Citations : 2345
Dentistry received 2345 citations as per Google Scholar report
Indexed In
- Genamics JournalSeek
- JournalTOCs
- CiteFactor
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2020) Volume 10, Issue 7
Low Level Laser Therapy: Its Expanded Tentacles in Dentistry, Review
Nagy Abdulsamee Consultant Prosthodontics and Head of Dental Biomaterials1*, Ahmed Elkhadem2 and Passant Nagi22Department of Oral and Dental Medicine and Surgery, Cairo University, Egypt
Received: 04-Aug-2020 Published: 11-Sep-2020, DOI: 10.35248/2161-1122.20.10.567
Abstract
Background: The introduction of lasers and more specifically Low Level Laser Therapy (LLLT) has been historic in almost every field of dentistry. LLLT nowadays have several applications in many dental fields. The non-invasive treatment of oral diseases is an important aim of modern dentistry. Laser effects have not yet been investigated widely, however as a safer option to traditional therapy they have the ability to become known.
Objectives: In this review we aim to highlight the mechanism of action and the effects of LLLT. We also aim to highlight how different wavelengths and energy applied can have a distinct impact on the effectiveness of LLLT.
Methodology: The search for articles was carried out on the Google Scholar, PubMed, and Web of Science. The articles selected were the most recent, original ones, and that evaluated the use of LLLT in dentistry.
Conclusion: The advantages of this particular laser LLLT are multidirectional, and thus the effects became multifold. Improved knowledge and ongoing work in this direction has culminated in a better awareness of the LLLT's stimulatory, antiinflammatory and biogenerative activity, not just on soft tissue but also on hard tissue. Finally, we provide insight on its current and potential future applications.
Keywords
Low level laser therapy; Phototherapy; Teeth whitening; Biostimulation; Flourescemce; Orthodontic
Introduction
In dental patients the use of Low Level Laser Therapy (LLLT) almost exclusively involves red and near-infrared light. There is a so-called "optical window" in tissue of these wavelengths (approx. 650 nm-1100 nm), where the effective light penetration of the tissue is greatly increased. Key tissue chromophores (haemoglobin and melanin) have broad absorption bands at shorter wavelengths, tissue light dispersion at shorter wavelengths is low, and water heavily absorbs infrared light at wavelengths of: >1100 nm [1]. In contrast to a focused laser beam that concentrates photons in order to cut, ablate, or destroy tissue, LLLT is a defocused beam that does not appreciably elevate the tissue temperature and should not destroy tissue. In fact, lasers designed for LLLT are sometimes referred to as “cold lasers”. Lasers work by affecting certain elements within target tissues that absorb specific wavelengths of radiation, which are called chromophores. Soft tissue chromophores are melanin and hemoglobin. Hydroxyapatite is a chromophore of hard tissues. Water is a chromophore for both hard and soft tissues (Figure 1) [2].energy inside living tissue. The event electromagnetic energy is converted by cellular mitochondria into Adenosine Tri-Phosphate (ATP) [3]. Consequently, the induced rise in the production of ATP may indicate enhanced neuronal involvement in, e.g., tissue healing fibroblasts. Additionally, the conversion of some of the incident energy to heat would suggest an increase in local microcirculation by vasodilation [4].
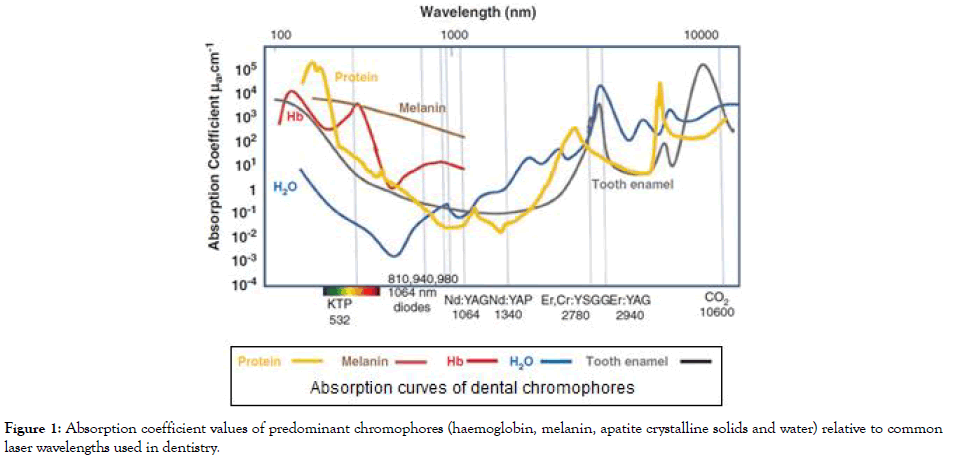
Figure 1: Absorption coefficient values of predominant chromophores (haemoglobin, melanin, apatite crystalline solids and water) relative to common laser wavelengths used in dentistry.
