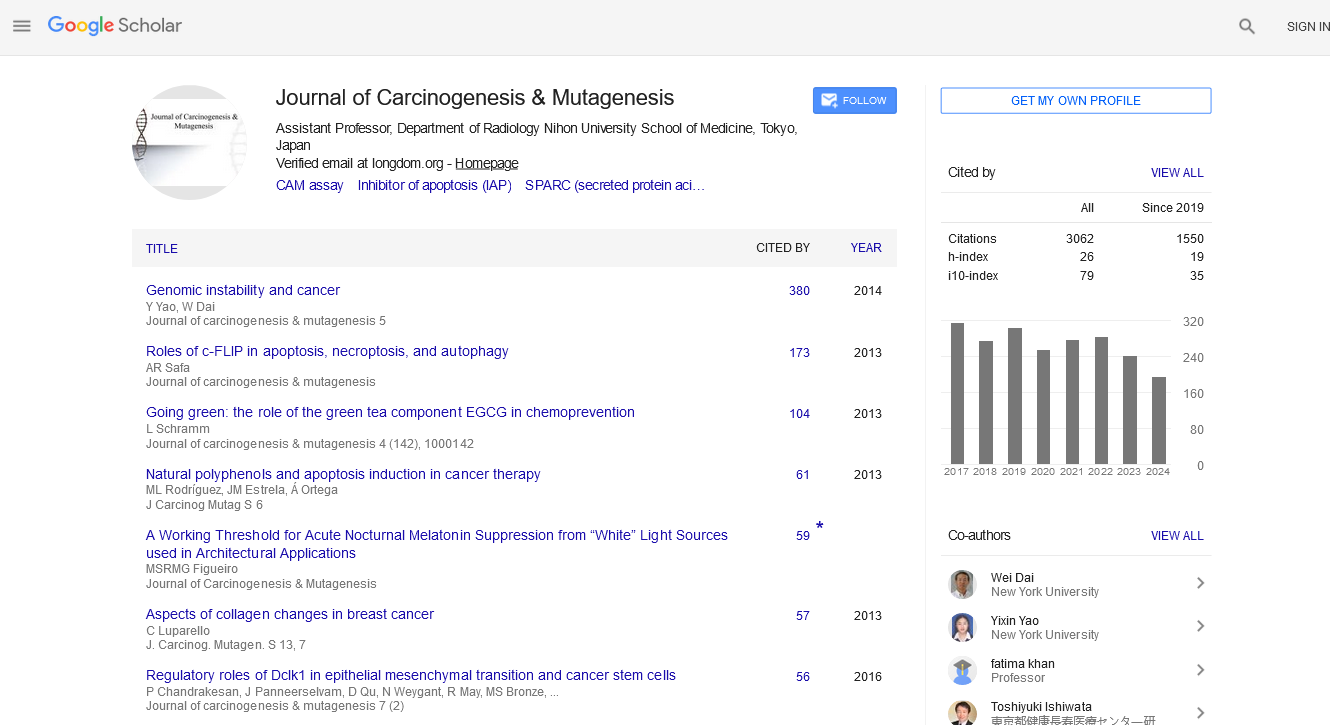
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2020) Volume 11, Issue 4
Helicobacter pylori Infection, DNA Methylation, and Gastric Carcinogenesis
Ya-Bin Qi, Ruo-Bing Hu, Song-Ze Ding*, Muhammad Noman Khan, Lei Lei, Pei-Ru Wei and Bai-Ling JiaReceived: 01-Jul-2020 Published: 22-Jul-2020, DOI: 10.35248/2157-2518.20.11.352
Abstract
Helicobacter pylori (H. pylori), the major cause of chronic gastritis, peptic ulcers and gastric cancer, infects about 50% of the world population. Although various host and bacterial factors have been suggested, the detailed pathogenic mechanisms remain to be defined. Increasing evidences have demonstrated that epigenetic dysregulation, such as DNA methylation, plays a critical role in gastric carcinogenesis, and is currently under intensive investigation. H. pylori infection result in aberrant DNA methylation in a number of gene promoters in gastric mucosa, eradication of H. pylori can reverse some hypermethylated genes, but had no effect on others. In some methylated genes, the methylation levels persist even after H. pylori eradication, and the fact suggests that DNA methylation accumulation is associated with molecular irreversibleness and gastric diseases progression. DNA methylome and gastric cancer risk analysis indicate that certain gene promoter methylation may serve as potential biomarkers for gastric cancer predication. In addition, H. pylori cagA and vacA s1m1 genotype are independent variables that is associated with higher methylation level. The levels of methylation can be influenced by the degree and length of infection exposure, and certain host gene polymorphisms are also associated with gene methylation in H. pylori-infected subjects. Continued investigation in these areas will be critical to provide insights into the molecular mechanisms of H. pylori induced gastric diseases and develop strategies for disease prevention and intervention. We review recent progress and discuss future research directions in this important area.
