Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- The Global Impact Factor (GIF)
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
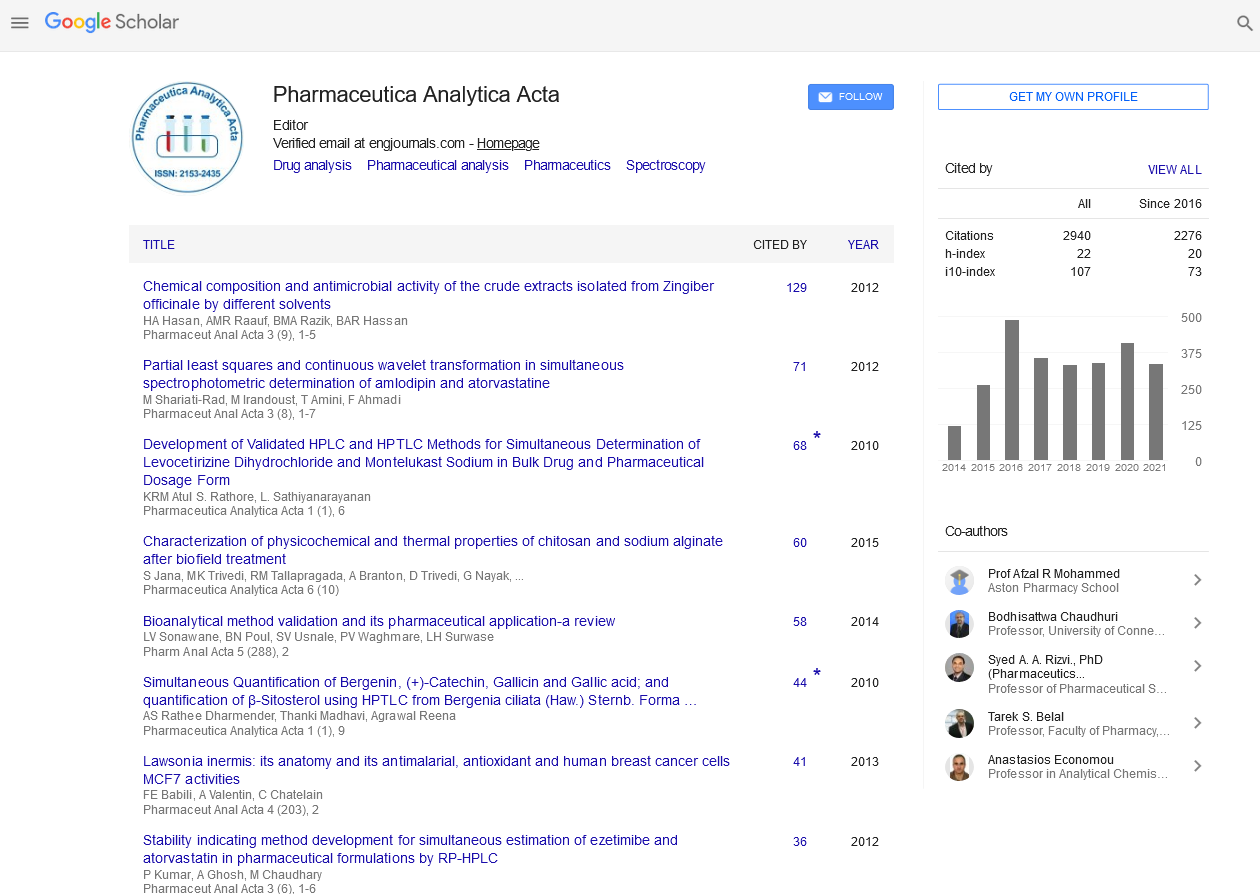
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2025) Volume 16, Issue 3
Liposomal Antineoplastic Drugs: Enhancing Efficacy and Safety in Cancer Treatment
Ralf Dieter*Received: 16-Feb-2024, Manuscript No. PAA-24-24917; Editor assigned: 21-Feb-2024, Pre QC No. PAA-24-24917 (PQ); Reviewed: 06-Mar-2024, QC No. PAA-24-24917; Revised: 04-Jun-2025, Manuscript No. PAA-24-24917 (R); Published: 11-Jun-2025, DOI: 10.35248/2153-2435.25.16.817
Description
The innovative approaches to cancer therapy, liposomal formulations of antineoplastic drugs have emerged as potential candidates for delivering chemotherapy agents to tumor sites with enhanced precision and reduced side effects. Liposomal antineoplastic drugs are encapsulated within lipid-based vesicles known as liposomes, which serve as carriers for delivering chemotherapy agents to cancer cells. These liposomes are composed of phospholipid bilayers that closely resemble the structure of cell membranes, allowing them to interact with biological membranes and facilitate drug delivery to target tissues.The encapsulation of antineoplastic drugs within liposomes offers several advantages over conventional chemotherapy formulations. Firstly, liposomal carriers can improve the solubility and stability of hydrophobic drugs, enhancing their pharmacokinetics and bioavailability in vivo. Additionally, liposomes can passively accumulate in tumor tissues through the Enhanced Permeability and Retention (EPR) effect, thereby increasing drug concentrations at the site of action while minimizing exposure to healthy tissues.