Physical mechanisms of LLLT
Laser photons that are delivered into living tissue can either be absorbed or scattered. The photons that are absorbed interact with an organic molecule or chromophore located within the tissue. Because these photons have wavelengths in the red or NIR regions of the spectrum, the chromophores that absorb these photons tend to have delocalized electrons in molecular orbitals that can be excited from the ground state to the first excited state by the quantum of energy delivered by the photon. According to the first law of thermodynamics, the energy delivered to the tissue must be conserved, and three possible pathways exist to account for what happens to the delivered light energy when low level laser therapy is delivered into tissue [5]. These three possible pathways are:-
First pathway (Photonic energy): A tissue/cellular chromophore consumes photonic radiation, and this elevates the chromophore 's energy status to an unstable upper stage. A chromophore is a molecule (or part of a molecule) that gives the tissue to which it is a portion a definite "color" (absorptive capacity). The chromophore's consequent first excited singlet state undergoes a transition from a higher to a lower electronic state and the energy of the electronically excited state is given off to the molecule's vibrational modes, i.e. the excitation energy is transformed into heat [6]. Hemoglobin, Cytochrome c oxidase (Cox), myoglobin, flavins, and porphyrins could be used as examples of chromophores [7].
Second pathway (Fluorescence): The second pathway that can occur is fluorescence. Fluorescence is a luminescence or reemission of light, in which the molecular absorption of a photon triggers the emission of another photon with a longer wavelength. The energy difference between the absorbed and emitted photons ends up as molecular vibrations or heat. The wavelengths involved depend on the absorbance curve and Stokes shift of the particular fluorophore [5].
Third pathway (Photochemistry): The rates of irradiation and strength of the photons concerned are inadequate to induce breakage of covalent bonds. However, the energy is sufficient to form a first excited singlet state, and this can undergo inter-system crossing to the chromophore's longer-lived triplet status. It allows for reactions, such as the conversion of energy to ground molecular oxygen to form the Reactive Singlet Oxygen (ROS) (Figure 2). Alternatively, the chromophore triplet state may undergo electron transfer (reduction) to form the radical anion which can then transfer a superoxide electron to oxygen. Stimulating the mitochondrial respiratory chain is a third photochemistry pathway that can occur after a photon is absorbed. In summary, the accumulation of photonic energy by cell mitochondria and related chromophores contributes to improvements in the biochemical system (positive and negative), signalling cells and transcription, from which instances of increased tissue regeneration and healing can be seen (Figure 2). The particular benefits of LLLT to both the central and peripheral nervous systems suggest that much wider use of LLLT could or should be made in cases of both brain diseases and nerve injuries [8].
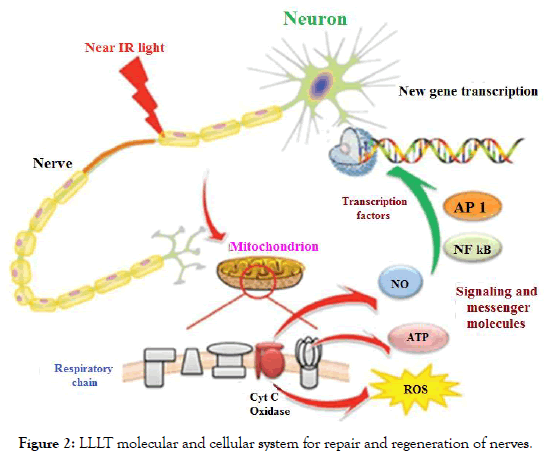
Figure 2: LLLT molecular and cellular system for repair and regeneration of nerves.
First pathway effects-photobiomodulation (Biostimulation): In order to obtain the biological result, biostimulation is the use of low-energy laser beam on the tis amounts. It is fundamentally used in wound healing and in pain reduction. The laser application providing low-dose energy is described as "low-dose laser therapy" to increase the applied tissue temperature no more than the normal body temperature (36.5°C) [9]. Photochemical theory is the most well-known hypothesis describing the mode of operation of the therapeutic lasers. The light is consumed by different molecules according to this principle and is accompanied by any of the biological chain of events. These photoreceptors on the respiratory chain are endogenous porphyrins and molecules, and increase the production of ATP [10].
