Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 12, Issue 2
Novel Therapy with Hybrid Liposomes for Orthotopic Graft Mouse Models of Glioblastoma
Keiji Kuwabara, Hideaki Ichihara and Yoko Matsumoto*Received: 08-Feb-2021 Published: 01-Mar-2021, DOI: 10.35248/2157-2518.21.12.360
Abstract
Hybrid Liposomes (HL25) composed of 90 mol% L-a-Dimyristoylphosphatidylcholine (DMPC) and 10 mol% polyoxyethylene(25) dodecyl ethers (C12(EO)25) were found to fuse and accumulate in the cell membranes of human brain tumor, glioblastoma, (U-87MG) cells and inhibit their growth. HL25 induced apoptosis in U-87MG cells via the release of AIF under a caspase-independent pathway. HL25 inhibited tumor enlargement in orthotopic graft mouse models of glioblastoma after crossing the blood-brain barrier.
Keywords
Hybrid liposomes, Glioblastoma, Apoptosis, Cell membrane, AIF, In vivo, Blood brain barrier
Abbrevations
AIF: Apoptosis Inducing Factor; C12(EO)25, Polyoxyethylene(25) Dodecyl Ether; DMPC, L-α-dimyristoylphosphatidylcholine; HL25: Hybrid Liposomes composed of DMPC and C12(EO)25; NBDPC: 1-palmitoyl-2-[12-[(7-nitro-2-1,3-benzoxadiazol-4-yl) amino]-dodecanoyl]-sn-glycero-3-phosphocholine; TUNEL: Terminal Deoxynucleotidyl Tranferase-Mediated dUTP-Biotin Nick End Labeling.
Introduction
Brain disease is the generic name of the diseases that occur in the brain. In brain disease, a tumor growing intracranially is called a brain tumor. Examples of primary brain tumors include meningioma that occurs in the membrane surrounding the brain, neurilemmoma that occurs in the nerves sheath, pituitary adenoma that occurs in the pituitary gland, and glioma that occurs in the brain itself. The tumors of the meninges and glioma account for a quarter of all brain tumors. Glioblastoma accounts for 9% of the primary brain tumors, 36% of total glioblastoma, and it is the highest grade tumor of grade 4 [1]. Treatment of brain tumors generally includes surgery, radiotherapy, and chemotherapy with anticancer agents. Complete surgical removal of the tumor is the most effective option. However, if even a small quantity of cancer cells is left in place after surgery, the tumor can recur. In addition, a sophisticated technique is necessary for the removal of the tumor because the surrounding structures can become dysfunctional if they are injured during surgery. Besides, there is a challenge that anticancer agents hardly reach the brain tumor, because being macromolecular drugs; they cannot cross the Blood-Brain Barrier (BBB).
Hybrid Liposomes (HLs) are the excellent medical material to control the membrane fluidity, membrane diameter, and phase transition temperature by influencing the composition ratio [2-7]. HLs have been used for anticancer effects in various cancer cells in vitro and in vivo and induce apoptosis [3-7,8-13]. The therapeutic effects of HLs not containing encapsulated drugs, such as anticancer drugs in patients with lymphoma, have been reported [12]. HLs were used to distinguish lung cancer cells from normal lung cells, which have higher and lower membrane fluidities, respectively. They fuse and accumulate preferentially in the lung cancer cells [13]. However, the inhibitory activity of HL25 on the proliferation of glioblastoma cells has not yet been elucidated. In this study, we examined the anticancer effects and the apoptotic induction pathway of human brain tumor (glioblastoma, U-87MG) cells of HL25 composed of 90 mol% Dimyristoylphosphatidylcholine (DMPC), and 10 mol% polyoxyethylene(25)dodecyl ether (C12(EO)25). Furthermore, the chemotherapeutic effect of HL25 was examined using orthotopic graft mouse models of glioblastoma in vivo.
Materials and Methods
Preparation of HLs
BHL25 was prepared using a sonicator (VS-N300; VELVO, Tokyo, Japan) after DMPC (purity>99 %; NOF Co. Ltd., Tokyo, Japan) and C12(EO)25 (Nikko Chemicals Co., Ltd., Tokyo, Japan) were mixed in 5% glucose solution at 45 °C, 300 W and filtered with a 0.20 μm filter.
