Indexed In
- Open J Gate
- Genamics JournalSeek
- CiteFactor
- Cosmos IF
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Proquest Summons
- Scholarsteer
- ROAD
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research - (2023) Volume 15, Issue 12
Outcome of Guilian Barreâ-Syndrome Using Clinical and Electrophysiological Parameters in Three Neurology CentersâSudan
Mahmoud H.S. Daoud1, Mohmed Hussien Ahmed Mohmed1*, Mohamed Khalaf Allah Saeed2, Ammar El Tahir Mohamed Ahmed3, Etedal Ahmed Abu Elbasher Ibrahim4, Omer Eladil Abdalla Hamid Mohammed5, Khalid Mohammed Ali6, Muaz Abdellatif Mohammed Elsayed7, Abubakr Elmotesim Abdulla Elamin8, Husam Abo Obaida9 and Abdalrahman Abdalmagid102Department of Science, University of Science and Technology, Omdurman, Sudan
3Department of Medicine, University of Khartoum, Khartoum, Sudan
4Department of Medicine, University of Science and Technology, Omdurman, Sudan
5Department of Medicine, International University of Africa, Khartoum, Sudan
6Department of Medicine, University of Gadarif, Gadarif, Sudan
7Department of Bio-Medicine, Omdurman Islamic University, Omdurman, Sudan
8Department of Medicine, University of Gezira, Gezira, Sudan
9Department of Neurology, Sudan Medical Specialization Board, Khartoum, Sudan
10Department of Medicine, Alsalam University, Aldamer, Sudan
Received: 12-Dec-2023, Manuscript No. BLM-23-24319; Editor assigned: 14-Dec-2023, Pre QC No. BLM-23-24319 (PQ); Reviewed: 28-Dec-2023, QC No. BLM-23-24319; Revised: 05-Jan-2024, Manuscript No. BLM-23-24319 (R); Published: 12-Jan-2024, DOI: 10.35248/0974-8369.23.15.632
Abstract
Background: Guillian Barre’-Syndrome (GBS) is an acute, immune mediated disorder, commonly characterized by a rapidly progressive, ascending weakness of the extremity, trunk, respiratory and facial musculature, with inconstant sensory and autonomic dysfunction. This research conducted in Sudanese patients to study the relation between the outcome in GBS and a four parameters; age of the patient, onset duration, presence of autonomic dysfunction and the electrophysiological subtypes.
Methods: A cross-sectional study involving the main three neurology centers in Sudan conducted from March to September 2020, 62 patients enrolled in the study, structured questionnaire consisted of personal data, clinical history, examination findings, management and outcome. The Hughes Functional Grading Scale (HFGS), which provides an objective measure of disability, was used to rate clinical performance at disease nadir and at 90 day from the illness.
Results: The study revealed that males and females are equally represented; the majority of patients (70%) are between 18 and 50 years. The onset of weakness was less than or equal 3 days in (33.9%) of patients, from 4 to 7 days in (41.9%), from 8 to 14 days in (11.3%) and above 14 days in (12.9%). 25 patients (40.3%) had Evidence of autonomic dysfunction. Based on the electrophysiology, (37.09%) of patients were classified as Acute Motor Axonal Neuropathy (AMAN), (29.03%) as Acute Inflammatory Demyelinating Poly neuropathy (AIDP) and (29.03%) as Acute Motor-Sensory Axonal Neuropathy (AMSAN).
Regarding the outcome, 30 patients (48.4%) fully recovered, 25 patients (40.3%) recovered with motor deficit, and 7 patients (11.3%) unfortunately died. The results showed that there was no statistically significance between different age groups, duration of onset or presence of autonomic dysfunction and the outcome after three months, P value (.21, .21, .1) respectively. The results showed that the Prognosis after three months and the mortality rate of AMAN and AMSAN subtypes were poorer than that of AIDP.
Conclusion: Axonal type of GBS found to be in nearly 2/3 patients. 40% showed clinical evidence of dysautonomia, and showed no statistical evidence with outcome, age of the patients, and onset of the disease also did not show statistically significant effect on outcome at day-90. The outcome of axonal types at day-90 was poorer than that of demyelinating form.
