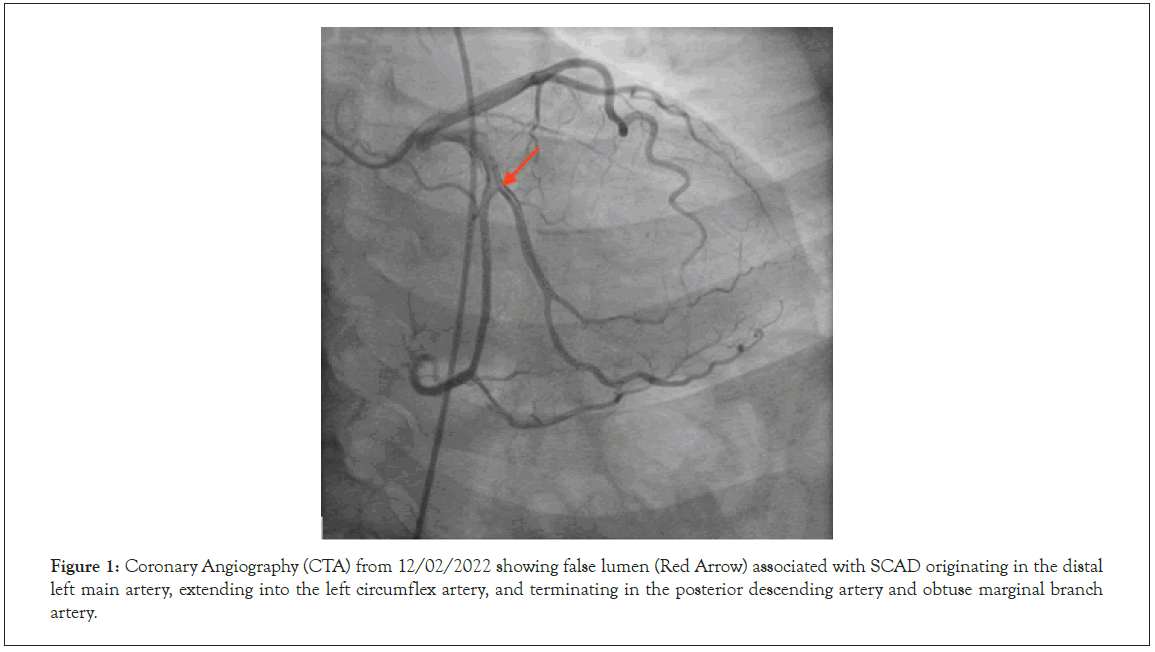
Figure 1: Coronary Angiography (CTA) from 12/02/2022 showing false lumen (Red Arrow) associated with SCAD originating in the distal left main artery, extending into the left circumflex artery, and terminating in the posterior descending artery and obtuse marginal branch artery.