Dynamic light scattering measurements
The diameter (dhy) of HL25 was measured by a light scattering spectrometer (ELS-8000, Otsuka Electronics, Osaka, Japan) using a He-Ne laser (633 nm) at a scattering angle of 90°. dhy was calculated using the Stokes-Einstein formula (Equation 1), where κ is the Boltzmann constant, T is the absolute temperature, η is the viscosity, and D is the diffusion coefficient:
dhy=κ T/3πηD
Cell Culture
The human glioblastoma (U87MG) cell line was purchased from ATCC (VA, USA). U87MG cells were cultured in MEM medium (Gibco, Thermo Fisher Scientific, Inc. MA, USA) containing 10% fetal bovine serum (FBS, HyClone Laboratories Inc., UT, USA), penicillin (100 unit/ml), and streptomycin (50 μg/ml). The cells were then kept in a humidified incubator at 37 ˚C and 5% CO2.
Assessment of the half-maximal inhibitory concentration (IC50) of HL25 in vitro
The half-maximal inhibitory concentration (IC50) of HL25 on the growth of U87MG cells was determined based on a WST-8 [2-(2-methoxy-4-nitrophenyl)-3-(4-nitrophenyl)- 5-(2, 4-disulfophenyl)-2H tetrazolium, monosodium salt] assay (Cell Counting Kit-8, Dojindo Laboratories, Kumamoto, Japan) [14]. U87MG (5.0 × 103 cells/ml) cells were seeded in 96-well plates and cultured in a 5% CO2 humidified incubator at 37 °C for 24 h. The cells were cultured for a further 48 h after the addition of DMPC (0-2.0 × 10-3 M) and HL25 (-1.4 × 10-3 M depending on the DMPC concentration). WST-8 solution was then added and the mixture incubated for 3 h. The absorbance at a wavelength of 450 nm was measured using a microplate reader (Thermo, CA, USA). The inhibitory activity of HL25 on the growth of U87MG cells was evaluated by Amean/Acontrol, where Amean and Acontrol denote the absorbance of water-soluble formazan in the presence and absence of HL25, respectively.
Analysis of apoptosis induction by HL25 based on a PI assay using flow cytometry
The cells were seeded at a density of 5.0 × 103 cells per 100 ml on a dish and incubated in a humidified atmosphere of 5% CO2 at 37 °C for 24 h. HL25 (0.1-5.0×10-4 M depending on the DMPC concentration) was added to each dish and the dishes were incubated. The cells were centrifuged and suspended in PBS (-), containing 1 mg/ml RNase, 0.1% Triton X-100 and 40 μg/ml propidium iodide (PI, Molecular Probes, Eugene, OR, USA), in a dark room. The percentage of apoptotic cells was analyzed using a flow cytometer (Epics XL system II, Beckman Coulter, Brea, CA, USA) [15].
Terminal deoxynucleotidyl transferase-mediated dUTP-biotin nick end labeling (TUNEL) assay
Detection of apoptotic cells was performed by the TUNEL method using the In Situ Cell Death Detection Kit (Roche Diagnostics, Basel, Switzerland). U87MG cells (5 × 103 cells/ml) were seeded in dishes and cultured for 24 h.
HL25 ([DMPC]=3.0×10-4 M, [C12(EO)25]=3.33 × 10-5 M) or DMPC liposomes were added and the cells were cultured for another 48 h. Thereafter, 4% paraformaldehyde solution was added for fixation. After the removal of the formalin, the cells were washed with Hank's Balanced Salt Solution (HBSS). An impregnated solution was added and the cells were stored in darkness at 4 °C for 2 min. The cells were then washed and a TUNEL reaction mixture was added, after which, the cells were incubated at 37 °C for 60 min within a humectant box. Stained cells were observed under a confocal laser microscope (TCS-SP; Leica Microsystems, Wetzlar, Germany) with a 488 nm Ar laser line for TUNEL (detection at 515-565 nm).
Assessment of AIF by flow cytometry
U87MG cells (5.0 × 103 cells/ml) were seeded in dishes and incubated for 24 h. They were then treated with HL25 (3.0×10- 4 M) and incubated for 24 h. Next, they were fixed with 10% formaldehyde for 30 min in wells, followed by incubation with anti- AIF Alexa Fluor® 488-conjugated antibody (5 μg/ml) (Abcam plc, Cambridge, UK) in a shaded box at 4 °C for 1 h. Stained U87MG cells were analyzed by flow cytometry.