Biological Effects of LLLT: The biological effects of LLLT are [8,11]:
1. Induces beta-endorphine activation and synthesis
2. Increases cortisol synthesis (cortisol is the front mol of cortisone which helps the body to combat pain or disease stress)
3. Raises output of ATP
4. Ultimately improves both DNA and protein synthesis activities
5. Neurotransmission is easy when the serotonin and acetylcholine levels increase
6. Cell replication enhances mitochondrial function
7. Modulation occurs in macrophages, fibroblasts and other cells
8. Na, Cl, and K ions regulated the cell membrane potential
9. The release of cytokines and other chemicals accelerate cell communication
10. Increase in arterial microcirculation
11. The edema reduces as venous and lymphatic movements rise
12. Inflammation reduces as leukocytes are more active in phagocytosis
13. Speedier division of cells, epithelial development and production of collagen
14. Minimal scarring and reduced formation of keloids occur
Photobiomodulation (PBM): It is the use of low intensity light sources to control cellular activites. Laser therapy (application of photonic energy at different wavelengths) operates on the concept of inducing by energy transmission a biological reaction. The photonic energy supplied to the tissue modulates biological processes within the tissue and throughout the biological framework of which the tissue is a portion. Within irradiated tissue PBM has no major thermal effect. Reported symptoms of LLLT photo-biomodulation in clinical dentistry can involve dentine hypersensitivity, post-extraction socket/post-trauma locations, drug-induced osteonecrosis/X-ray-induced osteonecrosis, orthodontic tooth movement, viral infections: herpes labialis, herpes simplex, neuropathy: trigeminal neuralgia, paraesthesia, bell's paralysis, appropriate ulceration, implant osseointegration, Tempro Mandibular Dysfunction Syndrome (TMJDS), trismus, and post-oncology: mucositis, dermatitis, post-surgery healing [12,13]. Additionally, there is evidence to support LLLT's analgesic efficacy by enhanced endorphin and bradykinin production, reduced c-fibre activity, and an altered pain tolerance. Therapeutic analgesic symptoms may also exist, by centrally releasing serotonin and acetylcholine, and peripherally releasing histamine and prostaglandins [14].
Second pathway effects-fluorescence: Fluorescent and photodynamic diagnosis can include screening services, or part of a tissue investigation hierarchy sequence. Suspect oral mucosal lesions can be exposed to biopsy and other tests. Auto-fluorescence imaging may produce good results for identifying lesions from regular mucosa, but using auto-fluorescence analysis in some other position than as an adjunctive scanning technique is inappropriate. To determine the best, most dysplastic position for biopsy, autofluorescence spectroscopy may be used wherever appropriate. The literature unfortunately indicates that auto-fluorescence is not adequately accurate for this reason [15].
The use of fluorescence in caries diagnosis was initially proposed more than a century ago, but gained greater importance with the advent of laser technologies into dental practice. Wavelengths ranging approximately 405 and 670 nm are typically used. A visual identification approach that was scientifically valid in the 1980s, based on the normal green fluorescence of tooth tissue, was developed [16]. The procedure used an argon-ion laser excitation wavelength of 488 nm to separate bright green fluorescence of good tooth tissue from carious lesions that are poorly fluoresced. In the early 1990s, the method was further evolved into what is now known as Quantitative Light-Induced Fluorescence (QLF), where the digitisation of fluorescence artifacts is used to calculate mineral damage measurements [17]. A red fluorescence method evolved at that time. Yellow fluorescence, excited either with long wavelengths of UV (350 nm-410 nm) or violet (550 nm-670 nm), was detected on the teeth in advanced caries as well as plaque and calculus.
To comparison to the lack of green fluorescence reported to caries, a strong red fluorescence in caries lesions exists between 650 nm and 800 nm and this is much brighter than that associated with sound enamel or dentine [18]. In 1998 Kavo (Kavo GmbH) developed the first commercially usable device using a red laser, with an emission wavelength of 655 nm. The aetiology of dental caries is multifactorial. Diagnosis and treatment will recognize aetiology, location of lesion and 3-D severity. Methods of identification include techniques for visual, radiographic, chemical and illuminescence, and for photodiagnostic fluoroscopy [19]. Evidence appears to show that hybrid approaches allow for better accuracy.
Laser irradiation induces differentiated tissue/caries/plaque/ calculus fluorescence in teeth. Fluorescence is a product of laser wavelength (photonic energy) [18]. Laser fluorescence may be a valuable supplement for identifying early caries in the enamel. The energy standard used in this procedure raises no patient danger and provides possible benefits [20].
Optical Coherence Tomography (OCT): OCT is a method used to produce sub-surface photographs of transparent or opaque materials at a resolution equal to a microscope with low strength. Conceptually it is analogous to an 'optical ultrasound' which provides cross-sectional images through capturing reflections from within the tissue [21]. Not all tests reliably diagnose early lesions, so there may be false positives or false negatives. It is important to identify early lesions in conjunction with an evaluation of the activity status to evaluate the prognosis and threshold needed for preventive intervention [22].
Third pathway effects-photochemistry: The therapeutic implementation of the photochemical activities triggered by the laser includes: a) tooth whitening, b) screening methods, and c) photodynamic chemotherapy of antimicrobials.
a) Tooth whitening: To counter the exponential growth in demand for tooth whitening, numerous treatment modalities have been created. Originally, the Argon 488 nm laser wavelength was developed to provide extreme photonic energy to assist in the action of hydrogen peroxide on darkened enamel and dentine, but the expense of the device coupled with the health criteria contributed to its decrease in use [23]. Many methods arose utilizing a preformed design tray device, varying from the usage of Light-Emitting Diode (LED) and plasma arc lights to home-use packages.