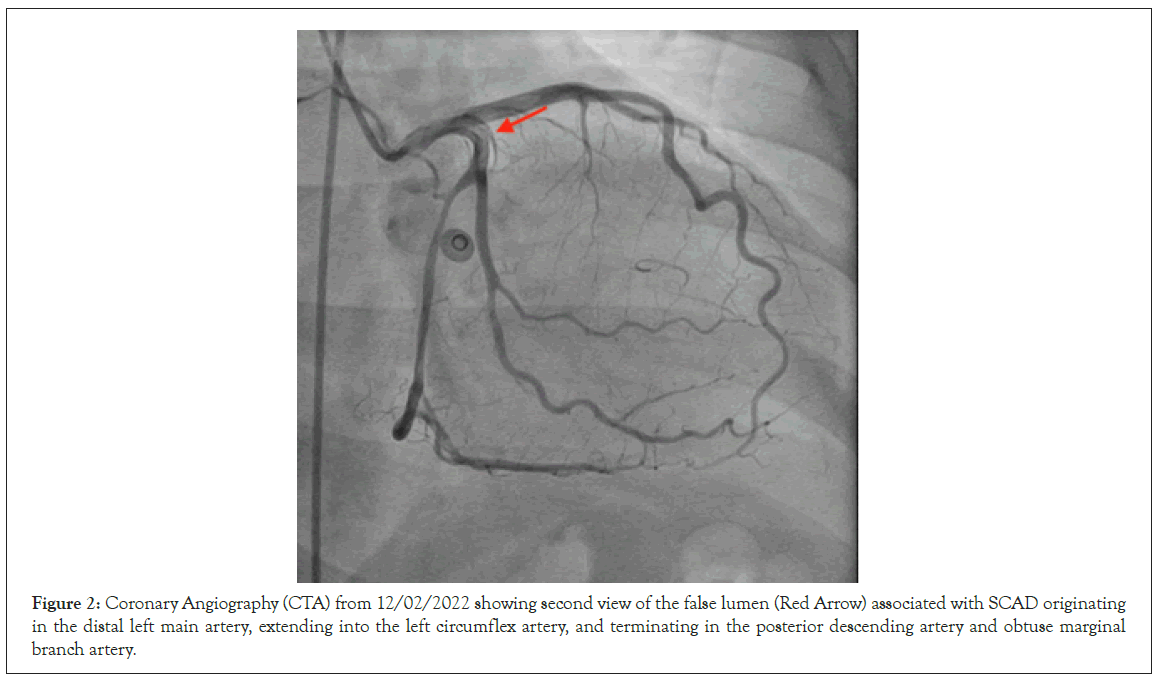
Figure 2: Coronary Angiography (CTA) from 12/02/2022 showing second view of the false lumen (Red Arrow) associated with SCAD originating in the distal left main artery, extending into the left circumflex artery, and terminating in the posterior descending artery and obtuse marginal branch artery.
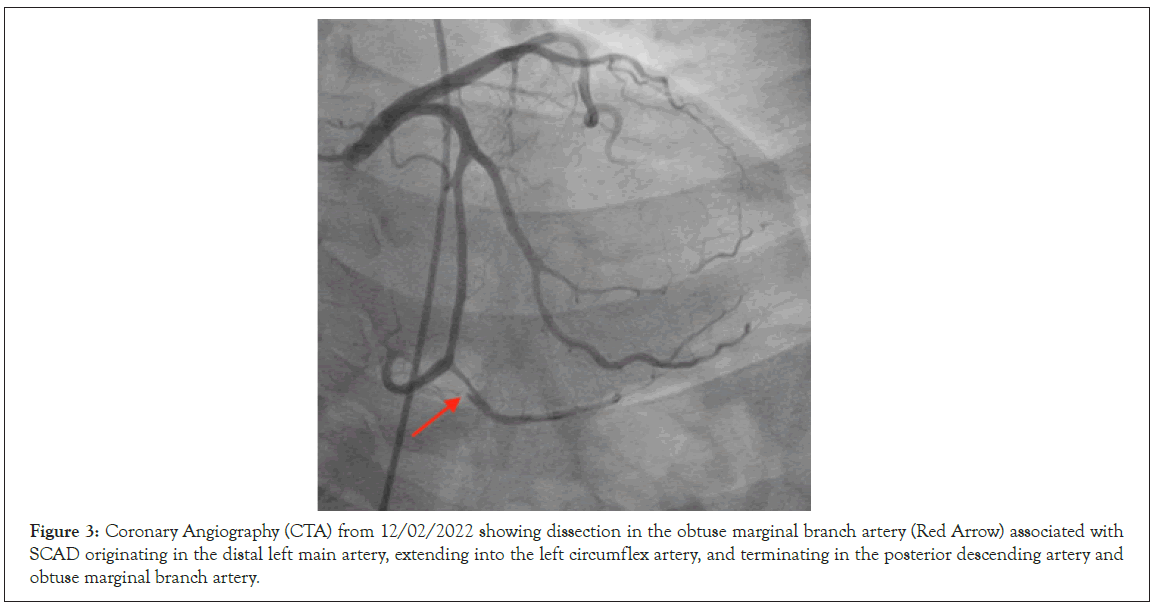
Figure 3: Coronary Angiography (CTA) from 12/02/2022 showing dissection in the obtuse marginal branch artery (Red Arrow) associated with SCAD originating in the distal left main artery, extending into the left circumflex artery, and terminating in the posterior descending artery and obtuse marginal branch artery.
