Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 17, Issue 4
Obstetric Near Miss in Northwest Ethiopia, Has a Pregnant Woman Still 'One Foot in the Grave'?
Selamawit Lake Fenta1*, Azezu Asres Nigussie1, Simachew Animen Bante1, Eyaya Misgan Asres2 and Martha Hoffman Goedert32Department ofObstetrics and Gynecology, College of Medicine and Health Sciences, Bahir Dar Universit, Bahir Dar, Ethiopia
3College of Public Health, University of Nebraska Medical Center, Bahir Dar, Ethiopia
Received: 25-Jun-2020 Published: 27-Jul-2020, DOI: 10.35248/2090-7214.20.17.353
Abstract
Background: Globally obstetric near misses occur in larger numbers than maternal deaths. In the developing countries the unacceptably high maternal mortality overshadows severe maternal morbidity. In Ethiopia a woman is said “ gulbete dekama ” when she get pregnant to mean she is incapacitated and congratulated when she has successfully given birth as “enkuan fetari aterefesh” to mean ‘well survived’. Severe obstetric morbidity continues to be a neglected dimension of maternal health, unlike maternal death. This study aimed at assessing proportion and factors associated with obstetric near miss in Northwest Ethiopia.
Methods: An institution based cross sectional study was conducted from March to April 2017. Data was collected using a pre-tested questionnaire with systematic random sampling technique among 501 participants and analyzed through SPSS. Both bivariable and multivariable logistic regressions were computed. A P-value less than 0.05 were considered statistically significant at 95% confidence level.
Results: Overall, 116 (23.2%; 95%CI:19.1-26.64) of the mothers were having obstetric near misses. The mean age was 26.12 ± 5.6, and the median distance a woman travelled to reach at this facility was 40 kilometers. Age of woman[AOR=3.6; 95%CI:1.29-9.93], marital status[AOR=4.3; 95%CI:1.61-9.12], gravidity[AOR=3.9; 95%CI: 1.74-8.84] and [AOR=2.5; 95%CI:1.14-5.23], antenatal care[AOR=0.1; 95%CI:0.03-0.61], birth weight[AOR=2.2; 95%CI:1.01-4.95], length of hospital stay[AOR=7.3; 95%CI:3.76-13.01] and mode of delivery[AOR=3.5; 95%CI: 1.72-7.22] and [AOR=3.5; 95%CI:1.21-11.13], were significantly associated with obstetric near miss.
Conclusions: The proportion of obstetric near misses was found to be high. Hemorrhagic disorders were the most common event of near miss. Risk of near miss was increased in mothers with extreme age, non-married, not having antenatal care, birth by cesarean section and longer hospital stay.
Keywords
Maternal near miss, Severe morbidity, Felege Hiwot comprehensive specialized referral hospital, Bahir Dar University
Background
The burden of maternal mortality is only a small fraction of the burden of maternal morbidity; the health problems borne by women during pregnancy and the postpartum period. Maternal deaths have been described as the tip of the iceberg and maternal morbidity as the base. Yet, women who survive lifethreatening conditions arising from complications related to pregnancy and childbirth have many common aspects with those who die of such complications [1, 2]
World Health Organizations [WHO] estimate reflects the difficulty in calculating and characterizing the profile of maternal mortality in Africa. This difficulty is attributed to its rare occurrence, incomplete vital registries, to the undernotification of causes of maternal death and to the dispersion of the cases over the wide geographical area involved. So this difficulty of investigating deaths of mother with underlined causes of death will lead us to the concept of near miss or severe maternal morbidities. The practical implementation of maternal near miss concept should provide an important influence to improving quality of obstetric care to reduce maternal mortality and optimize their health [3, 4].
World health organization defined situations where women nearly died during pregnancy, childbirth or after pregnancy and they survived either by chance or because of the good institutional care they received as maternal near-miss. Their complications are so severe that their chance of survival without any clinical assistance is very small. MNM is increasingly identified as useful means to examine quality of obstetric care since pregnancy complications occur in 15% of women worldwide [3, 5].
For every maternal death, there are close to 100 women with severe maternal morbidity referred to as maternal near miss. Although near-miss events occur more frequently than maternal deaths, it continues to be a neglected dimension of maternal health. While being alert of the pregnancy complications is much appreciated, in Ethiopia, a woman is said “ gulbete dekama” when she get pregnant to mean she is incapacitated and congratulated when she has successfully given birth as “enkuan fetari aterefesh” to mean ‘well survived’ [6, 7].