The current resurgence in laser-assisted tooth whitening has been the development of a Potassium Titanyl Phosphate (KTP) 532 nm laser based on diodes. This laser interacts in a photo-activated manner with bleaching gel comprising carbamide peroxide, as compared to the longer wavelengths (Diode 810 nm, CO2 10,600 nm), which work in a photothermal manner to supply heat to the gel and thus speed up the chemical reaction [24]. A red spray, comprising rhodamine B and hydrogen peroxide, is added to the tooth using the KTP laser technique and exposed to laser strength. The enzyme Rhodamine B has a median absorption of 539 nm. Once this dye is subjected to 532 nm light it consumes energy photons with resulting electron transfer to the excited singlet state. The molecule can then undergo molecular oxygen reactions, resulting in the formation of hydroxyl radicals, superoxide ions, peroxides, single labile oxygen or reactive oxygen species. In this sense, a photochemical process is the contact between the KTP laser energy and the dye [25].
In the type of thermal energy a part of the KTP laser energy consumed in the Rhodamine B dye is often passed from the excited molecule into the bleaching gel. This transition contributes to regulated gel heating and not tooth heating, reducing the risk of pulp thermal injury. The shallow heating of the gel accelerates the hydrogen peroxide degradation, thereby improving the total production of perhydroxyl radicals over a specified time span. Apart from extrinsic staining due to lifestyle causes, the administration of tetracycline antibiotics during the development of a tooth is a common cause of intrinsic staining. This staining has been shown to be immune to chemical bleaching agents that create oxidizing radicals, whereas the tetracycline molecule can be photo-oxidized with a laser of 532 nm [25].
b) Scanning and spectrometry: The creation of laser-based measurement instruments (e.g. confocal micrometer), utilizing lowenergy laser beam splitting and optical detector, allowed precise reproduction of the geometry of dental and oral structures and products used in dental restoration. In the area of orthodontics and facial growth the first application of laser scanning was to include 3D visualization and documentation of deformities preand post-treatment [26]. Scanned data was linked using Computer- Assisted Design (CAD) to the computer software. During the last decade, this concept has been extended to enable the scanning of restorative cavities prior to cast or milled indirect reconstruction and documenting of oral and facial swelling [27].
The integration of doppler laser flowmetry into dentistry applications has allowed comprehensive study of pulpal and gingival blood flow to assist in treatment planning [28,29]. An additional related application of laser light is by Raman Spectroscopy in oral medicine. A raman spectrum reflects the scattering of molecule or crystal motions of incident laser radiation. This activity is very sensitive to the molecular structure of the materials being studied, and work fields include the study of disease mechanisms such as cancer, atherosclerosis and bone disorder in vitro and in vivo. As for the above, Raman's in vivo spectroscopic study of improvements in mineral and matrix has been seen to be effective in measuring early shifts in bone tissue [30].
c) Photodynamic Antimicrobial Therapy (PDAT): The idea of the light-activated drug therapy in the context of photo-dynamic therapy is well known in medicine. Photo-activated antimicrobial chemotherapy is a technology that goes beyond the traditional usage of chemical agents to accomplish bacterial decontamination in parodontal and the restorative aspects of dentistry. Acronyms to characterize this treatment vary, and opinion has continued to follow the usage of PDAT. Currently, the most promising feature of PDAT seems to be the topical application of a photosensitizer to infected tissues and the subsequent illumination [31]. The procedure requires adding an effective chemical-a photosensitizerto the treatment site. A photosensitiser is a chemical compound that undergoes rapid photo-excitation laser irradiation and then converts the energy to other molecules. Oxygen from the host tissue, thus passing intersystems in near proximity to create oxygen radicals (O2−) and other free-radicals (H2O2 and OH−). In addition, Reactive Oxygen Species (ROS) production-electronically activated and extremely reactive oxygen state known as singlet oxygen (1O2) that can associate with a wide variety of biological substrates that trigger oxidative harm to the cell membrane and cell wall. Such damaging reactions by apoptosis or necrosis can destroy cells [32].
Throughout the dental sector, bacterial diseases are a significant cause of discomfort for practitioners [33] and, at some rates, chemical disinfectants can be carcinogenic (such as glutaraldehyde) [34]. Some of them are no longer used, accordingly. Photodynamic Antimicrobial Chemotherapy (PACT) utilizes LLLT to enable a chemical capable of generating ROS, such as H2O2 and ozone gas, which may contribute to cell death. This approach is used to remove pathogens in the root canal [35]. A variant of this is a form of PDTA employed on cariogenic biofilms. The main molecule necessary for ROS development during this step is oxygen. The approach includes generating free radicals, which may happen by one of two methods. In the first step, the photosensitizer reacts through an electron transfer with a substrate material and produces the radical species. In the second step, the photosensitizer interacts with oxygen to allow singlet oxygen (the reactive species) to form (Figure 3) [36]. This procedure was used as an alternative to the scaling and root planning as a parodontal operation.