Keywords
Helicobacter pylori; DNA methylation; Gastrointestinal disease; Gastric cancer
Introduction
Helicobacter pylori (H. pylori), a very common gram negative bacterium, colonized in mucus layer of human stomach, is the major cause of chronic gastritis, peptic ulcers and gastric cancer. H. pylori infects approximately 50% of world population, and is also closely associated with a number of extra-gastrointestinal diseases: such as iron deficiency anemia, idiopathic thrombocytopenic purpura, vitamin B12 deficiency, autoimmunity diseases, cerebrovascular diseases, etc. [1,2]. The cancer statistics of 2018 has indicated that gastric cancer is the fifth most frequently diagnosed cancer and the third leading cause of cancer death worldwide [3].
H. pylori possesses a number of virulent factors, such as cytotoxin associate gene A (CagA), vacuolating cytotoxin A (VacA), outer inflammatory protein (OipA), outer membrane protein (OMP), and duodenal ulcer-promoting factor (DupA) etc. [4-6]. Up on infection, H. pylori attaches to gastric epithelial cells and triggers numerous cellular, inflammatory, and oncogenic signalings. These activated host cellular signaling pathways include AP-1, NF-κB, TGF-β, Wnt, Stat3, p53 pathways etc. H. pylori infection also result in either genetic or epigenetic alternations in various types of cells, such as epithelial cells, fibroblasts, immune cells, stem cells through their interacting microenvironment, and cause dysregulation of important cellular events, such as cell proliferation, apoptosis, cell movement, migration, impairment of DNA repair mechanisms and ultimately oncogenic transformation. Despite intensive investigation, it remains to be defined on how and why long term H. pylori infection will lead to the development of precancerous conditions and gastric cancer [4-6].
H. pylori Virulent Factors And Gastric Cancer
H. pylori has a smaller genome, and it has been sequenced several times, the genome of recently sequenced strain B128 7.13 consists of one circular chromosome (1.67 Mbp), one plasmid (6.149 kb), and its chromosome contains 1584 identified open reading frames [7]. H. pylori cagPAI is a 40 kb region in its genome, contains 31 open reading frames and encodes type IV secretion system (TFSS), cagA gene is localized in the -3’end of the island and encodes a 120-145 kDa CagA protein. H. pylori strains that carry cag PAI with CagA-,VacA-positive cause severe clinical gastric inflammation, which predispose to either tissue damage or neoplastic transformation, which are high-risk strains of gastric cancer, and the role of CagA protein is critical in these processes [6,8-10].
CagA protein is delivered into gastric epithelial cells via TFSS, and once inside the cell, CagA undergoes tyrosine phosphorylation at the Glu-Pro-Ile-Tyr-Ala (EPIYA) motifs, it then acts as a non-physiological scaffold/hub protein by interacting with multiple host signaling molecules, most notably the pro-oncogenic phosphataseSHP2 and the polarity-regulating kinase PAR1/MARK [11]. In addition to CagA, bacteria peptidoglycan and DNA can also be delivered by TFSS into epithelial cell, and activate multiple cellular signaling as mentioned above, especially NF-κ B signaling, which contributes to the inflammatory process and oncogenic transformation [4-6]. Three layers of evidence have clearly indicated the role of CagA in gastric carcinogenesis: (1) H. pylori strains that carries mutated cagA gene do not have the tumor initiating effects in animal model [9]; (2) in vivo transgenic mice model using artificially synthesized whole sequence of cagA gene resulted in the development of gastric cancer and other gastrointestinal and hematological tumors in mice without H. pylori infection per se [8], suggesting that it has the characteristics of oncogenic protein; (3) CagA-,VacA-positive strains are the major form of H. pylori infection clinically in many areas globally, corresponding to their high prevalence in precancerous lesions and gastric cancer incidences in populationbased study [10].