Fusion and accumulation of HL25 in the cell membrane
HL25 fusion and accumulation in the cell membrane was assessed using a confocal laser microscope (TCS-SP; Leica Microsystems, Berlin, Germany) and a fluorescent probe ((1-palmitoyl-2-[12-[(7- nitro-2-1,3-benzoxadiazol-4-yl)amino]-dodecanoyl]-sn- glycero-3- phosphocholine (NBDPC; Avanti Polar Lipids, Alabama, USA)). U87MG cells (2.0 × 104 cells/ml) were incubated in a humidified incubator at 37°C and 5% CO2 for 24 h. They were then treated with HL25/NBDPC ([DMPC]=99.6 μM, [C12(EO)25]=1.11 μM, [NBDPC]=0.4 μM) for 10-60 min and viewed under a confocal laser microscope using a 488 nm Ar laser line (detection at 505-555 nm).
Measurement of cellular membrane fluidity
The membrane fluidity of U87MG cells was measured using a spectrophotometer (F-7100; HITACHI) based on the fluorescence depolarization method [12]. U87MG cells were labeled with DPH (1, 6-diphenyl-1,3,5-hexatriene, Nacalai Tesque, Japan). The fluorescence depolarization (P) value of DPH in the cells treated with HL25 (1.0×10-4 M) was measured.
Assessment of the therapeutic effects of HL25 in vivo
All mice were handled in accordance with the guidelines for animal experimentation set out by Japanese law. The animal studies were approved by the Committee on Animal Research of Sojo University. BALB/c-R/J mice were kindly provided by Prof. Okada (Kumamoto University, Japan) [16].
The mice were bred using a 100% fresh ventilatory change of 14 times per hour at a room temperature of 25 ± 1 °C, a humidity of 50 ± 10%, and a light/dark cycle of 12 h. The mice were randomly grouped based on their body weight by the stratified randomization method. There were five mice in each group. U87MG cells (2.5 × 106 cells in 10 μL of Matrigel) were orthotopically implanted into the right-brains of anesthetized mice. HL25 (dose: 136 mg/kg for DMPC) was intravenously administered once each day for 29 days starting one day after the inoculation with U87MG cells. Brain samples were harvested from anesthetized mice and weighed after the completion of the HL25 administration regime.
Statistical analysis
Data are presented as mean ± S.D. For statistical comparison, Student’s t-test was performed. P<0.05 was considered to represent a statistically significant difference.
Results and Discussion
Physical Properties of HL25
We examined the morphology of HL25 based on dynamic light scattering. HL25 with a hydrodynamic diameter less than 100 nm remained viable for 4 weeks. In contrast, DMPC liposomes were unstable and precipitated at 14 days after preparation. These results suggest that HL25 with a diameter that is less than 100 nm can avoid recognition by the reticular endothelial system (RES) and therefore, would be appropriate for administration by intravenous injection both in vivo and in the clinic [17].
Inhibitory effect of HL25 on the growth of U87MG cells
We examined the inhibitory effect of HL25 on the growth of human glioblastoma (U-87MG) cells based on the WST-8 method. The IC50 values of HL25 were calculated from a plot of cell viability recorded at each test concentration versus the concentration of HL25. The results are shown in Figure 1A. The IC50 values of HL25 (160 μM) obtained for U-87MG cells were lower than those of the DMPC liposomes (240 μM). These results indicate that the inhibitory effect of HL25 is better than that of DMPC liposomes on the proliferation of U-87MG cells.