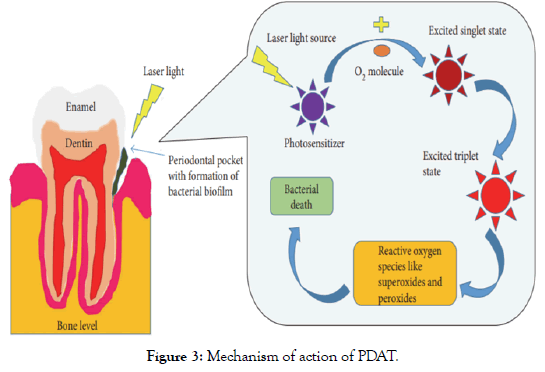
Figure 3: Mechanism of action of PDAT.
Several photo-sensitizers were used to analyze PDAT. Each photosensitiser has a specific absorption peak equal to the laser wavelength added. Circumin (Yellow)-430 nm, methylene blue- 660 nm, radachlorin (chlorophyll derivative)-660 nm, toluidine blue-680 nm, and indocyanine green-810 nm are examples of commercially available dyes. And it has been shown that these induce statistically important bacteriocidal effects on a number of bacterial periopathic species [37]. The triple-state photosensitiser molecules activated by π>850 nm have inadequate energy to cause ROS in neighboring tissue O2. The peak absorption at 810 nm with indocyanine green provided the impression that its behavior is not solely photodynamic, but is primarily photothermal [38].
Work in the early 1990s , especially by Wilson and Pearson at the Eastman Dental Institute, London, established the sensitivity of Streptococcus mutans to PDT while the organism was found in a collagen matrix-an condition identical to that that might occur inside a carious tooth [39]. If bacterial contamination of the prepared cavity could be rendered sterile, the hypothesis suggested a significant reduction in the potential for recurrent caries. The principle has also been extended to include a more interceptive treatment of demineralised but otherwise intact enamel surfaces, where bacterial removal and fluoride therapy may prevent a more important carious cavity from developing [40]. Latest in vitro and in vivo experiments on the usage of Photoactivated Disinfection (PAD) in endodontics have shown this therapy 's efficacy against a variety of endodontic-associated anaerobic bacterial strains [41].
Applications of LLLT in dentistry
The production of pulp cell care includes LLLT. Studies focused on the 660 nm wavelength diode laser phototherapy indicate a positive response in the differentiation and growth of pulp stem cells, judging by their cellular mitochondrial activity. The prospect of laser-driven pulp stem cells in their differentiation provides a insight in the medical strategies for the management of dental pulp diseases [42].
LLLT will give patients therapeutic value including rapid wound healing and pain relief. The key benefit is that it is a nonsurgical technique which reduces the occurrence of oedema and inflammation. Improving wound healing, remodeling and bone reconstruction, repairing neuronal functions after damage and encouraging immune system control and nociceptive signals are the advantages of utilizing soft lasers [43]. LLLT has developed itself well in clinical dentistry due to therapeutic benefits such as bio enhancement, regenerative ability, and lower heat antiinflammatory effects. The diode laser is absorbed by the soft tissue pigmentation and has a good haemostatic agent, with a power output of 2 W to 10 W [44].
LLLT controls the inflammatory cycle in surgical third molar extractions that induces little to no side effects by minimizing pain and swelling and restoring damaged tissues as these complications are normal in all patients following removal of the third molar. There has also been a rise in randomized clinical studies focused on the impact of LLLT on various variables such as wound healing, scarring, disorders of the temporomandibular joint, dental pain and oral mucositis [45]. Anaesthesia has had a beneficial impact on minimizing the damage of arteries or nerves that may in certain instances be induced by the needle puncture. Until application, LLLT can be added directly to the superficial mucosa, providing a strong cosmetic result, but it can not be extended to the hard palate. Oedema is based on the lymphatic system, which is attributed to an intensified inflammatory response. When LLLT is added specifically to the lymph nodes, then oedema would be minimized. Widespread oedema can take large doses and frequent treatments to relieve this. Through medical lasers, discomfort is reduced as it decreases the amplitude of nerve conduction and action potentials as well as the removal of noxious stimulations [43].
LLLT was implemented with very minimal side effects particularly for treating the erosive lichen planus form. There are, however, two forms of results generated by a low-level laser: essential and auxiliary. It causes primarily vasodilation, lymphatic drainage, cellular activity and metabolism, blood flow enhancement, fibroblast and neutrophil activation, and pain threshold stimulation. The secondary result of tissue encephaline is the accumulation of prostaglandin, immunoglobulin and lymphocytes, and beta-endorphin. It would also rising bacteria, inflammation, discomfort, soreness and immune response [46]. LLLT technology has demonstrated a substantial decrease in the discomfort associated with oral mucositis, as well as a quicker healing of oral lesions [47].
