Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Scientific Indexing Services (SIS)
- Euro Pub
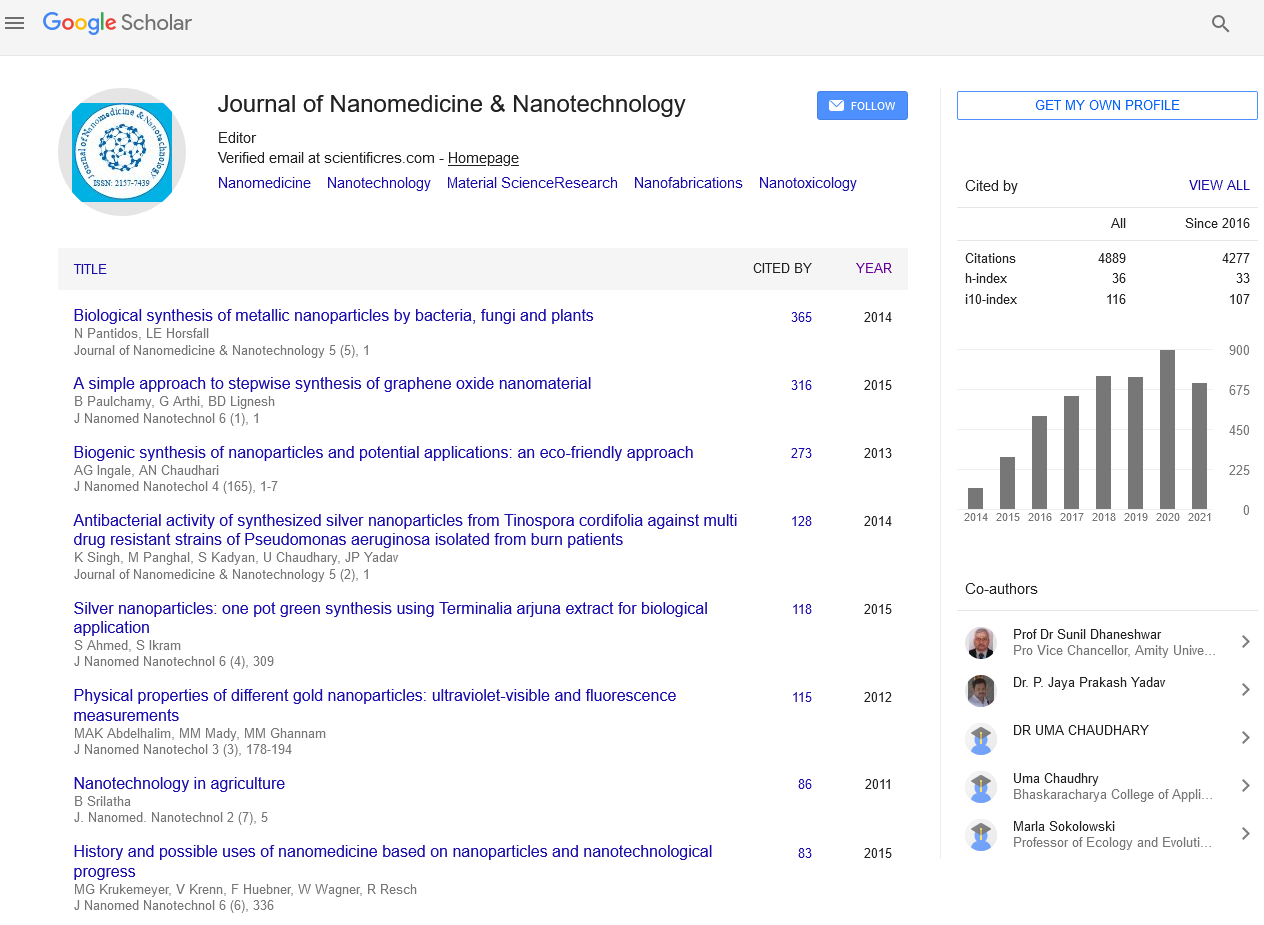
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 14, Issue 1
Nanotechnology based Targeted Delivery of Drugs: Cancer Therapy
Silva Luis*Received: 03-Jan-2023, Manuscript No. Jnmnt-23-19579; Editor assigned: 05-Jan-2023, Pre QC No. Jnmnt-23-19579; Reviewed: 18-Jan-2023, QC No. Jnmnt-23-19579; Revised: 25-Jan-2023 Published: 31-Jan-2023, DOI: 10.35248/2157-7439.23.14.656.