So as to investigate maternal near miss in diverse countries by different researchers three types of criteria have been used. The first one is the organ system criteria proposed by the World Health Organization to enable international comparison. And the second is the clinical criteria based on complications to enable comparison over time with previous studies. The last one is the management criterion which enables us to identify near misses based on the clinical management they received [8-10].
Most of Ethiopia’s population still suffer high rate of maternal morbidity and mortality. Even if Ethiopia ’ s Health Sector Development Program [HSDP] advert the importance of increasing access to high reproductive health care and increasing access to skilled delivery, we are unable to prevent pregnancy related complications [11-14].
This study was therefore conducted to determine the proportion and associated factors of obstetric near miss events at Felege Hiwot Specialized Referral Hospital, Northwest Ethiopia. Causes of near miss were also determined.
Methods
Study Setting and Period
Facility based cross sectional study using medical record was conducted from March to April 2017 at Felege Hiwot specialized referral hospital, Bahir Dar City, Northwest Ethiopia.
Study Population
All women who were admitted to obstetrics & gynecologic wards; during antenatal, intrapartum or within 42 days after delivery from January 1st to December 31st 2016 are the study populations.
Sample Size and Sampling Techniques
Sample size was estimated using Epi Info™ 7 StatCalc command considering 95% confidence level, OR=1.7 [15], 80% power, and adding 5% non-response rate. The sample size was estimated to be 519. All women delivered and admitted for pregnancy related services were identified through log book. After proportionally allocating the samples in each unit of admission, systematic random sampling technique was used.
Study Variables
Dependent variable in this study is obstetric near miss while the independent variables were grouped into seven categories. These are socio-demographic variables, past obstetric and gynecological variables, present client obstetric variables, current pregnancy outcome, maternal health services, condition of near misses and professional factors.
Data collection and management
Data were collected from patient’s case note by using structured format adapted from WHO standard questions [16, 17]. It has all the necessary variables in accordance with the objective of the study and it is a written English version. obstetric near miss cases were identified based on Waterstone and Bewley ’ s maternal near miss criteria [9, 16]. To assure the quality of data training was given for facilitators and supervisors, pretest was done. Each day collected information was reviewed and errors were returned to facilitators for correction. Supervisors and investigators closely supervised data collection technique.
Data processing and analysis
Data were entered to Epi Info™ 7 and exported to SPSS version 20 for analysis. Variables having P < 0.05 in multivariable logistic regression analysis were considered statistically significant. Odds ratios with 95% confidence interval were computed to assess the presence and degree of association between the dependent and independent variables.
Results
Socio-demographic characteristics of mothers
A total of 501 patient charts were reviewed with a response rate of 96.5%. The age of mothers ranged between 17 and 47 years, and the mean age was 26.12 ± 5.6. About 445[88.5%] of study participants were in the age< 35 years. Majority, 484 [96.6%] of them were married, and 295 [58.9%] of women were resided in urban areas. The median distance that a woman travelled to reach at this facility was 40 kilometers. Nearly two third [62.9%] of women were traveled more than ten kilometers (Table 1).
| Characteristics | Frequency | Percent (%) |
|---|---|---|
| Age | ||
| <35 years | 445 | 88.8 |
| =35 years | 56 | 11.2 |
| Marital status | ||
| Single | 17 | 3.4 |
| Married | 484 | 96.6 |
| Residence | ||
| Urban | 295 | 58.9 |
| Rural | 206 | 41.1 |
| Distance travelled to reach at facility | ||
| <10 Kilometers | 186 | 37.1 |
| =10 Kilometers | 315 | 62.9 |
Table 1 : Socio-demographic characteristics of mothers, Felege Hiwot Specialized Referral Hospital, Northwest Ethiopia, April 2017 (n= 501).
Proportion of obstetric near misses
From a total of 501 charts reviewed 116 [23.2%; 95% CI: 19.1-26.64] were identified as near misses 174 near miss events and there was no maternal death. Obstetric hemorrhage accounted for 31% of near miss cases, followed by 26.7% of pregnancy induced hypertension [Fig 1]. Whereas; severe anemia was the major contributing cause of near misses. Majority, 69[59.5% %], of near misses were occurred at home followed by 29.3% at this referral hospital. Most of [81.9%] near misses had their pregnancy terminated at this referral hospital.