Keywords
Guilian Barre’-Syndrome; Acute motor axonal neuropathy; Acute inflammatory demyelinating polyneuropathy; Outcomes
Abbreviations
GBS: Guilian Barre’-Syndrome; NCS: Nerve Conduction Study; AMAN: Acute Motor Axonal neuropathy; AMSAN: Acute Motor and Sensory Axonal Neuropathy; AIDP: Acute Inflammatory Demyelinating Polyneuropathy; IVIG: Intravenous Immunoglobulin
Introduction
Guilian Barre’-Syndrome (GBS) is an acute, immune mediated disorder of spinal roots, peripheral nerves and cranial nerves, commonly characterized by a rapidly progressive, ascending weakness of the extremity, trunk, respiratory and facial musculature, with inconstant sensory and autonomic dysfunction [1] with nadir of symmetrical weakness often reached within 4 weeks and represent the key clinical feature [2]. And majority of cases present with antecedent infection [3].
The annual incidence of Guillain-Barré syndrome is around 1-3/100000 population [4]. It can occur in any age group. The age specific curve seems to show a bimodal distribution, with peaks in young adults and the elderly [5]. Males appear to be affected more commonly [6].
GBS is a clinical diagnosis. The role of nerve conduction study NCS is to confirm the diagnosis and to discriminate between axonal and demyelinating subtypes [7], in addition the presence of albuminocytological dissociation in cerebrospinal fluid CSF analysis will support the diagnosis [5]. Commonly recognized subtypes are acute inflammatory demyelinating polyneuropathy AIDP, acute motor axonal neuropathy AMAN and acute motor and sensory axonal neuropathy AMSAN which are two variants characterized by immune attack directed against the axons rather than Schwann cells and myelin [8,9].
Intravenous immunoglobulin IVIG and plasma exchange have proved to be effective [10]. However, most of these studies were done in Europe and North America where most patients have the acute inflammatory demyelinating poly neuropathy variant of the disorder.
Dysautonomia is major factor of increasing morbidity, mortality and prolonged hospital stay in addition to cranial nerve and respiratory affection [11]. In 80% of cases with GBS start to recovery at 28 days in with mean 200 days achieving complete recovery and 65% may encounter residual weakness [12]. AMAN in particular associated with rapid progression of weakness and poor outcome [13].
Patients who survive Guillain-Barré syndrome frequently have residual complaints and deficits, which can have a substantial effect on daily activities and quality of life. About 20% of patients with Guillain Barré syndrome cannot walk unaided 6 months after onset. Most patients have residual pain and fatigue, which can in part be attributed to persistent axonal loss [14]. Patient characteristics consistently related to poor prognostic outcome in Guillain-Barré syndrome are high age (aged 40 years and over), preceding diarrhea and high disability at nadir [15].
As GBS has a significant morbidity and mortality if not managed properly, and it needs a special setting in management and a low threshold for diagnosis. Therefore accurate information is necessary regarding the frequency of electrophysiological variants, and prognostic factors, to ascertain public health measures and to ensure appropriate management. Therefore highlighting on this issue may help in improving the outcome and in anticipation of the disease sequelae.
Materials and Methods
A descriptive cross-sectional study involving multi Sudanese centers in Ibrahim Malik Hospital ICU at the National Center for Neurosurgery and Neurosciences (NCSN), Soba University Hospital and Omdurman teaching hospital. These are the major hospitals in Sudan receiving neurology patients from Khartoum and all Sudan states. Also These health facilities provide clinical and electrophysiology services and ICUs. This study conducted from March to September 2020, 62 patients were enrolled in this study, and structured questionnaire consisted of personal data, clinical history, examination findings, management and outcome. The Hughes Functional Grading Scale (HFGS), which provides an objective measure of disability, was used to rate clinical performance at disease nadir and at day 90 of the illness and Nerve Conduction Velocity (NCV) was performed using standard procedure protocols, reported by expert neurologists and elctrophysiologists. Data was analyzed using Statistical Packages for Social Sciences (SPSS) version 23.0. Frequencies and Chi squire test were used when appropriate.
Results
A total of 62 patients with Guilian Barre’-Syndrome, who satisfied the inclusion criteria were studied. There were 32 (51.6%) males and 30 (48.4%) females with male to female ratio of 1.07:0.93 (Figure 1) and Regarding age group, 20 patients (32.3%) were between 18 and 30 years, 23 patients (37.1%) were between 31 and 50 years, 15 patients (24.2.2%) were between 51 and 65 years and 4 patients (6.5%) were above 65 years (Figure 2). The majority of patients presented with lower limb weakness (93.5%), 4.8% presented with upper limb weakness and 1.6% presented with weakness in the bulbar or respiratory muscles from the start. The onset of the weakness was less than or equal 3 days in (33.9%) of patients, from 4 to 7 days in (41.9%), from 8 to 14 days in (11.3%) and above 14 days in (12.9%) (Figure 1).