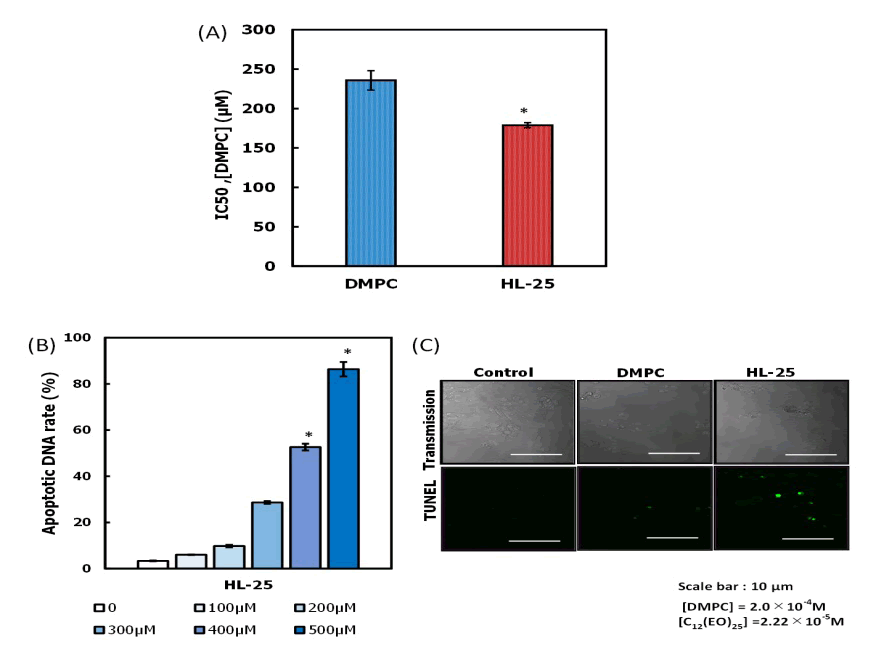
Figure 1:(A) Inhibitory effects of HL25 on the growth of human glioblastoma (U87MG) cells. p<0.05 (vs. DMPC) (B) Apoptotic DNA rate for U87MG cells treated with HL25 for 48h. *p<0.05 (vs. control) (C) Fluorescence micrographs of U87MG cells treated with HL25 for 24 h using the TUNEL method. [DMPC] = 3.0 × 10-4 M, [C12(EO)25]=3.33 × 10-5 M.
Apoptosis induction by HL25
The apoptosis induced by HL25 in U-87MG cells was evaluated based on a propidium iodide (PI) staining method using a flow cytometer. The results are shown in Figure 1B. Apoptotic DNA rates for U-87MG cells increased in a dose-dependent manner of HL25 and reached a high apoptosis rate of 90 %. We observed fragmentation of DNA in U-87MG cells by HL25 based on the TUNEL method using a confocal laser microscope. The results are shown in Figure 1C. A green fluorescence indicating the induction of apoptosis in U-87MG cells treated with HL25 was observed. In contrast, no green fluorescence was observed in U-87MG cells treated with DMPC liposomes. These results indicate that HL25 induced apoptosis in U-87MG cells.
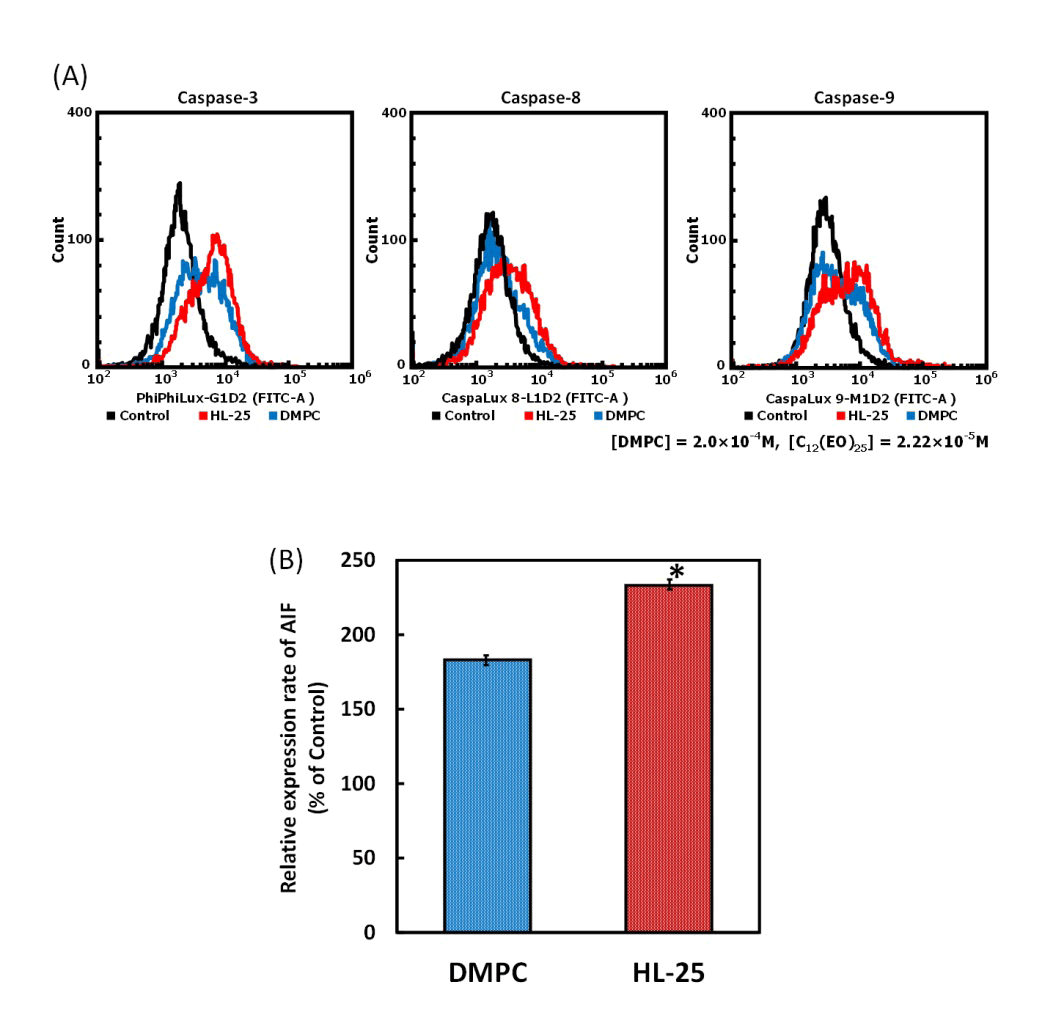
Figure 2:(A) Inactivation of caspase-3, -8, and -9 in U87MG cells treated with HL25. Data represent the mean ± S.E. Incubation time: 24 h. [DMPC] = 3.0×10-4 M, [C12(EO)25] = 3.33×10-5 M (B) Relative expression rate of AIF in U87MG cells after treatment with HL25 (40 μM) for 24 hours. Data represent the mean (n = 3) ± S.E. * p<0.05, vs. control and DMPC.
Apoptotic pathway in HL25-treated U87MG cells