Factors associated with maternal near miss
In multiple logistic regression model; mothers aged ≥ 35 years were 3.6 times more likely to develop near miss than those aged < 35 years [AOR=3.6; 95%CI[1.29-9.93]]. Single marital status increases the risk of development of near miss by 4.3 times comparing to married once [AOR=4.3; 95%CI [1.61-9.12]]. Primigravidas and gravida four and above were 3.9 and 2.3 times having increased chance of developing near miss than those who got pregnant for 2 to 3 times respectively [AOR=3.9; 95%CI [1.74-8.84]] and [AOR=2.5; 95%CI: [1.14-5.23]] (Figure 1).
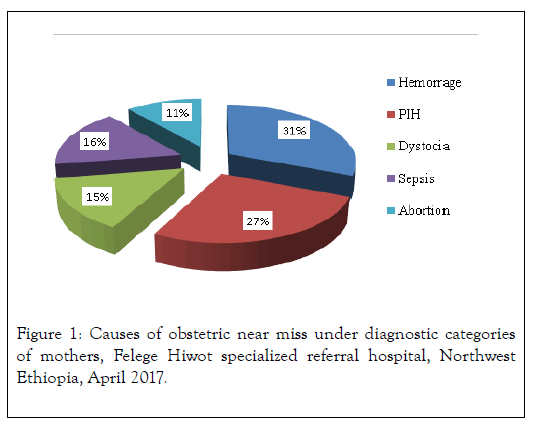
Figure 1 : Causes of obstetric near miss under diagnostic categories of mothers, Felege Hiwot specialized referral hospital, Northwest Ethiopia, April 2017.
Having attended antenatal care follow-up decreases the risk of near miss by ten times [AOR=0.1; 95%CI: [0.03-0.61]]. Those mothers who gave birth by cesarean section and instrumental delivery were 3.5 times more likely to develop near miss event than those having spontaneous vaginal delivery. [AOR=3.5; 95%CI: [1.72-7.22]] and [AOR=3.5; 95%CI: [1.12-11.13]]. In addition, birth weight of a newborn 1500-2499 grams increases the odds of MNM by 2.2 times [AOR=2.2; 95%CI: [1.01-4.95]].Also Women who stayed for 7 and more days were exposed to near miss by 7.3 times than their counterparts [AOR=7.3; 95%CI: [3.76-13.01]] (Table 2).
| Variables | Near miss | COR(95%CI) | AOR(95%CI) | P-value |
|
|---|---|---|---|---|---|
| Yes | No | ||||
| (n=116) | (n=385) | ||||
| Age | |||||
| <35 Years | 93 | 352 | 1 | 1 |
|
| =35Years | 23 | 33 | 2.6(1.49-4.71) | 3.6(1.29-9.93) | 0.014 |
| Marital status | |||||
| Married | 376 | 108 | 1 | 1 |
|
| Single | 9 | 8 | 3.1(1.2-8.2) | 4.3(1.61-9.12) | 0.013 |
| Residence | |||||
| Urban | 51 | 244 | 1 | 1 |
|
| Rural | 65 | 141 | 2.2(1.43-3.42) | 1.8(0.79-3.92) | 0.167 |
| Gravidity | |||||
| Gravida 1 | 47 | 166 | 4.5(2.50-8.03) | 3.9(1.74-8.84) | 0.001 |
| Gravida 2-3 | 21 | 145 | 1 | 1 |
|
| Gravida =4 | 48 | 74 | 1.91.12-3.43) | 2.5(1.14-5.23) | 0.013 |
| ANC visit? | |||||
| No | 25 | 20 | 1 | 1 |
|
| Yes | 91 | 365 | 0.2(0.11-0.38) | 0.1(0.03-0.61) | 0.01 |
| Duration of labour(n=402) | |||||
| <12 hours | 16 | 132 | 1 | 1 |
|
| 12-24 hours | 36 | 144 | 2.1(1.09-3.89) | 1.8(0.74-4.34) | 0.194 |
| 24-48 hours | 18 | 56 | 2.7(1.29-5.74) | 2.0(0.74-5.55) | 0.166 |
| Was a parthograph used?(n=402) | |||||
| Yes | 26 | 224 | 1 | 1 |
|
| No | 13 | 70 | 1.6(.78- 3.28) | 1.2(0.47-3.24) | 0.078 |
| Not a candidate | 31 | 38 | 7.0(3.76-13.12) | 1.7(0.54-5.15) | 0.372 |
| Birth weight(n=421) | |||||
| 1000-1499gms | 5 | 8 | 3.3(1.04-10.46) | 4.6(0.41-50.77) | 0.078 |
| 1500-2499gms | 19 | 38 | 2.6(1.41-4.10) | 2.2(1.01-4.95) | 0.046 |
| 2500-3999gms | 52 | 274 | 1 | 1 |
|
| =4000gms | 6 | 19 | 1.7(0.63-4.36) | 4.1(1.09-15.38) | 0.343 |
| Admission to delivery time | |||||
| 94 | 271 | 1 | 1 |
|
|
| 22 | 114 | 0.6(0.33-0.93) | 0.9(0.39-2.28) | 0.908 |
|
| Length of hospital stay | |||||
| £7da?s | 93 | 375 | 1 | 1 |
|
| >7days | 23 | 10 | 7.3(4.23-12.14) | 7.1(3.76-13.01) | 0 |
| Final mode of delivery (n=443) | |||||
| Vaginal | 35 | 247 | 1 | 1 |