Abstract
Several scientific breakthrough and inventions that could militate against uncountable barriers normally experienced in traditional drugs delivery system are utilized as therapeutic candidate for the management of cancer diseases. 66It has been observed that conventional chemotherapeutics are associated with several side effects and high level of toxicity, entailing impairment of the immune system as well as having numerous detrimental effects on organ with quick penetrating cells that might be linked to the absence of solubility, nonspecific targeting, and incapability of the drug to enter the core of the tumors, which eventually lead to compromised treatment with a decrease dose and with little subsistence rate. Nanotechnology has a very great prospect with direct impact on cancerous cells as well as higher selectively with enhanced cellular uptake and drug localization. Moreover, nanoparticles could be automated for accurate identification of cancerous cells permitting selective and more precise drug delivery, which could prevent interface with the healthy cells. This chapter provides detailed information on the cell identification capability of nanomaterials with the aids of special strategies that could differentiate them from the anticancer therapies. Special highlights are provided on specific nanodrugs that are highly effective for target delivery of the active constituents against numerous cancerous cells and how they could ameliorate several side effects of unadventurous therapies.
Keywords
Electrochemical sensor; Polymers Nanoparticles; Electro polymerization
INTRODUCTION
Cancer is one of the most serious fatal diseases in today’s world that kills millions of people every year. It is one of the major health concerns of the 21st century which does not have any boundary and can affect any organ of people from any place. Cancer, the uncontrolled proliferation of cells where apoptosis is greatly disappeared, requires very complex process of treatment. Because of complexity in genetic and phenotypic levels, it shows clinical diversity and therapeutic resistance. A variety of approaches are being practiced for the treatment of cancer each of which has some significant limitations and side effects [1]. Cancer treatment includes surgical removal, chemotherapy, radiation, and hormone therapy. Chemotherapy, a very common treatment, delivers anticancer drugs systemically to patients for quenching the uncontrolled proliferation of cancerous cells. Unfortunately, due to nonspecific targeting by anticancer agents, many side effects occur and poor drug delivery of those agents cannot bring out the desired outcome in most of the cases. Cancer drug development involves a very complex procedure which is associated with advanced polymer chemistry and electronic engineering. The main challenge of cancer therapeutics is to differentiate the cancerous cells and the normal body cells. That is why the main objective becomes engineering the drug in such a way as it can identify the cancer cells to diminish their growth and proliferation. Conventional chemotherapy fails to target the cancerous cells selectively without interacting with the normal body cells. Thus they cause serious side effects including organ damage resulting in impaired treatment with lower dose and ultimately low survival rates. Nanotechnology is the science that usually deals with the size range from a few nanometers (nm) to several hundred nm, depending on their intended use. It has been the area of interest over the last decade for developing precise drug delivery systems as it offers numerous benefits to overcome the limitations of conventional formulations. It is very promising both in cancer diagnosis and treatment since it can enter the tissues at molecular level. Cancer nanotechnology is being enthusiastically evaluated and implemented in cancer treatment indicating a major advance in detection, diagnosis, and treatment of the disease. Various researches are being carried out in order to discover more accurate nanotechnology based cancer treatment minimizing the side effects of the conventional ones [2]. Nanoparticles are now being designed to assist therapeutic agents to pass through biologic barriers, to mediate molecular interactions, and to identify molecular changes. They have larger surface area with modifiable optical, electronic, magnetic, and biologic properties compared to macroparticles. Current nanotechnology based drug delivery systems for cancer treatment, which are already marketed and under research and evaluation, include liposomes, polymeric micelles, dendrimers, nanospheres, nanocapsules, and nanotubes. Nanotechnology based formulations that have already been marketed are DOXIL (liposomal doxorubicin) and Abraxane (albumin bound paclitaxel).
METHODOLOGY
Limitations of Conventional Chemotherapy Conventional chemotherapeutic agents work by destroying rapidly dividing cells, which is the main property of neoplastic cells. This is why chemotherapy also damages normal healthy cells that divide rapidly such as cells in the bone marrow, macrophages, digestive tract, and hair follicles. The main drawback of conventional chemotherapy is that it cannot give selective action only to the cancerous cells. This results in common side effects of most chemotherapeutic agents which include myelosuppression (decreased production of white blood cells causing immunosuppression), mucositis (inflammation of the lining of the digestive tract), alopecia (hair loss), organ dysfunction, and even anemia or thrombocytopenia. These side effects sometimes impose dose reduction, treatment delay, or discontinuance of the given therapy [3]. In case of solid tumors cell division may be effectively ceased near the center, making chemotherapeutic agents insensitive to chemotherapy. Furthermore, chemotherapeutic agents often cannot penetrate and reach the core of solid tumors, failing to kill the cancerous cells. Traditional chemotherapeutic agents often get washed out from the circulation being engulfed by macrophages. Thus they remain in the circulation for a very short time and cannot interact with the cancerous cells making the chemotherapy completely ineffective. The poor solubility of the drugs is also a major problem in conventional chemotherapy making them unable to penetrate the biological membranes. Another problem is associated with Pglycoprotein, a multidrug resistance protein that is overexpressed on the surface of the cancerous cells, which prevents drug accumulation inside the tumor, acting as the efflux pump, and often mediates the development of resistance to anticancer drugs. Thus the administered drugs remain unsuccessful or cannot bring the desired output. 3. Nanotechnology in Cancer Targeting Nanotechnology has made a great revolution in selective cancer targeting. Nanoparticles can be designed through various modifications such as changing their size, shape, chemical and physical properties, and so forth, to program them for targeting the desired cells. They can target the neoplastic cells either through active or passive targeting. Cellular Uptake, pH Dependent Drug Delivery, and Prevention from Lysosomal Degradation [4].