We examined the pathway of apoptotic induction in U-87MG cells initiated by HL25. We measured the activation of caspase-3-8, and -9, to investigate the mechanism of induction of apoptosis in U-87MG cells treated with HL25 based on the fluorescence substrate assay using a flow cytometer. The results are shown in Figure 2A. No activation of caspase-3,-8, and -9, and substrate was observed in U-87MG cells after the treatment with HL25, suggesting that HL25 induced apoptosis of U-87MG cells without the activation of caspase-3,-8, and -9 shown in Figure 2B.
It is known that the Apoptosis-Inducing Factor (AIF) involves the caspase-independent pathway of apoptosis. The AIF in U-87MG cells treated with HL25 was measured by immunostaining and subsequently analyzed by flow cytometry. The results are shown in Figure 2C. The relative expression rate of AIF in U-87MG cells treated with HL25 was increased compared to the levels detected in DMPC liposome-treated cells. The data indicated that AIF was involved in the induction of apoptosis caused by HL25. These results suggest that HL25 induced apoptosis via AIF through a caspase-independent pathway.
HL25 fusion and accumulation in U87MG cells
The fusion and accumulation of HL25 in U-87MG cells were evaluated using flow cytometric analysis. The results are shown in Figure 3A. A time-dependent increase was observed in the fluorescence intensity of NBDPC (1-palmitoyl-2-[12-[(7- nitro-2-1,3- benzoxadiazol-4-yl) amino] dodecanoyl]-sn-glycero-3- phosphocholine) incorporated into HL25, indicating that HL25 was accumulated in U-87MG cells. We examined the membrane fluidity of U-87MG cells based on fluorescence polarization (P) analysis. The results are shown in Figure 3B. The P-value decreased in U-87MG cells treated with HL25, indicating the enhanced cell membrane fluidity. These results suggest that the increase in the membrane fluidity due to the accumulation of HL25 in the U-87MG cell membrane could be involved in the early events of HL25-induced apoptosis.