|
| Cesarean delivery | 41 | 95 | 3.0(1.83-5.07) | 3.5(1.72-7.22) | 0 |
| Assisted vaginal delivery | 10 | 15 | 4.7(1.96-11.29) | 3.5(1.12-11.13) | 0.001 |
| Referred from other institution | |||||
| No | 7 | 90 | 1 | 1 |
|
Yes |
109 |
295 |
4.7(2.11-10.52) |
2.5(0.61-10.51) |
0.203 |
Table 2: Associated factors of obstetric near miss among admitted mothers, Felege Hiwot specialized referral hospital, Northwest Ethiopia, April 2017.
Discussion
Although pregnancy complications are to a great extent unpredictable and unpreventable, early awareness of near miss cases can prevent the progress of disease and maternal death [18].
This study showed that proportion of obstetric near miss in the mothers was 23.2%. This result is consistent with studies done in Ethiopia [19-21] but very high compared to other studies in other parts of the world [22-27]. The possible reason for this difference might be ours is a specialized referral hospital covering many other districts around Bahir Dar, with most of the cases being referred in an already moribund state. The delays in referrals, delayed diagnosis, inappropriate transfer, and inadequate utilization of resources might have been the cause for maternal morbidities in our study.
Hemorrhagic and hypertensive disorders were the two leading causes of maternal near miss in our study. It was observed that obstetric hemorrhage occupied the highest portion, and this is in agreement with its locus as the commonest cause of maternal death most often found globally. This finding is consistent with studies done at several countries including Ethiopia. From these hemorrhagic disorders, primarily postpartum hemorrhage accounted for 47%; is consistent to the mentioned studies [22, 23, 28-30]. Form hypertensive disorders severe preeclampsia contributed to 65.6%. Severe preeclampsia was the diagnosis which occurs most frequently during primary admission.
This study showed significant association between extreme maternal age [≥35 years] and the occurrence of near miss which is in agreement with studies done at Latin America, USA and Brazil but inconsistent with a study done at Thailand, Sisaket which showed the two extreme maternal ages were protective of near miss. [20, 31-34]. This result is explained as mothers above the age of 35 usually have previous birth experience making them less concerned about the pregnancy as they have the familiarity so they are hesitant about routine follow ups or come late. Moreover, they are at risk of diabetes, obstetric hemorrhage, anemia due to repeated birth, malpresentations which begins from simple labour protraction to catastrophic conditions like ruptured uterus.
This study indicated that single marital status is a risk factor for development of near miss a similar result was shown in a study done at eight Latin American countries and Nigeria [26, 32]. However, this idea is in contrast with a study done at Thailand which shows single marital status is a protective factor for near miss [31]. The disagreement may due to the fact that in developed countries women are empowered and not economically dependent so they can cover every health cost by themselves and no delay in seeking care.