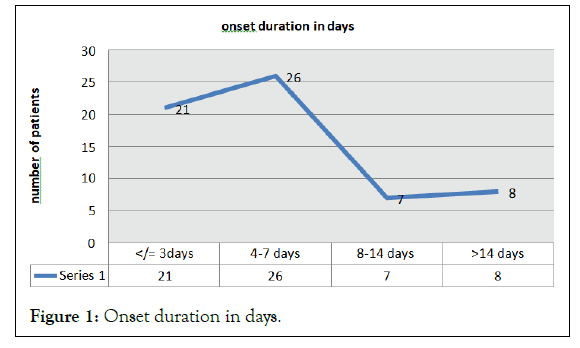
Figure 1: Onset duration in days.
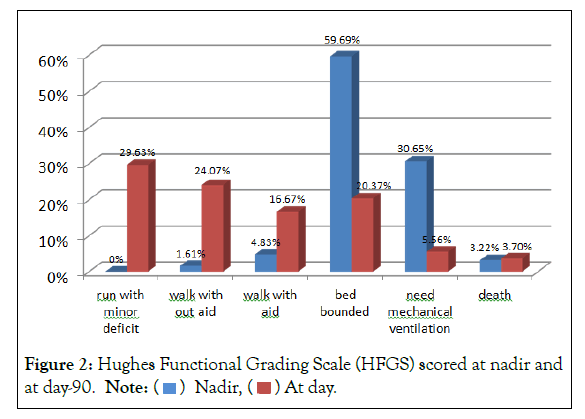
Figure 2: Hughes Functional Grading Scale (HFGS) scored at nadir and
at day-90. Note: ( ) Nadir, (
) Nadir, ( ) At day
) At day
Distal paresthesia preceding the weakness observed in 54 patients (87.1%), 3 patients (4.8%) developed urinary bladder incontinence and 36 patients (58.1%) had back pain at the onset of the disease. Regarding the autonomic dysfunction, 4 patients (6.5%) had minimum heart rate at rest (abnormal<50), 30 patients (48.4%) had maximum heart rate at rest (abnormal>110) and 25 patients (40.3%) had liable blood pressure. Overall, 25 patients (40.3%) developed clinical Evidence of autonomic dysfunction.
Based on the electrophysiology, (39.51%) were classified as Acute Motor Axonal Neuropathy (AMAN), (31.45%) as Acute Inflammatory Demyelinating Poly neuropathy (AIDP) and (29.03%) as Acute Motor- Sensory Axonal Neuropathy (AMSAN). The Hughes Functional Grading Scale (HFGS), which provides an objective measure of disability, was used to rate clinical performance. Motor function deficits were scored on the HFGS scale, ranging from 0 to 6. (Figure 2) showed Hughes Functional Grading Scale scored at nadir and at day 90.
Regarding treatment, (87.1%) received intra venous immune globulin, (3.2%) underwent plasma exchange, and (1.6%) received both of them while (8.1%) didn’t receive any treatment. With 43.5% of patients were admitted to the ICU (Mean=18 days) and 30.6% of patients needed assisted ventilator. And the outcome was, 30 patients (48.4%) fully recovered, 25 patients (40.3%) recovered with motor deficit, and 7 patients (11.3%) died.
The results showed that there was no statistical significance between different age groups and the outcome after three months (P value=0.21) but there was statistically significant between gender and the outcome (p value=0.05) (Table 1) show the results. Also onset of the disease was statistically not significant with the disease outcome after three months (p value=0.21) (Table 2) show the results. The study showed no statistically significant between the outcome and evidence of autonomic dysfunction (p value=0.10).