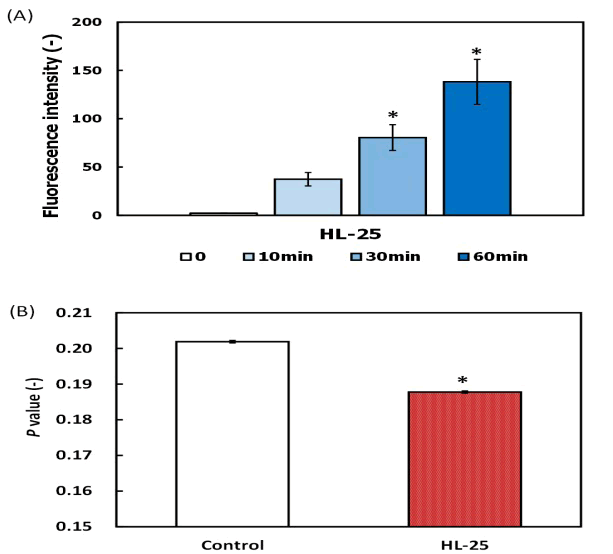
Figure 3: (A) Fusion and accumulation of HL25 (HL25/NBDPC) including fluorescence probe in the plasma membranes of U87MG cells. Data represent the mean (n=3) ± S.E. * p <0.05, vs. control and DMPC. [DMPC]=9.96 × 10-5 M, [NBDPC]=4.44×10-7 M, [C12(EO)25] = 1.11×10-5 M (B) Increase in membrane fluidity of U87MG cells after treatment with HL25. Incubation time: 24 h. * p <0.05, vs. control and DMPC. [DMPC] = 1.0 × 10-4 M, [C12(EO)25] = 1.11 × 10-5 M.
Reduction in the tumor area in the brains of orthotopic graft mouse models of glioblastoma after treatment with HL25
After the subcutaneous inoculation of U-87MG cells was completed, we examined the therapeutic effects of intravenous treatment of HL25 on tumor growth in orthotopic graft mouse models of glioblastoma. During the study, the animals were handled according to the guidelines for animal experimentation under Japanese law. This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals issued by Sojo University. The protocol was approved by the Committee on the Ethics of Animal Experiments at Sojo University. Remarkable inhibition of tumor enlargement (vs. control, p<0.05) was obtained in orthotopic graft mouse models of glioblastoma treated with HL25 based on relative brain weight (Figure 4A). Reduction in tumor growth was observed by analyzing the autopsy photographs of the tumors in the mouse models of glioblastoma treated with HL25 (Figure 4B). We investigated the accumulation of HL25 using sections of the tumors of the mouse models of glioblastoma treated with HL25, including NBDPC (Figure 4C). The accumulation of HL25, including NBDPC (green color), was detected among the tumor cells of the brain tissue sections obtained from model mice treated with HL25. These results indicated that HL25 is remarkably effective at inhibiting the growth of U-87MG cells and can cross the Blood-Brain Barrier (BBB) in orthotopic graft mouse models of glioblastoma.
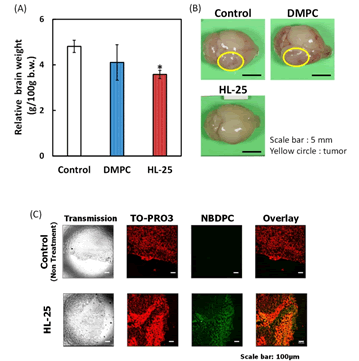
Figure 4: (A) Relative brain weight of orthotopic graft model mice treated with HL25 after inoculation with U87MG cells in the right brain area. The values represent the mean ± S.E. *p<0.05 (vs. control, DMPC) (B) Photographs of the cecum in the orthotopic graft model mice treated with HL25 after inoculation of U87MG cells to the right brain area. Circle: Tumor. Scale bar: 1 cm (C) Accumulation of HL25 encapsulating fluorescence probe after crossing the blood-brain barrier to the tumors in the orthotopic graft model mice 4 weeks after inoculation with U87MG cells. Scale bar: 1 cm.
Conclusion
We have established, for the first time that hybrid liposomes (HL25) have a therapeutic effect in an orthotopic graft mouse model of human glioblastoma (U87MG) cells.
The noteworthy findings are as follows: (a) HL25 with a hydrodynamic diameter less than 100 nm persisted for 4 weeks. (b) The inhibitory effect of HL25 on the growth of U87MG cells was observed, and it was driven by increased apoptosis. (c) HL25 induced apoptosis in U87MG cells via the release of AIF, a caspase-independent pathway. (d) HL25 fused and accumulated in U87MG cell membranes, increasing their fluidity. (e) HL25 also inhibited tumor enlargement of orthotopic graft mouse models of glioblastoma after crossing the blood-brain barrier. The results of this study could be potentially advantageous for future clinical applications of HL25 therapy in patients with glioblastoma.
Acknowledgments
We thank Aya Yamashita for her technical assistance. This work was supported in part by a Grant-in-Aid for Science Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (No. 20K05239).
