Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- The Global Impact Factor (GIF)
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
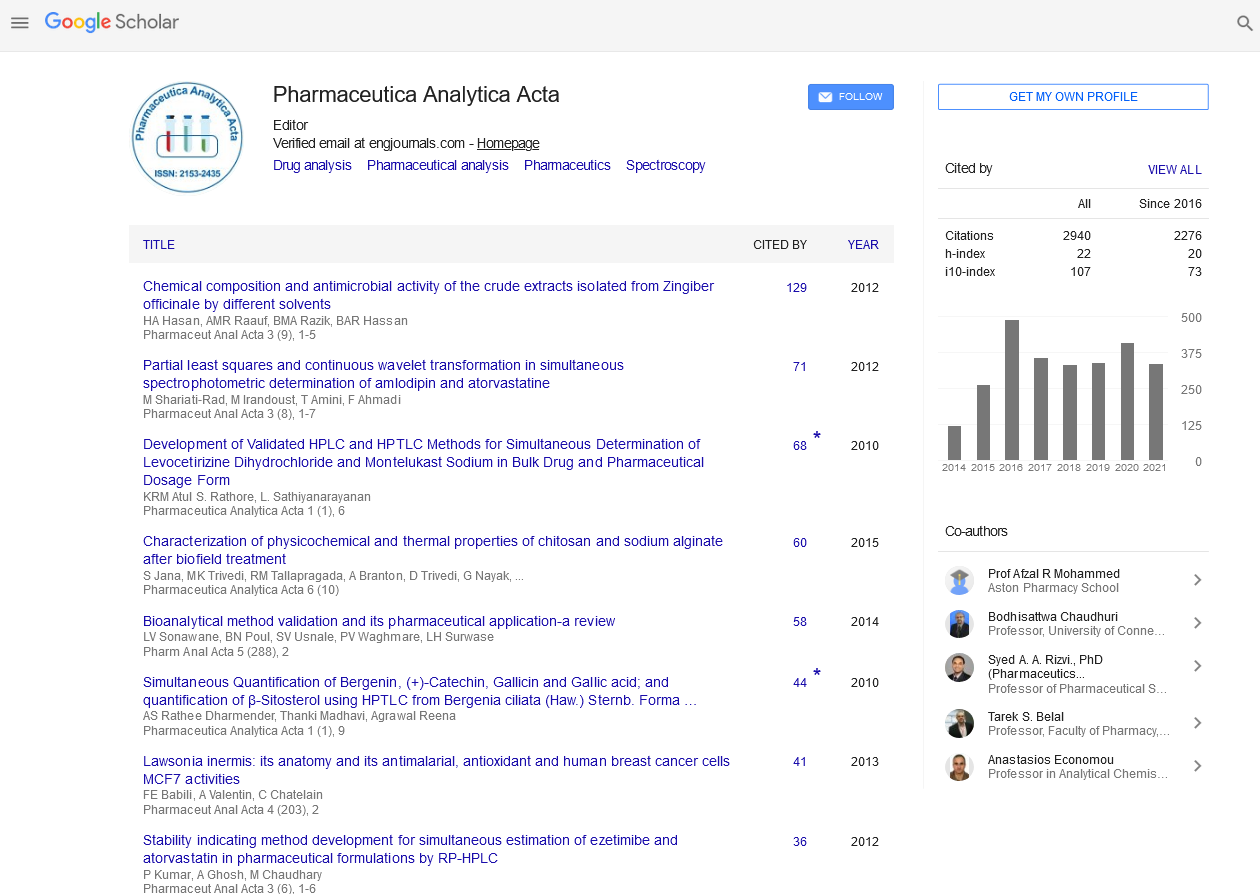
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2022) Volume 13, Issue 9
Pharmacokinetics and Pharmacodynamic Properties of Antimalarial Drugs
Heise Hartung*Received: 01-Sep-2022, Manuscript No. PAA-22-18322 ; Editor assigned: 05-Sep-2022, Pre QC No. PAA-22-18322 (PQ); Reviewed: 19-Sep-2022, QC No. PAA-22-18322; Revised: 26-Sep-2022, Manuscript No. PAA-22-18322 (R); Published: 03-Oct-2022, DOI: 10.35248/2153-2435.22.13.693
Description
Pharmacodynamics is the study of the interaction between a medication and its receptors, its mode of action, and its therapeutic effect. Pharmacokinetics is the study of a drug's absorption, distribution, metabolism, and excretion and they all plays a key role in drug-drug interactions. Many drugs target the same receptors use similar metabolic pathways. As a result, there are discrepancies in pharmacokinetics and pharmacodynamics mostly during medication absorption, distribution (plasma drug binding protein), biotransformation.