Outcome after three months |
|||
|---|---|---|---|
| Gender | Fully recovered | Recovered with motor deficit | Died |
| Male | 20 | 9 | 3 |
| FFemale | 10 | 16 | 4 |
| Total | 30 | 25 | 7 |
Table 1: Correlation between gender and the outcome at day-90.
| Onset of the disease | Outcome after three months | |||
|---|---|---|---|---|
| Fully recovered | Recovered with motor deficit | Died | Total | |
| less than or equal 3 days | 6 | 11 | 4 | 21 |
| 4 days-7 days | 16 | 8 | 2 | 26 |
| 8-14 days | 5 | 2 | 0 | 7 |
| >14 days | 3 | 4 | 1 | 8 |
| Total | 30 | 25 | 7 | 62 |
Table 2: Correlation between the onset of the disease and the outcome at day- 90.
The results showed that the Prognosis after three months and the mortality rate of AMAN and AMSAN subtypes were poorer than that of AIDP. Outcome after three months is statistically significant with AIDP and AMSAN subtypes (p value=0.01) (p value=0.05) but not with AMAN subtype (p value=0.17) (Table 3).
| Disease variants | Outcome after three months | ||
|---|---|---|---|
| Fully recovered | Recovered with motor deficit | Died | |
| Aman | 9 | 12 | 4 |
| Amsan | 5 | 10 | 3 |
| Aidp | 13 | 6 | 0 |
Table 3: Outcome after three months among disease variants.
Discussion
GBS occurs throughout the world with a median annual incidence of 1.3 cases per population of 100 000. Our results showed that there were no differences in incidence distribution between male and female, this may be due to the type of study and the number of cases, these results is similar to studies conducted in India [16,17]. Study conducted in USA showed that males are more likely to be affected than female.
GBS has been reported in all age groups from infancy to elderly with bimodal age distribution [18]; however it is more frequently affected adults and older people. In this study, people who are 50 years and less are more commonly affected, finding similar to results from previous studies [16,17].
Limb weakness was the most frequent symptom at the onset of the disease. This is due to inflammation of the nerves (polyneuritis) which lead to muscle weakness. The weakness starts in the feet and then ascends to involve the upper body and limbs [6]. Focal conduction block at the level of the lumbar and cervical nerve roots, rather than along the length of the nerve fiber can easily explained this [7]. No differences in the pattern of classical muscle weakness were noted in this study.
Weakness of respiratory and bulbar muscles can lead to dangerous consequences such as respiratory failure and aspiration pneumonia. Progressive weakness of both inspiratory and the expiratory muscles is the mechanism leading to respiratory failure in patient with GBS. Few patients in this study developed respiratory or bulbar muscle weakness, findings are less to another studies [18,19].
Autonomic disturbance is reported to occur in 40% of patients with GBS in this study. Abnormal heart rate and fluctuated blood pressure are one of the most frequent manifestations. In literature, the prevalence of autonomic dysfunctions in GBS is high and reported to affect 65% of patients with mild GBS and may reach up to 90% in moderate to severe GBS [20]. In this study we depend on monitoring the charts looking for pulse and blood pressure variabilities, we did not do objective tests to assess autonomic function, for this reason there may be underestimation for the exact number of patients who have autonomic dysfunction in our study.
The frequency and severity of GBS variants vary from region to region. This study revealed that AMAN was the commonest subtype accounted for 37.09% followed by AIDP and AMSAN (29.03% for each). Study from north china showed that AMAN was the commonest subtype there. On the other hand, AIDP subtype was found to be dominated in Europe and United States [21,22].
GBS could occur at any age. The results showed that there was no statistically significant difference between different age groups and the outcome after three months (P value=0.21). Epidemiological base study from UK reported that the severity of clinical features and prognosis of GBS are similar in old and young adults [23]. Another study showed that elderly patient with GBS has more severed disease, more damage, and slower recovery and consider an important factor in predicting poor prognosis of GBS [24].
GBS characterized by rapid onset muscle weakness reaching its worst within two or sometimes as long as four weeks. Onset of the disease was statistically not significant with the disease outcome after three months (p value=0.21) in this study. Several studies reported that progression and outcome of the disease was not related to the onset of the disease [25]. Other studies revealed that shorter timed of progression to maximal symptoms can be considered as poor prognostic factor [26,27].
Most patients with GBS begin to recover at 28 days with mean time to complete recovery being 200 days. Our results showed that the Prognosis at day-90 from the onset in AMAN and AMSAN subtypes were poorer than that of AIDP subtype. Studies conducted in China showed that there was no difference in prognosis between AIDP and AMAN subtypes [21,22]. AMAN subtype was associated with poor prognosis in several studies from Europe and America [22,28]. Other studies reported that AMSAN subtype had prolonged and incomplete recovery compared to other forms of GBS [29,30].