A study examined the intraoral treatment of LLLT's antiinflammatory and analgesic activity. Authors of this paper reported that LLLT is a healthy successful therapy for accelerated regeneration, increased tissue remodeling, decreased pain and analgesia for use in a broad variety of oral pathologies. It is drug-free and fairly side effect-free, which tends to be beneficial when there are not many existing pharmaceuticals. In addition to a greater rate of postoperative recovery and improved tissue remodeling, LLLT is often a significant advantage for patients in distress, who are needle phobic or who can not handle Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) [48].
An in vivo study conducted to evaluate the use of LLLT in pain, discomfort, bleeding, and clot formation within the socket after removal of healthy adult patients' upper anterior teeth. Conclusion was using a 0.8 W (output power) 940 nm diode laser in continuous mode as LLLT has a major impact on pain relief, irritation, and bleeding rates with the creation of a healthy blood clot within the tooth socket [49].
An article provided insight to the use of LLLT in the area of endodontics, be it drainage, disinfection, surgical treatment, pain relief or even an unincidental and quicker healing of the wound after endodontic operation. Based on the findings of these checked papers, it is hypothesized that LLLT will improve disinfection and healing in endodontics, with apicectomies consistent with periapical bony lesions and post-surgical analgesia and healing. The mechanism of action may be through the activation and differentiation of cellular proliferation and result in rapid healing process [50].
A comprehensive analysis was carried out to determine the utility of LLLT for the clinical treatment of orofacial neuropathic pain. The results were: 1) LLLT seems to be effective as a treatment alternative for various orofacial neuropathic pain disorders, such as trigeminal neuralgia; occipital neuralgia, and burning mouth syndrome as a single or combination therapy; 2) Furthermore, further clinical trials evaluating all outcome indicators of chronic pain are required in the medium and long term; and 3) In fact, the absence of standardization of the implementation methodology needs further well-designed experiments to validate the findings of this systematic review [51].
Lasers have numerous orthodontic uses, including accelerated teeth movement, bonding and debonding techniques, discomfort relief, bone healing, etching procedures, mini-implant protection, soft tissue procedures (gingivectomy, frenectomy, immediate anchorage uncovering, and welding procedures [11]. Owing to its reparative and anti-inflammatory activity LLLT was examined in many fields of dentistry. With regard to orthodontic tooth movement, LLLT accelerates tooth movement, reduces pain, enhances bone remodeling and reduces root resorption (OIIRR) orthodontic inflammatory induced. A recent research measured the impact of LLLT on OIIRR under strong orthodontic force magnitude (50 g) in rat model, both histologically and histomorphometrically. The result of this research was that LLLT appears effective in the avoidance or elimination of orthodontic root resorption, as well as the improvement and enhancement of OIIRR healing and repair [52,53].
Contra indication
For individuals with coagulation conditions LLLT has severe contraindications as it has a strong impact on blood supply and in instances with malignancies because it promotes cell growth [43].
Safety of LLLT
Laser instruments which are used for LLLT are rated as class III or class IIIb relative to hot lasers (class IV). Usage of special glasses is recommended for eye safety [48].
Conclusion
For virtually every area of dentistry the advent of lasers and more precisely soft lasers was revolutionary. The advantages of this particular laser is multidirectional, and thus the effects became multifold. Improved knowledge and ongoing work in this direction has culminated in a better awareness of the LLLT's stimulatory, anti-inflammatory and biogenerative activity, not just on soft tissue but also on hard tissue.
The use of LLLT in maxillofacial medicine has possible effects for quicker diagnosis and faster recovery. The soft tissue laser is a stateof- the-art tool for general dental care, delivering strong esthetic effects. Lasers have added greatly to dental clinical research in the 21st century and they will be playing a very important part in the dental profession in the future. Any dentist will also understand and promote the usage of lasers as an effective and complementary option for delivering soft and hard tissue dental treatments for babies, teenagers, teens and people with specific health care requirements, including geriatric patients. At the same time, it is important to highlight the fact that the dental practitioners undergo adequate education and training to allow effective and consistent use of lasers.
Lastly but not leastly, authors are deeply believed that LLLT will widespread in dentistry in near future when more studies and researches will be published.
Conflict of Interest
The writers are not claiming any conflict of interest.
REFERENCES
- Karu TI, Afanas’eva NI. Cytochrome c oxidase as the primary photoacceptor upon laser exposure of cultured cells to visible and near IR-range light. Dokl Akad Nauk. 1995;342:693-695.
- Verma SK, Maheshwari S, Singh RK, Chaudhari PK. Laser in dentistry: An innovative tool in modern dental practice. Natl J Maxillofac Surg. 2012;3:124-132.