Gastric cancer can generally be subdivided into intestinal and diffuse types according to Lauren classification. (1) Intestinal type of gastric cancer has a distinct ductal structure, and is commonly found in older men and manifests as a Correa cascade, including atrophic gastritis, intestinal metaplasia, dysplasia and cancer. (2) Diffuse type of gastric cancer is characterized with diffuse growth, predispose to have lymph nodes and distant metastasis, closely related to genetic inheritance, more common in young women, but both types of gastric cancer are closely related to H. pylori infection [12]. Although many factors, such as diet, high salt, chemical factors, life style, and changes in stomach flora are suggested to be involved in gastric cancer initiation and development, H. pylori infection remains the single most important pathogenic factor for gastric cancer [1,4,5].
H. Pylori- Induced DNA Methylation in Gastric Cancer
Epigenetic changes are generally categorized into four areas: DNA methylation, histone modification, chromatin remodeling and miRNAs [13]. Epigenetic dysregulation is a hallmark of cancer, and DNA methylation is the major form of epigenetic modifications in cancer cells. DNA of cancer cells is generally hypomethylated, while promoters of certain genes are hypermethylated, both of which are implicated in carcinogenesis, as this will lead to either activation of oncogenes or in activation of tumor suppressor genes [13,14]. Epigenetic aberrations induced by H. pylori infection have been recognized as a critical component of gastric carcinogenesis [15-17].
Connections of H. pylori infection, DNA methylation and gastric cancer have been noted in just recent years, many questions remain to be explored, including the effects of bacteria virulence factors such as CagA, VacA, cagPAI on DNA methylation, interaction with other epigenetic modifications, and their potential application as gastric cancer biomarker. H. pylori infection result in aberrant DNA methylation in a number of gene promoters in gastric mucosa that have been studied extensively [15-19], including cell growth-related genes p16 (INK4a), p14 (ARF) and APC; DNA-repair genes, hMLH1, BRCA1 and MGMT; cell adherence gene E-cadherin; as well as LOX, FLNC, HRASLS, HAND1, THBD and p41ARC, which are known to be methylated in gastric cancer patients [15-19]. Eradication of H. pylori lead to reduced methylation levels of several genes; but in other genes, the methylation levels persist even after H. pylori eradication, suggest that DNA methylation accumulation is associated with molecular irreversibleness and disease progression in gastric mucosa [15,20,21].
The long-term effects of H. pylori eradication on promotor CpG island hypermethylation in gastric carcinogenesis were recently evaluated. Gene methylation rate and median values of several tumor-related genesincludingp16, CDH1, and RUNX-3 were tested before and one year after H. pylori eradication. The results showed that H. pylori-infection increased DNA methylation rate over the normal control, and methylation rates decreased at p16 and CDH1 genes after bacteria eradication. In contrast, the methylation levels of RUNX-3 gene had no difference even one year after H. pylori eradication, indicating that H. pylori eradication may reverse some hypermethylated genes, but had no effects on others [21].
H. pylori infection also increases RUNX3 promoter methylation that correlated with distinct stages of gastric cancer progression. In another observation by Lu et al., gastric cancer tissues had the highest RUNX3 methylation rate (75.2%) over the atrophic gastritis (15.9%), intestinal metaplasia (36.7%), gastric adenoma (41.8%), and dysplasia (54.9%) groups [22]. The levels of RUNX3 methylation in blood samples correlated to the methylation levels observed in gastric cancer tissues. These findings support the notion that RUNX3 methylation as a risk factor for carcinogenesis during H. pylori infection, and RUNX3 methylation from blood samples might be a valuable biomarker for early gastric cancer detection.