Conclusion
Axonal Guillain-Barre Syndrome (GBS) is a subtype of GBS characterized by damage to the axons, which are the long, slender projections of nerve cells responsible for transmitting nerve impulses. Axonal GBS found to be in nearly 2/3 patients. 40% showed clinical evidence of dysautonomia, and showed no statistical evidence with outcome, age of the patients, and onset of the disease also did not show statistically significant effect on outcome at day-90. The outcome of axonal types at day-90 was poorer than that of demyelinating form.
Ethical Consideration
Ethical clearance was obtained from committee of SMSB (Sudan Medical Specialization Board). Acceptance of hospitals administrations on approval was obtained. Written informed consent from patients was obtained before participation.
References
- Hughes RA, Cornblath DR. Guillain-barre syndrome. Lancet. 2005;5;366(9497):1653-1666.
[Crossref] [Google Scholar] [PubMed]
- Fokke C, van den Berg B, Drenthen J, Walgaard C, van Doorn PA, Jacobs BC. Diagnosis of Guillain-Barré syndrome and validation of Brighton criteria. Brain. 2014;137(1):33-43.
[Crossref] [Google Scholar] [PubMed]
- Koga M, Yuki N, Hirata K. Antecedent symptoms in Guillain-Barré syndrome: An important indicator for clinical and serological subgroups. Acta Psychiatr Scand. 2001;103(5):278-287.
[Google Scholar] [PubMed]
- Sejvar JJ, Baughman AL, Wise M, Morgan OW. Population incidence of Guillain-Barre syndrome: A systematic review and meta-analysis. Neuro Epidemiol. 2011;36(2):123-133.
[Google Scholar] [PubMed]
- Yuki N, Hartung HP. Guillain-barré syndrome. N Engl J Med. 2012;366(24):2294-2304.
[Google Scholar] [PubMed]
- Beghi E, Kurland LT, Mulder DW, Wiederholt WC. Guillain-Barré syndrome: Clinicoepidemiologic features and effect of influenza vaccine. Arch Neurol.1985;42(11):1053-1057.
[Google Scholar] [PubMed]
- Hadden RD, Cornblath DR, Hughes RA, Zielasek J, Hartung HP, Toyka KV, et al. Plasma Exchange/Sandoglobulin Guillain‐Barré Syndrome Trial Group. Electrophysiological classification of Guillain‐Barré syndrome: Clinical associations and outcome. J Neurol. 1998;44(5):780-788.
[Crossref] [Google Scholar] [PubMed]
- McKhann GM, Cornblath DR, Griffin JW, Ho TW, Li CY, Jiang Z, et al. Acute motor axonal neuropathy: A frequent cause of acute flaccid paralysis in China. Ann Neurol. 1993;33(4):333-342.
[Google Scholar] [PubMed]
- Griffin JW, Li CY, Ho TW, Tian M, Gao CY, Xue P, et al. Pathology of the motor‐sensory axonal Guillain‐Barré syndrome. Ann Neurol. 1996;39(1):17-28.
[Google Scholar] [PubMed]
- Hughes RA, Swan AV, Raphaël JC, Annane D, van Koningsveld R, van Doorn PA. Immunotherapy for Guillain-Barré syndrome: A systematic review. Brain. 2007;130(9):2245-2257.
[Google Scholar] [PubMed]
- Van den Berg B, Walgaard C, Drenthen J, Fokke C, Jacobs BC, Van Doorn PA. Guillain-Barré syndrome: Pathogenesis, diagnosis, treatment and prognosis. Nat Rev Neurol. 2014;10(8):469-482.
[PubMed]
- Desforges JF, Ropper AH. The Guillain-Barré Syndrome. N Engl J Med. 326(17):1130-1136.
[PubMed]
- Hiraga A, Mori M, Ogawara K, Hattori T, Kuwabara S. Differences in patterns of progression in demyelinating and axonal Guillain-Barré syndromes. Neurol. 2003;61(4):471-474.
[Google Scholar] [PubMed]
- Drenthen J, Jacobs BC, Maathuis EM, Van Doorn PA, Visser GH, Blok JH. Residual fatigue in Guillain-Barre syndrome is related to axonal loss. Neurol. 2013;81(21):1827-1831.