- Passarella S. Increase of proton electrochemical potential and ATP synthesis in rat liver mitochondria irradiated in vitro by helium-neon laser. FEBS Lett. 1984;175:95-99.
- Karu T. Photobiological fundamentals of low powered laser therapy. IEEE J Quantum Electron. 1987;23:1703-1717.
- www.mgh.harvard.edu/wellman/people/mhamblin.asp.
- Sutherland JC. Biological effects of polychromatic light. Photochem Photobiol. 2002;76:164-170.
- Karu T. Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol. 1999;B49:1-17.
- Hashmi JT, Huang YY, Osmani BZ, Sharma SK, Naeser MA, Hamblin MR. Role of low-level laser therapy in neurorehabilitation. PMR. 2010;2:S292-S305.
- Lim HM, Lew KK, Tay DK. A clinical investigation of the efficacy of low level laser therapy in reducing orthodontic post adjust¬ment pain. Am J Orthod Dentofacial Orthop. 1995;108:614-622.
- Yamaguchi M, Hayashi M, Fujita S, Yoshida T, Utsunomiya T, Yamamoto H, et al. Low-energy laser irradiation facilitates the velocity of tooth movement and the expressions of matrix metalloproteinase-9, cathepsin K, and alpha (v) beta (3) integrin in rats. Eur J Orthod. 2010;32:131-139.
- Demirsoy KK, Kurt G. Use of laser systems in orthodontics. Turk J Orthod. 2020;33:133-140.
- Kimura Y, Wilder SP, Yonaga K, Matsumoto K. Treatment of dentine hypersensitivity by laser; a review. J Clin Periodontol. 2000;27:715-721.
- Wong SF, Wilder SP. Pilot study of laser effects on oral mucositis in patients receiving chemotherapy. Cancer J. 2002;8:247-254.
- Laakso EL, Cramond T, Richardson C, Galligan JP. Plasma ACTH and β-endorphin levels in response to low level laser therapy for myofascial trigger points. Laser Ther. 1994;3:133-142.
- Cherry KD, Schwarz RA, Yang EC, Vohra IS, Badaoui H, Williams MD, et al. Autofluorescence imaging to monitor the progression of oral potentially malignant disorders. Cancer Prev Res (Phila). 2019;12:791-800.
- Brotherton RD, Bjelkhagen H, Osanlou A, Excell P. Early detection of enamel caries by the luminescence excited by visible laser light. Swed Dent J. 1982;6:1-7.
- Hibst R, Gall R. Development of a diode laser-based fluorescence detector. Caries Res. 1998;32:294.
- Lussi A, Megert B, Longbottom C, Reich E, Francescut P. Clinical performance of a laser fluorescence device for detection of occlusal caries lesions. Eur J Oral Sci. 2001;109:14-19.
- Akbari M, Ahrari F, Jafari M. Comparative evaluation of diagnodent and caries detector dye in detection of residual caries in prepared cavities. J Contemp Dent Pract. 2012;13:515-520.
- Featherstone JD. The caries balance: the basis for caries management by risk assessment. Oral Health Prev Dent. 2004;2:259-264.
- Hariri I, Sadr A. Effects of structural orientation of enamel and dentine on light attenuation and local refractive index: an optical coherence tomography study. J Dent. 2012;40:387-396.
- Zandoná AF, Zero DT. Diagnostic tools for early caries detection. J Am Dent Assoc. 2006;137:1675-1684.
- Goldstein RE. In-office bleaching: where we came from, where we are today. J Am Dent Assoc. 1997;128:11S-15S.
- Zhang C, Wang X, Kinoshita J, Zhao B, Toko T, Kimura Y, et al. Effects of KTP laser irradiation, diode laser, and LED on tooth bleaching: a comparative study. Photomed Laser Surg. 2007;25:91-95.
- Walsh LJ, Liu JY, Verheyen P. Tooth discolorations and its treatment using KTP laser-assisted tooth whitening. J Oral Laser Appl. 2004;4:7-21.
- Commer P, Bourauel C, Maier K, Jäger A. Construction and testing of a computer- based intraoral laser scanner for determining tooth positions. Med Eng Phys. 2000;22:625-635.
- Harrison JA, Nixon MA, Fright WR, Snape L. Use of hand-held laser scanning in the assessment of facial swelling: a preliminary study. Br J Oral Maxillofac Surg. 2004;42:8-17.
- Gleissner C, Kempski O, Peylo S, Glatzel JH, Willershausen B. Local gingival blood flow at healthy and inflamed sites measured by laser doppler flowmetry. J Periodontol. 2006;77:1762-1771.
- Strobl H, Moschen I, Emshoff I, Emshoff R. Effect of luxation type on pulpal blood flow measurements: a long-term follow-up of luxated permanent maxillary incisors. J Oral Rehabil. 2005;32:260-265.