This study depicted that having ANC follow up decreases the risk of developing near miss. This finding is very much similar to other studies done in Ethiopia, Bolivia and Brazil [19, 20, 24, 35]. This can be explained possibly as mothers who look for ANC services have a better health seeking behavior. ANC acts as an enabler of timely arrival for emergency obstetric care. Women who receive antenatal care are more likely to receive skilled birth attendants for delivery and postpartum care.
Mode of delivery was found to be an important predictor of maternal near miss. In this study cesarean section and assisted vaginal or instrumental deliveries were strongly associated with maternal near miss. This result is consistent with studies done at Brazil, Nigeria and Thailand [24, 26, 30, 31, 36]. A possible explanation for this may be related to the survival of a near miss rather than being a risk factor due to the temporal sequence of the events. This is because such treatment modalities are employed after the occurrence of a complication and not conversely.
In this study it was found that birth weight of a newborn was significantly associated with maternal near miss. This result shows consistency with a study done at Nigeria, Thailand and Latin America which revealed a positive association between low birth <2500gms and maternal near miss [26, 31, 32]. A possible explanation for this is; maternal morbidities like severe preeclampsia and severe antepartum hemorrhage have increased risk of prematurity and low birth weight through pathologic and iatrogenic for urgent gestational resolution. The fact that 71% proportion of low birth weight [<2500gms] among near misses in this study also supports the evidence. And in a study done at Brazil cesarean delivery was the main route of delivery for this preterm births [37], in that case cesarean increases morbidity in the woman as aforementioned in this study as well.
This study revealed that mother who stayed for longer than seven days were at increased risk of near miss. This is consistent with study done in Amhara region hospitals and a study done in Latin America [19, 38]. The reason for this could be related to the onset of some postpartum and post-abortal infection morbidities often occur after five to seven days of termination of pregnancy. Furthermore, prolonged stay at the hospitals for other therapeutic indications by itself limits mobility and a mother could have other morbidities like deep venous thrombosis and athelectatic pneumonia. However, cause and effect reasoning is not possible in cross-sectional study design, and regardless, the related underlying conditions should be identified first.
The major limitation of the study was that ideally, the definition of maternal near miss should be based on organ dysfunction criteria to have international comparison but availability and use corresponding resources was the important obstacle in our study. Additionally, data recorded in medical charts, individual clinicians’ differences on diagnosis of disease, which may not have been fully standardized also limits this study.
Conclusions
This study demonstrated high prevalence of obstetric near miss. In this study hemorrhage and hypertensive disorders were common cause of morbidity. We recommended awareness creation should be given about importance of utilizing reproductive health services like antennal care and family planning and establish hospital guidelines to safely lower the rate of cesarean and assisted vaginal deliveries are recommended.
Ethics Approval
Ethical clearance for this study was obtained from Bahir Dar University, College of Medicine and Health Sciences Institutional Review Board. Amhara Regional State Health Bureau, Research and Technology Transfer Core Process approved ethical clearance to collect data from the medical record. As the data is collected from individual medical records, neither written nor verbal consent is obtained from participants. However confidentiality of the information was possibly maintained throughout the study by excluding personal identifiers.
Consent for Publication
Not applicable
Availability of Data and Materials
The selected data sets supporting the conclusion of this manuscript are included in the manuscript. However, the raw datasets used in the current study are available from the corresponding author on reasonable request.
Competing Interests
All the authors declare that they have no competing interests.
Authors' Contributions
SLF: conceived of the presented idea, verified the design, and analyzed the data, wrote the draft manuscript with support from AAN, EMA and MHG
AAN: approved the design, supervised the findings of this work and wrote the draft manuscript
SAB: analyzed the data, revised subsequent drafts of the paper and reviewed the manuscript
EMA: revised the draft manuscript and final approval of the version to be published
MHG: revised subsequent drafts of the manuscript
All authors discussed the results and contributed to the final manuscript.
Acknowledgements
We would like to thank Bahir Dar University College of Medicine and Health Sciences for the technical support and assistance of this research. We are also grateful to Amhara regional health bureau research and technology transformation core processor and Felege Hiwot Comprehensive Referral Hospital for their kind assistance in offering the important information during proposal preparation and in the final data collection.
REFERENCES
- Alkema LCD, Hogan D, Zhang S, Moller AB, Gemmill A, Fat DM, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. The Lancet. 2016;30(387):462-474.