RESULTS
Active or passive targeted nanoparticles face a major difficulty in releasing drugs in the neoplastic cells since lysosomal enzymes rapidly destroy both the nanoparticles and drugs inside the cells. After internalization, the colloidal carriers usually reach the lysosomal compartment, in which hydrolytic enzymes degrade both the carrier and its content. Therefore, the intracellular distribution of the carrier is modified when the encapsulated drug is a nucleic acid. Because pH around of tumors cells is more acidic, carriers that change solubility at lower pH can be used to target and release drugs [5]. The extracellular environment of solid tumors is acidic and there is an altered pH gradient across their cell compartments. Nanoparticles sensitive to the pH gradients are promising for cancer drug delivery. A pHresponsive nanoparticle consists of a shell and a core and it responds to the pH gradient and changes its solubility pattern. The core-shell polymer nanoparticles are designed with their lower critical solution temperature being dependent on the ambient pH 7.4. At low pH, in and around of tumor cells the resulting change in LCST causes the coreshell nanoparticles to deform and precipitate in an acidic environment, triggering the release the chemotherapeutics. A targeting molecule is additionally conjugated to the shell of the nanoparticles which can recognize tumor cells [6].
Shefer and his team reported a new strategy for preparing a pH sensitive sustained release system for cancer treatment. The system utilizes solid hydrophobic nanospheres containing anticancer drugs that are encapsulated in a pH sensitive microsphere. It additionally included a bio adhesive material into the solid hydrophobic matrix of the nanospheres. The nanospheres hydrophobic matrix was formed by dispersing paclitaxel into the hot melt of candelilla wax. The microsphere of pH sensitive matrix was created by adding the drug wax mixture into an aqueous solution containing a pH dependent anionic polymer which is stable at pH 7.4 but solubilized at pH 6 and lower. The prepared suspension was spray dried to produce a free flowing dry powder which consists of 10% paclitaxel [7]. The nanospheres can release the drug over an extended period of time by dissolving swelling the microsphere at a lower pH that is typically found in cancerous tissue. Recently, researchers developed a system that either fuse with the plasma membrane or have a pHsensitive configuration that changes conformation in the lysosomes and allows the encapsulated material to escape into the cytoplasm. Biodegradable nanoparticles were formulated from the copolymers of poly for their rapid endolysosomal escape. The system worked by selective reversal of the surface charge of nanoparticles in the acidic endo lysosomal compartment causing the nanoparticles to interact with the endo lysosomal membrane and escape into the cytosol. These nanoparticles can deliver wide ranged therapeutic agents, including macromolecules such as DNA at a slow rate, for sustained therapeutic effect. For using nanotechnology in cancer treatment, researchers developed thermoresponsive, pH-responsive, and biodegradable nanoparticles by grafting biodegradable poly onto N-isopropyl acrylamide and methacrylic acid. It may be sufficient for a carrier system to concentrate the drug in the target tissue.