Discussion
Acute coronary syndrome patients are thought to be at an increased risk of developing spontaneous coronary artery dissection, which has an estimated incidence of 0.1% to 0.2%. SCAD should be suspected as a diagnosis as soon as possible in patients with ACS of unknown origin because it prevents coronary perfusion distal to the lesion, with Acute Myocardial Infarction (AMI) being a life-threatening disease. The precise etiology and pathophysiology of SCAD is poorly understood [5]. Conditions linked to SCAD include connective tissue abnormalities, vasculitis, coronary arthritis, underlying atherosclerosis, cocaine use and following physical exercise, or traumatic chest injuries. SCAD cases are typically divided into three categories those who present with:
• Significant preexisting atherosclerosis
• During the peripartum period, with the majority of cases occurring within two weeks of delivers, or in association with oral contraceptive use
• Idiopathic presentation [6].
Saw angiographic classification includes Type I—which has a link between real and false lumens with contrast staining, Type II—has diffuse stenosis and is at least 20 mm, with Variant 2A having diffuse arterial narrowing bordering normal arterial segments, and Variant 2B showing diffuse narrowing that extends to the distal tip of the artery, and Type III—being less than 20 mm and comprising of focal or tubular stenosis and mimicking atherosclerosis [2].
Here, a case of SCAD of the left circumflex artery, that originated in the distal left main artery and terminated in the posterior descending artery and obtuse marginal branch artery, caused an increase in troponin levels. The posterolateral branch, which in some individuals will develop from the left circumflex and the obtuse marginal branch, supplies a portion of the cardiac inferior wall and left marginal artery. The left marginal artery is a broad branch that extends over the heart’s rounded obtuse margin. It is generally understood that SCAD has a proclivity for coronary disease, and usually occurs in the Left Anterior Descending Artery (LAD). In 46% to 61% of cases, the diagonal and septal branches are damaged, whereas 15% to 45% of cases include the circumflex, ramus, and marginal branches. Depending on the literature, SCAD that affects several coronary branches is uncommon, but may occur in 9% to 23% of patients [7].
Clinical trials to determine the best therapy and treatment guidelines for SCAD are currently lacking. Emphasis is placed on encouraging flow distal to the lesion and limiting aggravation of the dissection. A definite risk factor for the reoccurrence of SCAD is hypertension [8]. Poorly managed blood pressure, atherosclerosis, and other vascular diseases are additional risk factors for SCAD, as well as other arterial dissections. Women tend to experience left coronary artery dissection more often than men overall; and with 75% of cases involving the LAD, 20% involving the Right Coronary Artery (RCA), 4% involving the left circumflex artery, and less than 1% due to the reoccurrence of HTN [8].
Preferred treatments are determined on the comorbidities at play. ACH inhibitors or ARBS’s should be taken if the patient has diastolic heart failure. Potential agents are beta-blockers, which may lead to reduced contractility. There are no obvious benefits to the use of lipid lowering medications like statins or fibrates; and both dual anti-platelet and anticoagulation medications have limited benefit for SCAD as they may induce bleeding [9]. Treatment options include medical therapy and revascularization with either Coronary Artery Bypass Graft (CABG) or Percutaneous Coronary Intervention (PCI) [1]. Follow up angiograms have shown the use of aspirin, other anti-platelets, nitrates, and beta-blockers, have helped dissections heal. The majority of left main dissections, and those involving the RCA or triple vessel, are treated with CABG. Bridging to orthotopic heart transplantation using a Left Ventricular Assist Device (LVAD) may be the only choice in severe heart failure cases [1]. SCAD has a significant risk of reoccurrence. Depending on the context and underlying comorbidities, reoccurrence from HTN occurs in 10% to 30% of patients. Saw et al, prospectively tracked 327 patients with SCAD and found 10.4% of them had reoccurring SCAD [10].
