Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- The Global Impact Factor (GIF)
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
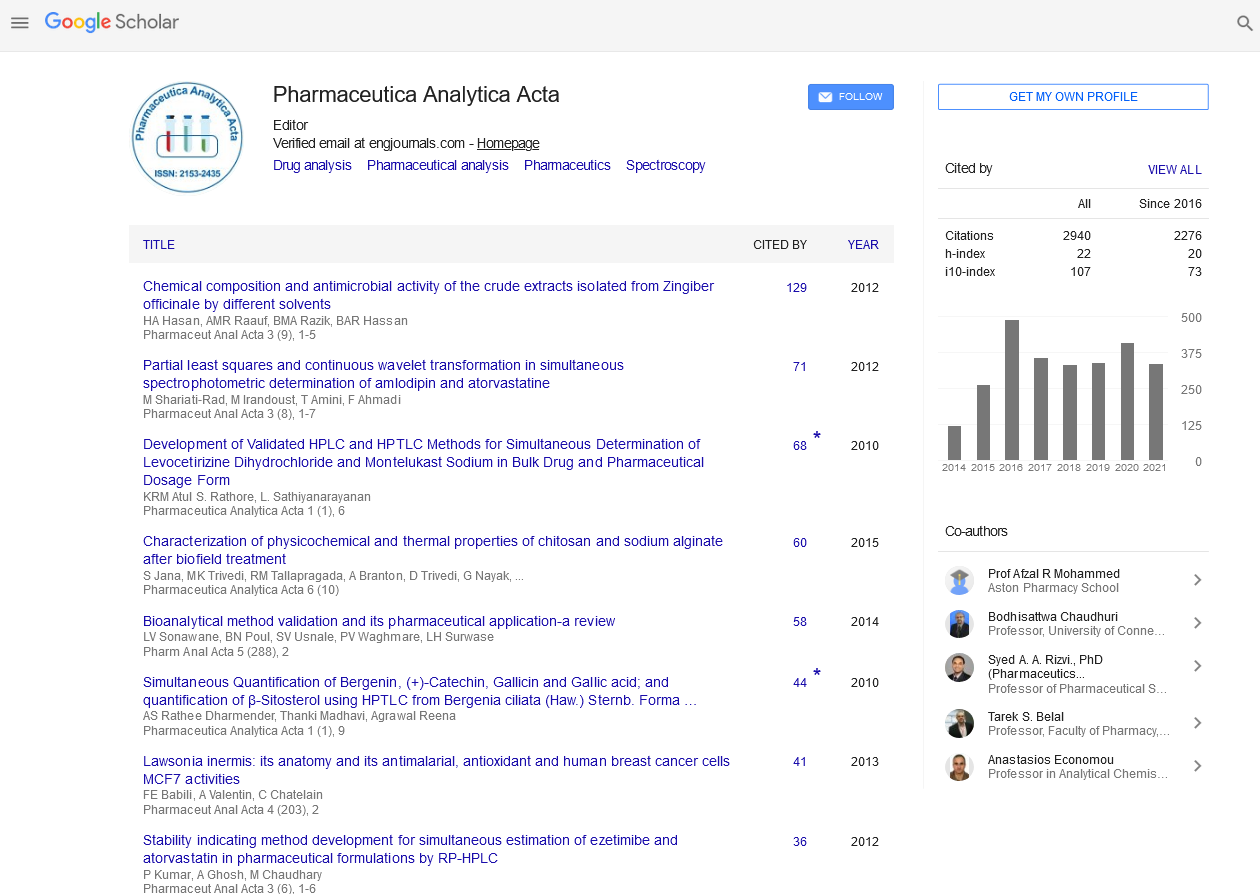
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion Article - (2023) Volume 14, Issue 1
Product Certification for the Pharmaceutical Goods
Svan Lube*Received: 02-Feb-2023, Manuscript No. PAA-23-19631; Editor assigned: 06-Feb-2023, Pre QC No. PAA-23-19631(PQ); Reviewed: 20-Feb-2023, QC No. PAA-23-19631; Revised: 27-Feb-2023, Manuscript No. PAA-23-19631(R); Published: 06-Mar-2023, DOI: 10.35248/2153-2435.23.14.711
Description
World Health Organisation (WHO) has created Good Manufacturing Practices (GMP) for pharmaceutical goods that are similar to those imposed by national pharmaceutical control bodies in industrialised nations. They include criteria for employees, buildings, equipment, materials, production procedures, labelling, packaging, quality assurance, and, in most cases, stability testing. Adherence to GMPs is enforced in countries with effective pharmaceutical control agencies by a system of investigations and regulatory controls, which are often, tailored to individual medicine dosage forms. A manufacturer may have acceptable requirements for solid dosage forms but not for sterile injectable preparations. Frequently, a supplier must accept or at least expedite requests for performance reports from national pharmaceutical control agencies, and failing to get such data for the buyer casts doubt on prior performance.
If funds are available, buyers with pharmaceutical employees skilled in GMP inspection may do their own examinations of local manufacturers who are possible suppliers. Countries that join the system agree to confirm that pharmaceuticals are registered in the exporting country and that producers' facilities have been inspected and meet GMPs. However, according to a WHO report published in 1995, very few importing countries need pharmaceutical product certifications for registration or procurement purposes. This certification process provides considerable assurance because it is based on an inspection of the manufacturing facilities for GMPs by the exporting country's competent authorities. It is a low-cost method for the procuring office to help ensure the quality of purchased products.
The procurement office should be able to obtain the following information through the certification scheme:
• Whether a product is lawfully marketed in the exporting country, and if not, why not.
• Whether the supplier produces the dosage forms, packages or labels a finished dosage form produced by a third party, or is not involved in any of these operations.
• Whether the product's maker has been inspected and the frequency of inspections
• Whether the certificate is provisional, requiring technical review
• Whether the information given by the supplier satisfies the certifying authority on all aspects of the product's production performed by a third party. The validity and accessibility of pharmaceutical product certificates granted under the WHO framework.
• The exporting nation's authority's dependability and reactivity.
• The exporting nation's authority's ability to conduct necessary GMP inspections.
• Capability of the importing country’s authority to assess the authenticity or validity of the certificate of a pharmaceutical product provided, especially when it is submitted through the manufacturer or importing agent.
As a result, product certification under the WHO scheme is only as reliable as the agency doing it, and according to WHO, only around 20% of member nations have a national drug regulatory system capable of ensuring the quality of medicines circulating in their national markets. As a result, certifications should be received with caution unless the national Drug Regulatory Affairs (DRA) ability to carry out the scheme is known. Furthermore, while national pharmaceutical-control authorities in the major pharmaceutical-exporting countries are generally thorough in their assessments, getting reports may take some time. Some countries' agencies have been determined to be less trustworthy.
WHO admits that the pharmaceutical manufacturing sector has changed dramatically since the plan was created decades ago on the basis that a drug discovery output would be sold directly one by one from relevant country to the country of ultimate destination. Pharmaceutical manufacturing and trade had already expanded significantly over the world, with numerous phases of production taking place in various countries before the product reaches its final destination. As a result of this evolution and other difficulties found, WHO has required service levels the approach.
Citation: Lube S (2023) Product Certification for the Pharmaceutical Goods. Pharm Anal Acta. 14:711
Copyright: © 2023 Lube S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.