DISCUSSION
Hyperthermia Healthy cells are capable of surviving exposure to temperatures up to 46.5°C. Irreversible cell damage occurs to the cancerous cells at temperatures from approximately 40°C to about 46°C due to the disorganized and compact vascular structure for which they are less stable. On the other hand, surrounding healthy cells are more readily able to spatter heat and maintain a normal temperature. This process stated above is called hyperthermia which is used for the purpose of damaging protein and structures within cancerous cells and in some cases, causing tumor cells to directly undergo apoptosis [8]. Nanoparticles are utilized for a variety of purposes in hyperthermia-based treatments which include serving as the active thermo therapeutic agents, sensitizers and are also used for targeting purposes like antibody enhanced targeting to increase efficacy and to reduce hypothermia-associated side effects. Nanoparticles can locate and specifically target the deep-seated tissues and organs. Magnetic fluid hyperthermia is a well-practiced old method for cancer treatment. Small magnetic particles are used which respond to an externally applied magnetic field by heating up. In addition to specific targeting, nanoparticles add another benefit. Cells that have picked up some of the particles cannot get rid of them, and thus every daughter cell will have one half of the amount of particles present on the mother cell. Handy et al. developed a method of manufacturing nanoparticles for targeted delivery of thermotherapy in cancer treatment. The prepared ferromagnetic nanoparticles were coated with biocompatible material poly using free-radical polymerization. A stabilizing layer was formed around the magnetic particles by an ionic surfactant, sodium bis-2-ethylhexyl sulfosuccinate. For selective targeting, antibodies were covalently attached to the surface of coated magnetic particles. The thermo therapeutic magnetic composition containing singledomain magnetic particles attached to a target specific ligand was inductively heated using a magnetic field. High efficiency of the bioprobes was determined in animal model [9].
Overcoming Other Limitations of Conventional Chemotherapy Lack of solubility is one of the major limitations of most chemotherapeutic agents. Nanoparticles can effectively solve the solubility problem. Hydrophobic drugs can be encapsulated in micelles to increase their solubility. Dendrimers contain many binding sites with which both hydrophobic and hydrophilic molecules can bind. Liposomes also allow encapsulating hydrophobic drugs and transporting them to the desired area soon after administration. Several approaches have been taken to overcome Pglycoprotein mediated drug resistance. P-glycoprotein locates drugs which are localized in the plasma membrane only. One strategy is to use the inhibiting agents such as verapamil or cyclosporine when concurrently administered with a cytotoxic drug can restrain P-glycoprotein. Thus both chemotherapeutic agent and inhibiting agent are incorporated into the nanoparticles to overcome the problem associated with P-glycoprotein. A new strategy was developed for inhibition of the P-glycoprotein-mediated efflux of vincristine where vincristine-loaded lipid nanoparticles, conjugated to an anti-P-glycoprotein monoclonal antibody, showed greater cytotoxicity in resistant human myelogenous leukaemia cell lines than nontargeted particles. Developed SP1049C, a nonionic block copolymer composed of a hydrophobic core and hydrophilic tail that contains doxorubicin, which was able to circumvent P-glycoprotein mediated drug resistance in a mouse model of leukaemia and is now under clinical evaluation. In another study, folic acid, attached to polyethylene glycol derivatized distearoylphosphatidylethanolamine, was used to target in vitro doxorubicin loaded liposomes to folate receptor overexpressing tumor cells. Folate receptor mediated cell uptake of targeted liposomal doxorubicin into a multidrug resistant subline of M109-HiFR cells was clearly unaffected by P-glycoprotein-mediated drug efflux, in sharp contrast to uptake of free doxorubicin [10]. Targeting Agents Nanocarriers are used as targeting agents for cancer therapy comprising anticancer drugs, targeting moieties, and polymers. There are a variety of nanocarriers such as liposomes, dendrimers, micelles, carbon nanotubes, nanocapsules, nanospheres, and so forth. Therapeutic agents can be entrapped, covalently bound, encapsulated, or adsorbed to the nanoparticle. Liposomes are composed of lipid bilayers where the core can be either hydrophilic or hydrophobic depending on the number of lipid bilayers. Liposomes having a single lipid bilayer contain an aqueous core for encapsulating water soluble drugs, whereas other liposomes having more than a single bilayer entrap lipid soluble drugs. They are readily cleared by the macrophages and are therefore coated with inert polymers for stabilization in the physiological conditions. Liposomes are commonly coated with polyethylene glycol (PEG). In vivo study shows that liposomes coated with hyaluronan (HA) improves circulation time and enhances targeting to HA receptor-expressing tumors. Both active and passive targeting can be achieved with liposomal drug delivery. Liposomal nanoparticles can conjugate with either antibodies or ligands for selective drug delivery. They possess some advantages that they are biodegradation, nonantigenic and have a high transport rate. They can also be designed for pH sensitive drug delivery or thermotherapy. Dendrimers are branched three dimensional treelike structures with a multifunctional core. They are synthesized from either synthetic or natural elements such as amino acids, sugars, and nucleotides. Dendrimers can be prepared by controlled polymerization of the monomers maintaining desired shape and size. Multiple entities including both hydrophobic and hydrophilic molecules can be conjugated to dendrimers due to their exclusive branching point. They can also be loaded with drugs using the cavities in their cores through hydrophobic interactions, hydrogen bonds, or chemical linkages. Dendrimers are capable of delivering genes, drugs, anticancer agents, and so forth. Micelles are spherical structures where molecules with a hydrophobic end aggregate to form the central core and the hydrophilic ends of other molecules are in contact with the liquid environment surrounding the core. Micelles are effective carrier for the delivery of water insoluble drugs carried in the hydrophobic core. Nanospheres are spherical in shape that is composed of a matrix system in which drug is evenly distributed by entrapment, attachment, or encapsulation.