- Tarnowski CP, Ignelzi MA, Wang W, Taboas JM, Goldstein SA, Morris MD. Earliest mineral and matrix changes in force-induced musculoskeletal disease as revealed by Raman microspectroscopic imaging. J Bone Miner Res. 2004;19:64-71.
- Maisch T. A new strategy to destroy antibiotic resistant microorganisms: antimicrobial photodynamic treatment. Mini Rev Med Chem. 2009;9:974-983.
- Rajesh S, Koshi E, Philip K, Mohan A. Antimicrobial photodynamic therapy: an overview. J Indian Soc Periodontol. 2011;15:323-327.
- Laheij AM, Kistler JO, Belibasakis GN, Välimaa H, de Soet JJ. Healthcare-associated viral and bacterial infections in dentistry. J Oral Microbiol. 2012;4:1-10.
- Miyachi T, Tsutsui T. Ability of 13 chemical agents used in dental practice to induce sister-chromatid exchanges in Syrian hamster embryo cells. Odontol. 2005;93:24-29.
- Singh H, Khurana H, Singh H, Singh M. Photodynamic therapy: truly a marriage between a drug and a light. Muller J Med Sci Res. 2014;5:48-55.
- Diogo P, Goncalves T, Palma P, Santos JM. Photodynamic antimicrobial chemotherapy for root canal system asepsis: a narrative literature review. Int J Dent. 2015;2015:269205.
- Eick S, Markauskaite G. Effect of photoactivated disinfection with a light-emitting diode on bacterial species and biofilms associated with periodontitis and peri-implantitis. Photodiagnosis Photodyn Ther. 2013;10:156-167.
- Hopp M, Biffar R. Photodynamic therapies-blue versus green. Laser. 2013;1:1-25.
- Williams JA, Pearson GJ, Colles MJ, Wilson M. The photo-activated antibacterial action of toluidine blue O in a collagen matrix and in carious dentine. Caries Res. 2004;38:530-536.
- Vlacic J, Meyers IA, Walsh LJ. Combined CPP-ACP and Photoactivated Disinfection (PAD) therapy in arresting root surface caries: a case report. Br Dent J. 2007;204:457-459.
- Bonsor SJ, Nichol R, Reid TM, Pearson GJ. Microbiological evaluation of photo-activated disinfection in endodontics (an in vivo study). Br Dent J. 2006;200:337-341.
- Eduardo FP, Bueno DF, de Freitas PM, Marques MM, Passos BMR, Eduardo CP, et al. Stem cell proliferation under low intensity laser irradiation: a preliminary study. Lasers Surg Med. 2008;40:433-438.
- https://www.elsevier.com/books/principles-and-practice-of-laser-dentistry/convissar/978-0-323-29762-2.
- Mishra BM, Mishra S. Lasers and its clinical applications in dentistry. Int J Dent Clin. 2011;3:35-38.
- Oliveira SS, Melo DA, Mesquita FRA, Maia AP, Bussadori SK, Santos FKP. Effect of low level laser therapy on the post-surgical inflammatory process after third molar removal. Trials. 2013;14:373-380.
- Mahdavi O, Boostani N, Jajarm HH, Falaki F, Tabesh A. Use of low level laser therapy of oral lichen planus. J Dent (Shiraz). 2013;14:201-204.
- Cauwels RG, Martens LC. Low level laser therapy in oral mucositis: a pilot study. Eur Arch Paediatr Dent. 2011;12:34-78.
- Elson N, Foran D. Low level laser therapy in modern dentistry. Periodon Prosthodon. 2015;1:1-6.
- Hamzah BF, Ibraheem NS. The effect of low-level laser therapy after simple tooth extraction. J Int Oral Health. 2019;11:181-186.
- Kapasi A, Kapasi F. When less is more-an update on low level laser therapy applications in endodontics for predictable outcomes-a review article. Acta Scientific Dent Sci. 2019;3:83-93.
- de Pedro M, López PRM, de la Hoz AJL, Casañas E, Hernández G. Efficacy of low-level laser therapy for the therapeutic management of neuropathic orofacial pain: a systematic review. J Oral Facial Pain Headache. 2020;34:13-30.
- Yassin A, Shehata F, Al Sawa A, Karam S, et al. Effect of low-level laser therapy on orthodontic induced inflammatory root resorption in rats. Alexandria Dent J. 2020;45:62-67.
- Luke AM, Mathew S, Altawash MM, Madan BM. Lasers: a review with their applications in oral medicine. J Lasers Med Sci. 2019;10:324-329.
Citation: Abdulsamee N, Elkhadem A, Nagi P (2020) Low Level Laser Therapy: Its Expanded Tentacles in Dentistry, Review. Dentistry 10: 567. doi: 10.35248/2161-1122.20.10.567
Copyright: © 2020 Abdulsamee N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : Nil