[Google Scholar] [PubMed]
- Hughes RA, Hadden RD, Rees JH, Swan AV. The Italian Guillain-Barré Study Group. The prognosis and main prognostic indicators of Guillain-Barré syndrome: A multicentre prospective study of 297 patients. Brain: J Neurol. 1998;121(4):767-769.
[Google Scholar] [PubMed]
- Sudulagunta SR, Sodalagunta MB, Sepehrar M, Khorram H, Raja SK, Kothandapani S, et al. Guillain-Barré syndrome: Clinical profile and management. Ger Med Sci. 2015;13.
- Dhadke SV, Dhadke VN, Bangar SS, Korade MB. Clinical profile of Guillain Barre syndrome. J Assoc Physicians. 2013;61(3):168-172.
[PubMed]
- McGrogan A, Madle GC, Seaman HE, De Vries CS. The epidemiology of Guillain-Barré syndrome worldwide: A systematic literature review. Neuroepidemiol. 2009;32(2):150-163.
[Google Scholar] [PubMed]
- Orlikowski D, Prigent H, Sharshar T, Lofaso F, Raphael JC. Respiratory dysfunction in Guillain-Barré syndrome. Neurocrit Care. 2004;1:415-422.
[Google Scholar] [PubMed]
- Samadi M, Kazemi B, Oskoui SG, Barzegar M. Assessment of autonomic dysfunction in childhood guillain-barré syndrome. J Cardiovasc Thorac Res. 2013;5(3):81.
[Google Scholar] [PubMed]
- Tian J, Cao C, Li T, Zhang K, Li P, Liu Y, et al. Electrophysiological subtypes and prognostic factors of Guillain-Barre syndrome in northern China. Frontiers Neurol. 2019;10:714.
- Ho TW, Mishu B, Li CY, Gao CY, Cornblath DR, Griffin JW, et al. Guillain-Barre syndrome in northern China Relationship to Campylobacter jejuni infection and anti-glycolipid antibodies. Brain. 1995;118(3):597-605.
[Google Scholar] [PubMed]
- Winner SJ, Evans JG. Guillain-Barré syndrome in Oxfordshire: Clinical features in relation to age. Age Ageing. 1993;22(3):164-170.
[Google Scholar] [PubMed]
- González-Suárez I, Sanz-Gallego I, Rodríguez de Rivera FJ, Arpa J. Guillain-Barré syndrome: Natural history and prognostic factors: A retrospective review of 106 cases. BMC Neurol. 2013;13:1-6.
[Google Scholar] [PubMed]
- Bernsen RA, Jacobs HM, De Jager AE, Van der Meche FG. Residual health status after Guillain-Barre syndrome. J Neurol Neurosurg Psychiatry Res. 1997;62(6):637-640.
[Google Scholar] [PubMed]
- Eiben RM, Gersony WM. Recognition, prognosis and treatment of the Guillain-Barré syndrome (acute idiopathic polyneuritis). Med Clin N Am. 1963;47(5):1371-1380.
[Google Scholar] [PubMed]
- Andersson T, Sidén Å. A clinical study of the Guillain‐Barré syndrome. Acta Neurol Scand. 1982;66(3):316-327.
- Doets AY, Verboon C, Van Den Berg B, Harbo T, Cornblath DR, Willison HJ, et al. Regional variation of Guillain-Barré syndrome. Brain. 2018;141(10):2866-2877.
[Google Scholar] [PubMed]
- Rostásy KM, Huppke P, Beckers B, Brockmann K, Degenhardt V, Wesche B, et al. Acute MNotor and Sensory Axonal Neuropathy (AMSAN) in a 15-year-old boy presenting with severe pain and distal muscle weakness. Neuro Pediatr. 2005;36(4):260-264.
- Ward IM, Fewell AE, Ferraro DM, Morris MJ. Concurrent acute motor and sensory axonal neuropathy and immune thrombocytopenic purpura. Mil Med. 2013;178(3):367-371.
[Google Scholar] [PubMed]
Citation: Daoud MHS, Mohmed MHA, Saeed MK, Ahmed AETM, Ibrahim EAA, Mohammed OEAH, et al. (2024) Outcome of Guilian Barre’- Syndrome Using Clinical and Electrophysiological Parameters in Three Neurology Centers-Sudan. Bio Med. 15:632.
Copyright: © 2024 Daoud MHS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