H. pylori infection exert different effects on DNA methylation dependent on gastric disease stages changes of DNA methylation in gastric mucosa after H. pylori eradication were investigated in LOX, APC and MOS genes [23,24]. The patients were follow-up for an average of 26.0 months (range: 6 to 76 months). H. pylori eradication decreased methylation levels in LOX, but not in APC gene. In MOS gene, methylation level decreased following H. pylori eradication over the controls groups without intestinal metaplasia (IM); but not in patients with IM or in those with dysplasia or gastric cancer. This effect was also noticed in miRNAs methylation during H. pylori infection, as Watari et al., [24] noted that miR-124a-3 methylation is reduced after H. pylorieradication in non-IM patients, but not in IM mucosa. The results indicate that H. pylori eradication affects DNA methylation in disease stage and gene-specific manner.Accumulation of aberrant DNA methylation in normal tissues is associated with the risk of gastric carcinogenesis [25]. Using a Mongolian gerbil model of H. pylori-induced gastritis, the degree of infection exposure on methylation burden was analyzed in four CpG islands, including HE6 (exon 2 of Ntrk2 gene), SA9 (exon 1 of Nol4 gene), SB5 (location not identified), and SD2 (promoter of Nptx2 gene), which were previously identified as aberrantly methylated genes by H. pylori infection. The methylation levels were increased by H. pylori infection, depending upon the infection duration. DNA methylation levels decreased after H. pylori eradication, but tended to be higher in gastric mucosae with a longer infection period. DNA with dense methylation, but not in those with sparse methylation, increased depending upon the infection period. The data suggest that the level of methylation can be influenced by the degree of exposure to H. pylori infection.In addition to the promoter specific effect and intensity of infection, virulence of bacteria strains and inflammation also affect DNA methylation level. Schneider et al., in 2013 tested DNA methylation levels in gastric biopsies at promoters of EN1, PCDH10, RSPO2, ZIC1 and ZNF610 genes during H. pylori infection [26]. The results found that cagA positive samples had higher methylation level over the uninfected persons; cagAnegative H. pylori strains only induced intermediate DNA methylation. H. pylori vacA s1m1 genotype is highly associated with cagA positivity, and vacA s2m2 genotype is associated with cagA negativity, and methylation level was not related to the number of EPIYA motifs in CagA proteins. Presence of cagA and vacA s1m1 in H. pylori strain were independent variables associated with higher methylation in these genes. In addition, high levels of mononuclear cell infiltration were significantly related to methylation in PCDH10, RSPO2, and ZIC1 genes. In another study, H. pylori CagA-induced tumor suppressor gene MGMT hypermethylation was shown by upregulating DNMT1 via AKT-NFκB pathway, and MGMT promoter methylation is positively correlated with the presence of CagA in clinical specimens [27].
Gene promoter methylation also appears associated with tumor location and histological type. Alves et al., noted that in cardia tumors, p16(INK4A) showed negative immune histochemical staining; in noncardia tumors, a significant finding was HMLH1 inactivation by methylation in intestinal type of gastric cancer; while in diffuse subtype, CDKN2A inactivation by methylation was prominent [28]. Tumors with methylated COX-2 and HMLH1 genes were associated with H. pylori vacA s1 genotype, and nonmethylated tumors were associated with the presence of flaA gene. The results suggest that inactivation of these genes by methylation occurs by distinct pathways related to histological subtype and tumor location, and also depends on the H. pylori genotype. In addition, DNA methylation accumulation is even found in gastric mucosa adjacent to cancer after H. pylori eradication [20].
Using high-throughput methylation microarray technology, genome-wide methylation profiling of H. pylori and cancerassociated DNA methylome changes were analyzed. Woo et al., in 2018 found that H. pylori infection were associated with 1,924 differentially methylated positions (DMPs) and 438 differentially methylated regions (DMRs) in gastric biopsy samples, 97.3% of them (1,872 DMPs) were hypermethylated [29]. H. pylori associated DMP/Rs showed marked stability after H. pylori clearance, suggesting an “ epigeneticmemory ” . In addition, single-nucleotide polymorphism array analysis from patient peripheral blood leukocytes found that 152 DMRs were associated with cancer risk that is independent of H. pylori infection status in normal gastric mucosa; H. pylori and cancerspecific methylation signatures were minimally affected by this genetic variation. These genes therefore may contribute to the gastric carcinogenesis, and also have the potential to be biomarkers for gastric cancer detection.