Most drugs are administered orally, consequently the intestinal mucosa accounts for the majority of absorption (duodenum). Medication bioavailability is reliant on enterocyte cytochrome P450 (CYP450) enzymes, which metabolize the drug before it reaches the systemic circulation, and enterocyte P-glycoprotein, which can actively pump medicines back into the intestinal lumen. Thus, P-glycoprotein and enterocyte CYP450 induction or inhibition can affect a drug's bioavailability. Drugs typically bind to plasma transport proteins after absorption. Distribution is fundamentally influenced by the amount of binding protein, and different medications can have an impact on protein binding. The medication is transformed into active and inactive metabolites as it travels through the liver. This process, known as biotransformation, has a significant impact on the effectiveness of treatments.
The biotransformation of drugs depends on a number of stages. Phase I consists of three reactions hydrolysis, oxidation, and reduction that are mostly mediated by CYP450. Phase II involves conjugation, which is carried out by the use of enzymes including glutathione S-transferase, N-acetyl transferase, and uredines diphosphoglucuronosyl transferase. These enzymes are crucial for xenobiotic detoxification and/or excretion rates. P-glycoprotein, Multidrug Resistance Protein (MRP), and Organic Anion Transport Protein 2 (OATP2) are examples of drug plasma membrane transporters (influx and efflux) that are localized in the liver, kidney, gastrointestinal system, endothelium, and epithelial membrane, among other organs. They play an important role in drug pharmacokinetics and pharmacodynamics.
The metabolism and distribution of some medications have been demonstrated to be impacted by acute malaria itself, though not, it would appear, through affecting drug absorption, but rather by enhancing binding to 1-glycoprotein in plasma. In acute malaria, inhibition of hepatic metabolism, particularly CYP3A4 enzymes, results in a decreased clearance of quinine.
Quinine is one of the most commonly used drugs for malaria treatment worldwide. It is the first-line treatment. Falciparum complicated malaria and is a treatment option falciparum uncomplicated malaria in chloroquine resistant regions. The metabolism of quinine is interesting because severe malaria affects quinine absorption, the binding protein fraction, CYP450 activity, and excretion.
Both rifampicin and rifabutin, two medications used to treat tuberculosis, have different pharmacokinetic properties. Rifampicin and rifabutin pharmacokinetics both rifampicin and rifabutin are drugs used for the treatment of TB. Since it has less pharmacological interactions with antiretroviral medicines (i.e. protease inhibitors) than rifampicin, rifabutin, which is produced from rifamycin S, is mostly utilized in patients who are also HIV infected. In some instances, it has been demonstrated that it is still effective in the presence of rifamycin resistance. It is also used to treat atypical mycobacterial infections. Both drugs act by inhibiting the β-subunit-dependent DNA–RNA polymerase that leads to suppression of DNA formation by Mycobacterium tuberculosis. They are bactericidal and bacteriostatic and act intra and extra cellular. Absorption both drugs are generally well absorbed by the oral route. However, patients with gastrointestinal disorders, diabetes, and AIDS have shown altered absorption. Rifampicin absorption also exhibits substantial inter individual variability, with both slow and fast patterns of absorption, according to pharmacokinetic studies.
Citation: Hartung H (2022) Pharmacokinetics and Pharmacodynamic Properties of Antimalarial Drugs. Pharm. Anal. Acta. 13:693.
Copyright: © 2022 Hartung H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.