REFERENCES
- Committee of Brain Tumor Registry of Japan. Report of brain tumor registry of Japan (1969-1996) (11th edn), Neurol Med Chir, Tokyo, Japan, 2003.
- Ueoka R, Matsumoto Y, Moss RA, Swarup S, Sugii A, Harada K, et al. Membrane matrix for hydrolysis of amino acid esters with marked enantioselectivity. J Am Chem Soc. 1988;110(5):1588-1595.
- Matsumoto Y, Kato T, Iseki S, Suzuki H, Nakano K, Iwahara M, et al. Remarkably enhanced inhibitory effects of hybrid liposomes on the growth of specific tumor cells. Bioorg Med Chem Lett. 1999;9(14):1937-1940.
- Matsumoto Y, Iwamoto Y, Matsushita T, Ueoka R. Novel mechanism of hybrid liposomes-induced apoptosis in human tumor cells. Int J Cancer. 2005;115(3):377-382.
- Iwamoto Y, Matsumoto Y, Ueoka R. Induction of apoptosis of human lung carcinoma cells by hybrid liposomes containing polyoxyethylenedodecyl ether. Int J Pharm. 2005;292(2):231-239.
- Nagami H, Nakano K, Ichihara H, Matsumoto Y, Ueoka R. Two methylene groups in phospholipids distinguish between apoptosis and necrosis for tumor cells. Bioorg Med Chem Lett. 2006;16(4):782-785
- Komizu Y, Matsumoto Y, Ueoka R. Membrane targeted chemotherapy with hybrid liposomes for colon tumor cells leading to apoptosis. Bioorg Med Chem Lett. 2006;16(23):6131-6134.
- Kitajima H, Komizu Y, Ichihara H, Goto K, Ueoka R. Hybrid liposomes inhibit tumor growth and lung metastasis of murine osteosarcoma cells. Cancer Med. 2003;2(3):267-276.
- Ichihara H, Ueno J, Umebayashi M, Matsumoto Y, Ueoka R. Chemotherapy with hybrid liposomes for acute lymphatic leukemia leading to apoptosis in vivo. Int J Pharm. 2011;406(1): 173-178
- Ichihara H, Hino M, Umebayashi M, Matsumoto Y, Ueoka R. Intravenous injection of hybrid liposomes suppresses the liver metastases in xenograft mouse models of colorectal cancer in vivo. Eur J Med Chem. 2012;57(11):143-148.
- Ichihara H, Okumura M, Matsumoto Y. Theranostics with hybrid liposomes in an orthotopic graft model mice of breast cancer. Anticancer Res. 2018;38(10):5645-5654.
- Ichihara H, Nagami H, Kiyokawa T, Matsumoto Y, Ueoka R. Chemotherapy using hybrid liposomes along with induction of apoptosis. Anticancer Res. 2008;28(2):1187-1196.
- Ueoka R, Matsumoto Y, Goto K, Ichihara H, Komizu Y. Membrane targeted chemotherapy with hybrid liposomes for tumor cells leading to apoptosis. Curr Pharm Des. 2011;17(17):1709-1719.
- Tominaga H, M Ishiyama F, Ohseto K, Sasamoto T, Hamamoto K, Suzuki et al. A water-soluble tetrazolium salt useful for colorimetric cell viability assay. Anal Commun. 1999;36():47-50
- Telford WG, Komoriya A, Packard BZ. Detection of localized caspase activity in early apoptotic cells by laser scanning cytometry. Cytometry. 2002;47(2):81-88.
- Ono A, Hattori S, Kariya R, Iwanaga S, Taura M, Harada H, et al. Comparative study of human hematopoietic cell engraftment into Balb/c and C57BL/6 strain of Rag-2/Jak3 double-deficient mice. J Biomed Biotechnol. 2011;2011(1):539748.
- Allen TH, Hansen C, Martin F, Redemann C, Yau-Young A. Liposomes containing synthetic lipid derivatives of poly(ethylene glycol) show prolonged circulation half-lives in vivo. Biochim Biophys Acta. 1991;1066(1):29-36.
Citation: Kuwabara K, Ichihara H, Matsumoto Y (2021) Novel Therapy with Hybrid Liposomes for Orthotopic Graft Mouse Models of Glioblastoma J Carcinog Mutagen. 12: 360.
Copyright: ©2021 Kuwabara K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