DNA Methylation as a Biomarker In Gastric Cancer Predication And Disease Progression
Recent advances start to investigate whether certain gene promoter methylation might be able to serve as biomarkers for gastric cancer and disease stage predication. A variety of samples were tested including serum, plasma and gastric washes. The DNA methylation status of tissue, particularly blood, has been associated with predisposition to gastric cancer, further studies are required to validate the results and their usefulness in clinical practice [16,30-32].
Maeda et al., in 2018 investigated nine candidate marker genes, including FLT3, LINC00643, RPRM, JAM2, ELMO1, BHLHE22, RIMS1, GUSBP5, and ZNF3 as epigenetic markers for gastric cancer risk stratification in individuals after H. pylori eradication [16]. The results showed that these genes had significantly higher methylation levels in gastric cancer patients than in gastric atrophy patients. The candidates had sufficient performance (AUC: 0.70-0.80) and high odds ratios (5.43-23.41). The methylation levels of these markers were not associated with gastric atrophy, gender, or age [16].
Using gastric wash DNA or gastric juice exosomal DNA, methylation level of BARHL2 gene was tested for its usefulness as a marker for detection of early gastric cancer. Yamamoto et al., found high levels of BARHL2 methylation in gastric washderived DNA obtained from early gastric cancer patients [32]. Analysis using gastric juice-derived exo DNA samples revealed that BARHL2 methylation yielded an area under the curve of 0.923 with 90% sensitivity and 100% specificity in discriminating gastric cancer patients from controls. Future studies are required to confirm if the gastric wash-derived DNA and/or gastric juice-derived exo DNA might be useful for early cancer detection in clinical setting.
Development of the intestinal subtype of gastric cancer is marked by a progression of histopathologic lesions. In a Colombian study in Andean regions in 2015, gastric biopsy samples were examined on the effects of H. pylori eradication and antioxidants treatment on the progression of gastric lesions, the patients were followed for 6,12, and 16 years [30]. Methylation levels of AMPH, PCDH10, RSPO2, SORCS3, and ZNF610 genes were able to predict progression of gastric lesions independent of the effect of duration of H. pylori infection, baseline diagnosis, gender of the patient, or scores for mononuclear leukocytes, polymorphonuclear leukocytes, or intraepithelial lymphocytes. Therefore, DNA methylation levels in AMPH, PCDH10, RSPO2, SORCS3, and ZNF610 may contribute to the identification of persons with gastric lesions likely to progress [30].
Metachronous gastric cancer (MGC) can develop after endoscopic tumor resection. Suzuki et al. ,in 2014 tested if miR-34b/c, SFRP1, SFRP2, SFRP5, DKK2 and DKK3 genes promoter methylation might be able to predict the risk of MGC development after endoscopic tumor resection, they noted 17 (13%) out of 129 patients developed MGC after curative endoscopic therapy [33]. The cumulative incidence of MGC was significantly higher among patients with elevated miR-34b/c, SFRP2 and DKK2 methylation in their gastric body. MiR-34b/c showed the strongest association with the risk of MGC. In another multicenter prospective cohort study of 826 patients in 2015, miR-124a-3 has been suggested as a better predicated marker for predicting the risk of developing metachronous gastric cancer [34]. Further studies will be required to confirm these results and develop protocols for clinical tests.
Gene Polymorphisms And DNA Methylation In Gastric Cancer
Gene polymorphisms are associated with gastric carcinogenesis. DNA methylation in gastric cancer seems to be influenced by the presence of host gene polymorphisms and by H. pylori cagA/ vacAs1m1 strains [35].
da Costa et al., investigated the interleukin polymorphisms in gastric tumor samples during H. pylori infection. In cardia tumors, methylation in COX-2 promoter was associated with IL-1RA Allele 2(IL1RN*2) genotype, and the associated genotypes IL1B511T+IL1RN*2 seem to be important in the methylation of COX-2 gene, especially infected by H. pylori strains that carries cagA and vacAs1 [35]. The associated genotypes IL6 CC+TNF GG appear to be involved in the unmethylation of CDKN2A along with cagA-positive H. pylori infection.