- Reichenheim ME ZF, Moraes CL, Lobato G. Severe acute obstetric morbidity (near-miss): a review of the relative use of its diagnostic indicators. Archives of gynecology and obstetrics. 2009;280(3):337-343.
- C FV. Reviewing severe maternal morbidity: learning from women who survive life-threatening complications.
- A W. Maternal mortality: it’s time to get political. BJOG: An International Journal of Obstetrics & Gynaecology. 2007;114(2):125-126.
- AbouZahr C WT. Maternal mortality at the end of a decade: signs of progress. Bulletin of the World Health Organization. Bulletin of the World Health Organization. 2001;79:561-573.
- L PR, Gülmezoglu AM. WHO systematic review of maternal morbidity and mortality: the prevalence of severe acute maternal morbidity (near miss). Reproductive health. 2004;1(1):3.
- Galvão LPL, de Mendonça CM, Menezes FE, do Nascimento Góis KA, Ribeiro Jr RF, Gurgel RQ. The prevalence of severe maternal morbidity and near miss and associated factors in Sergipe, Northeast Brazil. BMC pregnancy and childbirth. 2014;14(1):25.
- Souza JP CJ, Parpinelli MA, Serruya SJ, Amaral E. Appropriate criteria for identification of near-miss maternal morbidity in tertiary care facilities: a cross sectional study. BMC pregnancy and childbirth. 2007;7(1):20.
- M MJ, Bewley S, Wolfe C. Incidence and predictors of severe obstetric morbidity: case-control studyCommentary: Obstetric morbidity data and the need to evaluate thromboembolic disease. Bmj. 2001;322(7294):1089-1094.
- Say L SJ, Pattinson RC. Maternal near miss-towards a standard tool for monitoring quality of maternal health care. Best Practice & Research Clinical Obstetrics & Gynaecology. 2009;23(3):287-296.
- Ambel AA AC, Bakilana AM, Foster EM, Khan Q, Wang H. Examining changes in maternal and child health inequalities in Ethiopia. International journal for equity in health. 2017;16(1):152.
- Karim AM AK, Schellenberg J, Alemu H, Getachew N, Ameha A, Tadesse L, et al. Effect of Ethiopia’s health extension program on maternal and newborn health care practices in 101 rural districts: a dose-response study. PLoS One. 2013;8(6):e65160.
- Say L RR. A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bulletin of the World Health Organization. 2007;85:812-819.
- T L, AD MA. Trends and causes of maternal mortality in Jimma University specialized Hospital, southwest ethiopia: a matched case–control study. International journal of women's health. 2017;9:307.
- Mulugeta D, Tewodros S. Proportion of Maternal Near Misses and Associated Factors in Referral Hospitals of Amhara Regional State, Northwest Ethiopia: Institution Based Cross Sectional Study. Gynecol Obstet (Sunnyvale). 2015;5(308):2161-0932.
- World Health Organization. Evaluating the quality of care for severe pregnancy complications: the WHO near-miss approach for maternal health. 2011.
- Souza JP CJ, Haddad SM, Parpinelli MA, Costa ML, Katz L, Say L. The WHO maternal near-miss approach and the maternal severity index model (MSI): tools for assessing the management of severe maternal morbidity. PloS one. 2012;7(8):e44129.
- EDHS. Trends in Maternal Health in Ethiopia: In -depth Analysis of the EDHS 2000-2011 Addis Ababa. 2012.
- MekangoDE, Alemayehu M, Gebregergs GB, Medhanyie AA, Goba G. Determinants of maternal near miss among women in public hospital maternity wards in Northern Ethiopia: A facility based case-control study. PLoS ONE. 2017;12(9):e0183886.
- Gedefaw Molla GH, Gizachew Ayu, Taddess F. Assessment of Maternal Near Miss at Debre Markos Referral Hospital, Northwest Ethiopia: Five Years Experience. Open Journal of Epidemiology. 2014;4:199-207.
- Souza JP SM, Parpinelli MA, Amaral E, Cecatti JG. Self-reported maternal morbidity and associated factors among Brazilian women. Rev Assoc Med Bras. 2008;54:249-255.
- Noor Norhayati NH, Zaharah Sulaiman, Mohd Yacob Azman. Severe maternal morbidity and near misses in tertiary hospitals, Kelantan, Malaysia: a cross-sectional study. BMC Public Health. 2016;16(229):1-7.