Conclusion
In conclusion, Spontaneous Coronary Artery Dissection (SCAD) is a significant contributor to acute coronary syndrome, myocardial infarction, and sudden death, particularly in young women with minimal traditional atherosclerotic risk factors. The exact etiology and pathophysiology of SCAD are still not fully understood, but it is believed to be associated with connective tissue abnormalities, coronary arteriopathies, and underlying atherosclerosis. Various risk factors such as female sex, intense mental stress, physical effort, pregnancy, fibromuscular dysplasia, and genetic connective tissue diseases can predispose individuals to SCAD. Patients diagnosed with SCAD are at a significant risk of recurrence, particularly those with hypertension. Long-term follow-up and management are crucial to prevent further vascular events. While the available data on optimal medical therapy for SCAD is limited, current approaches focus on individualized care and risk factor modification. Further research is needed to enhance our understanding of the pathophysiology, risk factors, and optimal management strategies for SCAD. By raising awareness and improving clinical recognition, healthcare professionals can provide timely and appropriate care to individuals experiencing SCAD, ultimately reducing morbidity and mortality associated with this condition.
Conflict of Interest
All authors agree for the publication. For all authors, there is no competing interests to.
References
- Almeda FQ, Barkatullah S, Kavinsky CJ. Spontaneous coronary artery dissection. Clin Cardiol. 2004;27(7):377-380.
- Hayes SN, Kim ES, Saw J, Adlam D, Arslanian-Engoren C, Economy KE, Ganesh SK, et al. Spontaneous coronary artery dissection: Current state of the science: A scientific statement from the American Heart Association. Circulation. 2018;137(19):e523-557.
- Akyuz A, Alpsoy S, Akkoyun DC. Spontaneous coronary artery dissection and woven coronary artery: three cases and a review of the literature. Korean Circ. J. 2013;43(6):411-415.
- Mortensen KH, Thuesen L, Kristensen IB, Christiansen EH. Spontaneous coronary artery dissection: a Western Denmark Heart Registry study. Catheter Cardiovasc Interv. 2009;74(5):710-717.
- Valencia-Manrique JC, Garcia M, Adetiloye A, Alaameri R, Singh R, Chaudhari S. A case report of spontaneous coronary artery dissection. An intern med Clin cases. 2022;1(4):e220040.
- Mararenko A, Minassian G, Kataria A, Ajam F, Schoenfeld MS. Double trouble-spontaneous coronary artery dissection of the left anterior descending and posterior descending arteries in a right dominant circuit: A case report. J Med Cases. 2021;12(12):491.
- Li Y, Yang M, Chen X, Zhang X, Zhang R, Zuo P, et al. Spontaneous left main coronary artery dissection occurred in a young male: a case report and review of literature. BMC Cardiovasc Disord. 2022;22(1):256.
- Alquran L, Patel A, Safi L, Patel A. A rare case of multivessel SCAD successfully treated with conservative medical management. Case Reports in Cardiology. 2020;2020:1-4.
- Thaler C, Witt DR, Henry TD, Grey EZ, Baechler CJ, Lohese O, et al. Revascularization and long-term outcomes in high- acuity spontaneous coronary artery dissection. Catheter and Cariovasc Interv. 2022;100(7):1229-1241.
- Sokolska JM, Meirer LM, Holy EW, Templin C, Alkadhi H, Manka R. A young woman with recurrent spontaneous coronary artery dissection. Kardiol Pol. 2020;78:1059-1061.
Citation: Bhagwagar S, Menon T, Mistry AC, Pham R (2023) Spontaneous Coronary Artery Dissection in a Female with Hypertension: A Case Report and Discussion. J Thrombo Cir. 9:221.
Copyright: © 2023 Bhagwagar S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