The NF-κ B1 polymorphisms, -94 insertion (ins)/deletion (del) (rs28362491) and -449 C>G (rs72696119), were recently investigated for their effects on the aberrant gene methylation during H. pylori infection [36]. Methylation status was determined in p14ARF, p16INK4a, DAPK and CDH1 gene promoters in gastric mucosa. The results found that -94 del/del homozygosity was significantly associated with risk for developing CpG island methylation, and the number of methylated genes was significantly higher in -94 del/del homozygotes than in ins/del and ins/ins (ins carrier) in H. pyloriinfected elder subjects. In addition, the inflammation score was significantly higher in H. pylori-infected del/del homozygotes over the ins carriers. Therefore, NF-κ B1 -94 ins/del ATTG polymorphism (rs28362491) is associated with increased risk developing age-related gene methylation in non-cancerous gastric mucosa during H. pylori infection [37].
Discussion
Genome-wide association study reveal polymorphisms (rs2294008) in prostate stem cell antigen (PSCA) gene are also associated with gastric cancer especially the diffuse type. PSCA rs2294008 C/T polymorphisms were genotyped in 410 cancerfree subjects in relation to promoter CpG island methylation status of three candidate genes (IGF2, MYOD1, and SLC16A12). Methylation levels of all three genes were significantly higher in subjects with PSCA rs2294008 T/T compared with the PSCA rs2294008 C/C, and H. pylori infection enhanced the methylation.
These observations provide evidences that host gene polymorphisms may influence the susceptibility of DNA methylation induction in gastric mucosa. However, the detailed molecular mechanisms and their impact of the cancer susceptibility remain to be explored. Future works are required to validate the results and their usefulness in identifying cancer susceptible candidates for disease prevention.
Conclusion
Methylation of CpG islands in gene promoter is one of the most characteristic abnormalities in H. pylori-induced gastric cancer; despite recent advance, the detailed molecular mechanisms remain to be investigated. H. pylori-induced inflammatory microenvironment, including increased inflammatory cell infiltration, reactive oxygen species, cytokines, growth factors and hormones production together impact on DNA methylation in epithelial cells and facilitate oncogenic transformation. Future studies addressing interactions of these factors and their impacts on other epigenetic events will be critical to uncover their roles in gastric carcinogenesis, and more importantly, will provide options for gastric cancer prevention and intervention.
Funding
This work was supported by grants to SZD from National Natural Science Foundation of China, No.U1604174; Henan Provincial Government-Health and Family Planning Commission, No. 20170123; Henan Provincial Government- Health and Family Planning Commission Research Innovative Talents Project, No.51282; and Henan Provincial Government- Science and Technology Bureau, No.142300410050.
The funding sources had no role in the design of this study and will not have any role during its execution, analyses, interpretation of the data, or decision to submit results.
Acknowledgement
Authors are grateful to the staffs of Dept.of Gastroenterology and Hepatology, People’s Hospital of Zhengzhou University for their valuable assistant in this work.
REFERENCES
- Malfertheiner P, Megraud F, O'Morain CA, Gisbert JP, Kuipers EJ, Axon AT, et al. Management of Helicobacter pylori infection-the Maastricht V/Florence Consensus Report. Gut. 2017;66(1):6-30.
- Sugano K, Tack J, Kuipers EJ, Graham DY, El-Omar EM, Miura S, et al. Kyoto global consensus report on Helicobacter pylori gastritis. Gut. 2015;64(9):1353-1367.
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424.
- Ding SZ, Goldberg JB, Hatakeyama M. Helicobacter pylori infection, oncogenic pathways and epigenetic mechanisms in gastric carcinogenesis. Future Oncol. 2010;6(5):851-62.
- Amieva M, Peek RM, Jr. Pathobiology of Helicobacter pylori-Induced Gastric Cancer. Gastroenterology. 2016;150(1):64-78.
- Knorr J, Ricci V, Hatakeyama M, Backert S. Classification of Helicobacter pylori Virulence Factors: Is cagA a Toxin or Not? Trends Microbiol. 2019;27(9):731-738.
- Dawson EM, Dunne KA, Richardson EJ, Praszkier R, Alfawaz D, Woelfel S, et al. Complete genome sequence of Helicobacter pylori B128 7.13 and a single-step method for the generation of unmarked mutations. Helicobacter. 2019;24(4): 12587.