CONCLUSION
The surface of these nanoparticles can be modified by the addition of ligands or antibodies for targeting purposes. On the other hand, nanocapsules are like vesicles that have a central core where a drug is confined and a core is surrounded by a polymeric membrane. Targeting ligands or antibodies can be attached to the surface. Fullerenes (also called bucky balls) and nanotubes are a family of molecules composed of carbon in the form of a hollow sphere or ellipsoid tube. Atoms may be trapped inside fullerenes while antibodies or ligands are bound to the surface for targeting. Carbon nanotubes are modified to make them watersoluble and functionalized as they can be linked to a variety of active molecules such as peptides, proteins, nucleic acids, and therapeutic agents. Nanotubes can be single walled or multiwalled. Suitable polymers for nanoparticle preparation include poly (alkyl cyanoacrylates), poly (methylidenemalonate), and polyesters such as poly (lactic acid), poly (glycolic acid), poly (e-caprolactone), and their copolymers. Poly, poly lactic acid (PLA), poly glycolic acid (PGA), and their copolymers are most extensively researched due to their biocompatibility and biodegradability. Illustrates some polymer based formulations that brought out positive results in recent research. 9. Conclusion Nanotechnology has already revolutionized cancer therapy in many aspects and is radically changing the treatment pattern. It has made a great impact on selective recognizing of the cancerous cells, targeted drug delivery, and overcoming limitations of the conventional chemotherapies. Some nanotechnology based formulations have already been launched in the market and many are undergoing research and clinical trials. The side effects of the traditional chemotherapies can greatly be removed by these novel active or passive targeting which can substantially increase the survival rate. As cancer is one of the most serious lethal diseases, the contribution of nanotechnology in precise treatment avoiding the life threatening side effects can potentially contribute to a positive movement in clinical practice for life saving approach.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interests regarding the publication of this paper.
REFERENCES
- Niinomi M, Nakai M. Titanium-based biomaterials for preventing stress shielding between implant devices and bone. Int J Biomater. 2011; 2011(1): 836587.
- Donnelly RF, Raj Singh TR, Woolfson AD. Microneedle-based drug delivery systems: Microfabrication, drug delivery, and safety. Drug Delivery. 2010; 17(4): 187-207.
- Sharma D. Microneedles: An Approach in Transdermal Drug Delivery: A Review. Pharmatutor. 2018; 6(1): 07.
- Hopcroft MA, Nix WD, Kenny TW. What is the Young’s modulus of silicon. J Microele Systems. 2010; 19(2):229–238.
- Mcallister D v, Wang PM, Davis SP, Park JH, Canatella PJ, Allen MG, et al. Microfabricated needles for transdermal delivery of macromolecules and nanoparticles: Fabrication methods and transport studies. Proc Natl Acad Sci. 2003; 100(24): 13755-13760.
- Gupta J, Felner EI, Prausnitz MR. Minimally Invasive Insulin Delivery in Subjects with Type 1 Diabetes Using Hollow Microneedles. Diabetes Technol Ther.2009; 11(6): 329-337.
- Williams AC, Barry BW. Penetration enhancers. Adv Drug Deliv Rev. 2004; 56(5): 603–618.
- Gittard SD, Narayan RJ, Jin C, Ovsianikov A, Chichkov BN, Monteiro-Riviere NA, et al. Pulsed laser deposition of antimicrobial silver coating on Ormocer microneedles. Biofabrication. 2009;1(4): 041001.
- Li J, Liu B, Zhou Y, Chen Z, Jiang L, Yuan W, et al. Fabrication of a Ti porous microneedle array by metal injection molding for transdermal drug delivery. PLoS ONE. 2017; 12(2): e0172043.
- Verbaan FJ, Bal SM, van den Berg DJ, Groenink WHH, Verpoorten H, Lüttge R, et al. Assembled microneedle arrays enhance the transport of compounds varying over a large range of molecular weight across human dermatomed skin. J Control Release. 2007; 117(2): 238–245.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Luis S (2023) Nanotechnology Based Targeted Delivery of Drugs: Cancer Therapy. J Nanomed Nanotech. 14: 656.
Copyright: ©2023 Luís S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.