- Mazhar SB BA, Emanuel A, Khan AT, Bhutta S. Severe maternal outcomes and their predictors among Pakistani women in the WHO Multicountry Survey on Maternal and Newborn Health. Gynaecol Obstet. 2015;129(1):30-33.
- Marcos Augusto Bastos Dias RMSMD, Arthur Orlando Corrêa Schilithz, Marcos Nakamura-Pereira, Carmen Simone Grilo Diniz, Ione Rodrigues Brum and et.al. Incidence of maternal near miss in hospital childbirth and postpartum: data from the Birth in Brazil study. Cad Saúde Pública. 2014;30:1-12.
- Stephen Rulisa IU, Maria Small, Jos van Roosmalen. Maternal near miss and mortality in a tertiary care hospital in Rwanda. BMC Pregnancy and Childbirth. 2015;15(203):1-5.
- Ikeola A Adeoye. Incidence, determinants and perinatal outcomes of near miss maternal morbidity in Ile-Ife Nigeria: a prospective case control study. BMC Pregnancy and Childbirth. 2013;13(93):1-4.
- Ayele Babusha. Prevalence of maternal near miss and maternal death in Atat Hospital, Ethiopia. Journal of Women's health issues and care. 2014;3(6)-1-5.
- Tayebeh Naderi SF, Samaneh Omidi, Faezeh Samadani and Nouzar Nakhaee. Incidence and Correlates of Maternal Near Miss in Southeast Iran. Hindawi. 2015.
- Oladapo OT S-OA, Olatunji AO, Daniel OJ. Near-miss obstetric events and maternal deaths in Sagamu, Nigeria a retrospective study. Reproductive Health. 2005;2(9):1186-1195.
- Cecatti JG SR, Pacagnella RC, Leal MC, Moura EC, Santos LMP. Maternal near miss among women using the public health system in the Amazon and Northeast regions of Brazil. Pan American Journal of Public Health. 2015;37(4/5):232-238.
- Wianwiset W. The incidence of maternal near miss cases (severe morbidity), their near miss events and obstetric outcomes at Sisaket Hospital, Thailand. Thai Journal of Obstetrics and Gynecology. 2012;20:69-76.
- João Paulo Souza JGC, Anibal Faundes, Sirlei Siani Morais, Jose Villar, Guillermo Carroli et al. Maternal near miss and maternal death in the World Health Organization’s 2005 global survey on maternal and perinatal health. Bull World Health Organ. 2010;88(113-119):1-8.
- J CJ, Parpinelli M, Sousa M, Lago T, Pacagnella R, Camargo R. Maternal morbidity and near miss in the community: findings from the 2006 Brazilian demographic health survey. BJOG. 2010;117:1586-1592.
- Goffman D MR, Harrison EA, Merkatz IR, Chazotte C Predictors of maternal mortality and nearmiss maternal morbidity. Perinatol 2007;27:597.
- Roost M AV, Liljestrand J, Essen B. Does antenatal care facilitate utilization of emergency obstetric care? A case-referent study of near miss morbidity in Bolivia. Acta Obstet Gynecol Scand 2010;89:335-342.
- Larissa Paes Leme Galvão FA-P, Caio Menezes Machado de Mendonça, Filipe Emanuel Fonseca Menezes, Kaique Andre do Nascimento Góis, Ruy Farias Ribeiro Jr, Ricardo Queiroz Gurgel. The prevalence of severe maternal morbidity and near miss and associated factors in Sergipe, Northeast Brazil. BMC Pregnancy and Childbirth. 2014;14(25):1-3.
- Oliveira Leonam Costa. Fetal and neonatal deaths among cases of maternal near miss. Rev Assoc Med Bras. 2013;59(5):487-494.
- Lotufo FA, Haddad SM, Surita FG, Cecatti JG. Applying the new concept of maternal near-miss in an intensive care unit. University of Campinas, Obstetrics and Gynecology, Campinas/SP, Brazil. Clinics 2012;67(3):225-230.
Citation: Fenta SL, Nigussie AA, Bante AS, Asres EM, Goedert MH (2020) Obstetric Near Miss in Northwest Ethiopia, Has a Pregnant Woman Still ‘One Foot in the Grave’?. Clinics Mother Child Health. 17: 353. DOI: 10. 35248/2090-7214. 20. 17. 353.
Copyright: © 2020 Fenta SL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