- Ohnishi N, Yuasa H, Tanaka S, Sawa H, Miura M, Matsui A, et al. Transgenic expression of Helicobacter pylori CagA induces gastrointestinal and hematopoietic neoplasms in mouse. Proc Natl Acad Sci USA. 2008;105(3): 1003-1008.
- Franco AT, Johnston E, Krishna U, Yamaoka Y, Israel DA, Nagy TA, et al. Regulation of gastric carcinogenesis by Helicobacter pylori virulence factors. Cancer Res. 2008;68(2):379-387.
- Matos JI, de Sousa HA, Marcos-Pinto R, Dinis-Ribeiro M. Helicobacter pylori CagA and VacA genotypes and gastric phenotype: a meta-analysis. Eur J Gastroenterol Hepatol. 2013;25(12): 1431-141.
- Hatakeyama M. Structure and function of Helicobacter pylori CagA, the first-identified bacterial protein involved in human cancer. Proc Jpn Acad Ser B Phys Biol Sci. 2017;93(4): 196-219.
- Uemura N, Okamoto S, Yamamoto S, Matsumura N, Yamaguchi S,Yamakido M, et al. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med. 2001;345(11): 784-789.
- Esteller M. The necessity of a human epigenome project. Carcinogenesis. 2006;27(6):1121-1125.
- Rosenquist R, Esteller M, Plass C. Introduction: Epigenetics in cancer. Semin Cancer Biol. 2018;51:4-5.
- Maeda M, Moro H, Ushijima T. Mechanisms for the induction of gastric cancer by Helicobacter pylori infection: aberrant DNA methylation pathway. Gastric Cancer. 2017;20(1): 8-15.
- Maeda M, Yamashita S, Shimazu T, Iida N, Takeshima H, Nakajima T, et al. Novel epigenetic markers for gastric cancer risk stratification in individuals after Helicobacter pylori eradication. Gastric Cancer. 2018;21(5):745-55.
- Maekita T, Nakazawa K, Mihara M, Nakajima T, Yanaoka K, Iguchi M, et al. High levels of aberrant DNA methylation in Helicobacter pylori-infected gastric mucosae and its possible association with gastric cancer risk. Clin Cancer Res. 2006;12(1): 989-995.
- Ushijima T, Nakajima T, Maekita T. DNA methylation as a marker for the past and future. J Gastroenterol. 2006;41(5): 401-407.
- Chan AO, Peng JZ, Lam SK, Lai KC, Yuen MF, Cheung HKL, et al. Eradication of Helicobacter pylori infection reverses E-cadherin promoter hypermethylation. Gut. 2006;55(4):463-468.
- Tahara S, Tahara T, Horiguchi N, Kato T, Shinkai Y, Yamashita H, et al. DNA methylation accumulation in gastric mucosa adjacent to cancer after Helicobacter pylori eradication. Int J Cancer. 2019;144(1): 80-88.
- Choi J, Kim SG, Kim BG, Koh SJ, Kim JW, Lee KL. Helicobacter pylori eradication modulates aberrant cpG island hypermethylation in gastric carcinogenesis. Korean J Gastroenterol. 2016;68(5):253-259.
- Lu XX, Yu JL, Ying LS, Han J, Wang S, Yu QM, et al. Stepwise cumulation of RUNX3 methylation mediated by Helicobacter pylori infection contributes to gastric carcinoma progression. Cancer. 2012;118(22):5507-5517.
- Shin CM, Kim N, Lee HS, Park JH, Ahn S, Kang GH, et al. Changes in aberrant DNA methylation after Helicobacter pylori eradication: a long-term follow-up study. Int J Cancer. 2013;133(9):2034-242.
- Watari J, Ito C, Shimoda T, Tomita T, Oshima T, Fukui H, et al. DNA methylation silencing of microRNA gene methylator in the precancerous background mucosa with and without gastric cancer: Analysis of the effects of H. pylori eradication and long-term aspirin use. Sci Rep. 2019;9(1):12559.