The mechanisms of action of liposomal antineoplastic drugs are multifaceted and depend on various factors, including the specific drug encapsulated, the tumor microenvironment, and the characteristics of the liposomal carrier. Generally, liposomes deliver antineoplastic drugs to cancer cells through endocytosis or membrane fusion, allowing for the intracellular release of the drug payload.
Once inside the cancer cells, the encapsulated antineoplastic drugs exert their cytotoxic effects through diverse mechanisms, including inhibition of DNA replication, interference with cell cycle progression, disruption of microtubule dynamics, and induction of apoptosis. Importantly, liposomal formulations can enhance the intratumoral concentration of chemotherapy agents while reducing their systemic exposure, thereby minimizing offtarget effects and improving therapeutic efficacy.
Liposomal antineoplastic drugs offer several therapeutic benefits that distinguish them from conventional chemotherapy regimens. Firstly, the targeted delivery of chemotherapy agents to tumor tissues enables higher drug concentrations to be achieved at the site of action, leading to increased tumor cell kill and improved treatment outcomes. Moreover, the reduced systemic exposure to antineoplastic drugs can mitigate systemic toxicity and adverse effects, enhancing patient tolerability and quality of life during cancer treatment.
Furthermore, liposomal formulations can overcome multidrug resistance mechanisms commonly observed in cancer cells, thereby restoring sensitivity to chemotherapy agents and improving treatment response rates. Additionally, the prolonged circulation time of liposomal carriers in the bloodstream allows for sustained drug release and enhanced tumor penetration, further augmenting their therapeutic efficacy against solid tumors and metastatic lesions.
Liposomal antineoplastic drugs have been extensively investigated across a wide range of cancer types and clinical settings. In oncology, liposomal formulations have shown potential for the treatment of various malignancies, including breast cancer, ovarian cancer, lung cancer, pancreatic cancer, and lymphoma. Examples of liposomal antineoplastic drugs that have received regulatory approval or are in advanced stages of clinical development include liposomal doxorubicin, liposomal paclitaxel, liposomal irinotecan, and liposomal cytarabine.
Moreover, liposomal antineoplastic drugs have demonstrated efficacy as monotherapy or in combination with other chemotherapy agents, targeted therapies, immunotherapies, and radiation therapy. The versatility of liposomal formulations allows for altered treatment regimens that can be adapted to individual patient profiles, tumor characteristics, and treatment goals.
Despite the significant progress in liposomal antineoplastic drug development, several challenges remain to be addressed to further optimize their therapeutic potential. These include issues related to drug loading efficiency, stability, scalability, manufacturing complexity, and regulatory approval. Additionally, strategies to improve tumor targeting, drug release kinetics, and resistance modulation are areas of active investigation in liposomal research.
Future directions in liposomal antineoplastic drug development may involve the integration of advanced drug delivery technologies, such as stimuli-responsive liposomes, targeted ligand-conjugated liposomes, and combination therapy approaches. Furthermore, the advent of personalized medicine and precision oncology holds potential for altering liposomal treatments to individual patient characteristics, including genetic profiles, tumor biomarkers, and treatment responses.
Conclusion
In conclusion, liposomal antineoplastic drugs represent a potential approach to cancer therapy, offering enhanced efficacy, reduced toxicity, and improved patient outcomes. By harnessing the unique properties of liposomal carriers, these innovative formulations enable targeted delivery of chemotherapy agents to tumor tissues while sparing healthy cells from cytotoxic effects. As research efforts continue to resolve the complexities of liposomal drug delivery and address existing challenges, the future holds immense potential for leveraging liposomal therapies as powerful tools in the fight against cancer.Citation: Dieter R (2025) Liposomal Antineoplastic Drugs: Enhancing Efficacy and Safety in Cancer Treatment. Pharm Anal Acta. 16:817.
Copyright: © 2025 Dieter R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.