- Takeshima H, Niwa T, Toyoda T, Wakabayashi M, Yamashita S, Ushijima T. Degree of methylation burden is determined by the exposure period to carcinogenic factors. Cancer Sci. 2017;108(3):316-321.
- Schneider BG, Piazuelo MB, Sicinschi LA, Mera R, Peng DF, Roa JC, et al. Virulence of infecting Helicobacter pylori strains and intensity of mononuclear cell infiltration are associated with levels of DNA hypermethylation in gastric mucosae. Epigenetics. 2013;8(11):1153-1161.
- Zhang BG, Hu L, Zang MD, Wang HX, Zhao W, Li JF, et al. Helicobacter pylori CagA induces tumor suppressor gene hypermethylation by upregulating DNMT1 via AKT- NF-κB pathway in gastric cancer development. Oncotarget. 2016;7(9):9788-9800.
- Alves MK, Ferrasi AC, Lima VP, Ferreira MV, de Moura Campos Pardini MI, Rabenhorst SH. Inactivation of COX-2, HMLH1 and CDKN2A gene by promoter methylation in gastric cancer: relationship with histological subtype, tumor location and Helicobacter pylori genotype. Pathobiology. 2011;78(5):266-276.
- Woo HD, Fernandez-Jimenez N, Ghantous A, Esposti DD, Cuenin C, Cahais V, et al. Genome-wide profiling of normal gastric mucosa identifies Helicobacter pylori- and cancer-associated DNA methylome changes. Int J Cancer. 2018;143(3): 597-609.
- Schneider BG, Mera R, Piazuelo MB, Bravo JC, Zabaleta J, Delgado AG, et al. DNA methylation predicts progression of human gastric lesions. Cancer Epidemiol Biomarkers Prev. 2015;24(10):1607-1613.
- Tahara T, Arisawa T. DNA methylation as a molecular biomarker in gastric cancer. Epigenomics. 2015;7(3):475-486.
- Yamamoto H, Watanabe Y, Oikawa R, Morita R, Yoshida Y, Maehata T, et al. Barhl2 methylation using gastric wash DNA or gastric juice exosomal DNA is a useful marker for early detection of gastric cancer in an H. pylori-independent manner. Clin Transl Gastroenterol. 2016;7(7):184.
- Suzuki R, Yamamoto E, Nojima M, Maruyama R, Yamano H, Yoshikawa K, et al. Aberrant methylation of microRNA-34b/c is a predictive marker of metachronous gastric cancer risk. J Gastroenterol. 2014;49(7):1135-1144.
- Asada K, Nakajima T, Shimazu T, Yamamichi N, MaekitaT, Yokoi C, et al. Demonstration of the usefulness of epigenetic cancer risk prediction by a multicentre prospective cohort study. Gut. 2015;64(3):388-396.
- da Costa DM, Neves-Filho EH, Alves MK, Rabenhorst SH. Interleukin polymorphisms and differential methylation status in gastric cancer: an association with Helicobacter pylori infection. Epigenomics. 2013;5(2):167-75.
- Arisawa T, Tahara T, Shiroeda H, Yamada H, Nomura T, Hayashi R, et al. NF-κB1 polymorphism is associated with age-related gene methylation in Helicobacter pylori-infected subjects. Int J Mol Med. 2012;30(2): 255-262.
- Tahara T, Tahara S, Horiguchi N, Kato T, Shinkai Y, Okubo M, et al. Prostate stem cell antigen gene polymorphism is associated with H. pylori-related promoter DNA methylation in nonneoplastic gastric epithelium. Cancer Prev Res (Phila). 2019;12(9):579-584.
Citation: Qi YB, Hu RB, Ding SZ, Khan MN, Lei L, Wei PR, et al. (2020) Helicobacter pylori Infection, DNA Methylation, and Gastric Carcinogenesis. J Carcinog Mutagen. 11:352.DOI:10.35248/2157-2518.20.11.352.
Copyright: © 2020 Qi YB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : This work was supported by grants to SZD from National Natural Science Foundation of China, No.U1604174; Henan Provincial Government-Health and Family Planning Commission, No. 20170123; Henan Provincial GovernmentHealth and Family Planning Commission Research Innovative Talents Project, No.51282; and Henan Provincial GovernmentScience and Technology Bureau, No.142300410050.