Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2024) Volume 9, Issue 1
Glaucoma Implant Surgery in Cornelia de Lange Syndrome Associated Congenital Glaucoma
Balqees Al Mahrezi1*, Huda Abdullah Al Farsi2 and Ali Mouhammad Deeb Alsheikheh22Department of Ophthalmology, Al Nahdha Hospital, Muscat, Oman
Received: 17-Nov-2023, Manuscript No. JEDD-23-24398; Editor assigned: 20-Nov-2023, Pre QC No. JEDD-23-24398 (PQ); Reviewed: 04-Dec-2023, QC No. JEDD-23-24398; Revised: 11-Dec-2023, Manuscript No. JEDD-23-24398 (R); Published: 18-Dec-2023, DOI: 10.35248/2684-1622.23.8.227
Abstract
Cornelia de Lange Syndrome (CdLS) is a rare multisystem congenital disorder marked by psychomotor retardation and delayed growth, along with a variety of malformations such as facial dysmorphia, upper-extremity malformations, hirsutism, cardiac defects, and gastrointestinal abnormalities. Ocular abnormalities are seen in the majority of CdLS patients. Common findings include long eyelashes, synophrys, hirsutism of the eyebrows, peripapillary pigment ring, and myopia. Congenital glaucoma is a rare ocular association in such condition. We present a case of Cornelia de Lange Syndrome associated with bilateral congenital glaucoma.
Introduction
Cornelia de Lange syndrome (CdLS) is a rare multisystem congenital disorder. It is also known as Brachmann de Lange syndrome. It is distinguished by facial dysmorphism, mental retardation, growth retardation, developmental delay, distal limb anomalies, gastroesophageal dysfunction, genitourinary anomalies, hirsutism, pyloric stenosis, congenital diaphragmatic hernias, cardiac septal defects, hearing loss, and ophthalmologic anomalies [1]. The syndrome was first described by Cornelia de Lange, in 1933, although Brachmann described a child with similar features in 1916 [2]. The prevalence of CdLS may be as high as 1 case per 10 000 people, and although familial autosomal dominant cases have been reported, most cases seem to be sporadic [3-6]. Mutations in NIPBL, SMC1A, HDAC8, SMC3, or RAD21 have been linked to the syndrome A clinical evaluation of 181 people with this condition revealed that 57% had ocular abnormalities [7]. Common ocular findings described in the literature include long eyelashes, synophrys, hirsutism of the eyebrows, peripapillary pigment ring, and myopia. Hyperopia, ptosis, blepharitis, short palpebral fissure length, down-slanting palpebral fissures, mild micro cornea, strabismus, nystagmus, and optic nerve abnormalities are less common findings [8]. Congenital glaucoma is a rare ophthalmic manifestation in such a condition. In this case, we aim to present a successfully managed congenital glaucoma in a child with Cornelia de Lange syndrome.
Case Presentation
A one-month-old female baby with Cornelia de Lange syndrome with classical facial features was referred to the Department of Ophthalmology to rule out glaucoma in view of bilateral cloudy cornea. The baby was the third born child of the couple, born at 35 weeks of gestation by caesarean section due to severe polyhydramnios. Mother had gestational diabetes mellitus. The birth weight was 1600 g, length of 38 cm, and head circumference of 27 cm. Child was kept in Neonatal Intensive Care Unit for 42 days due to respiratory distress and low growth parameters. Anomaly scan at age 20 weeks of gestation reported: Akinesia, abnormal head shape, short neck, limited motions of limbs, right hand missing and small right forearm.
There was no history of consanguinity. There was no family history of congenital anomalies or similar complaints. The other two siblings were healthy.
On Clinical Examination, the child had microcephaly, small anterior fontanelle, long arcuate eyelashes, synophrys, up slant palpebral fissures, short upturned nose, thin downturned lips, low set ears, micrognathia, retrognathia, short neck, subcostal retraction and hirsutism (Figures 1-3).
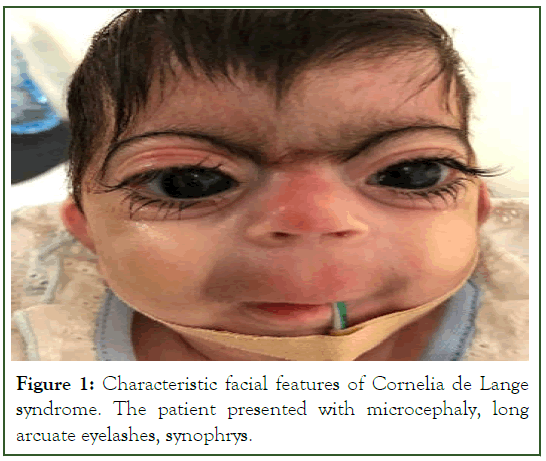
Figure 1: Characteristic facial features of Cornelia de Lange syndrome. The patient presented with microcephaly, long arcuate eyelashes, synophrys.
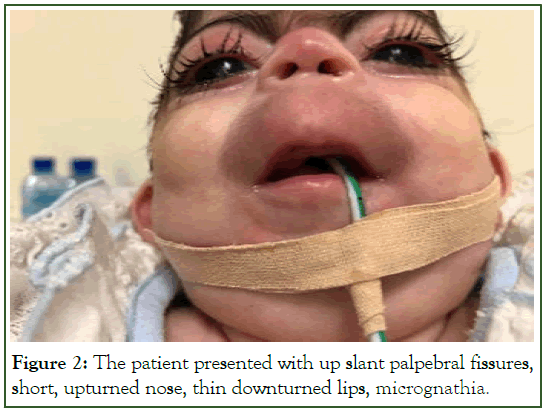
Figure 2: The patient presented with up slant palpebral fissures, short, upturned nose, thin downturned lips, micrognathia.
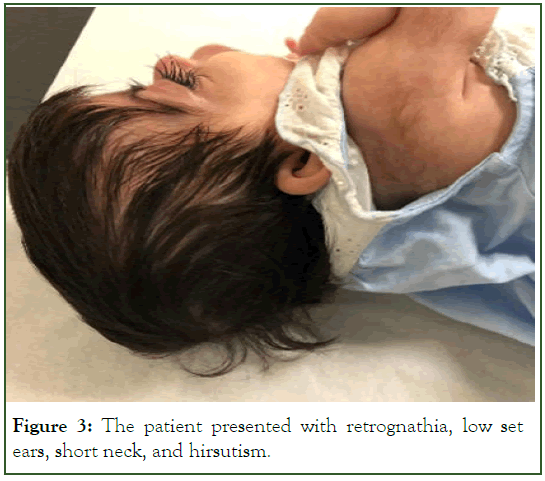
Figure 3: The patient presented with retrognathia, low set ears, short neck, and hirsutism.
In addition to a missed right ulnar, small feet, overriding toes and joint contractures (Figures 4 and 5). Echocardiogram revealed Patent Ductus Arteriosus with Patent Foramen Ovale and Hypoplastic pulmonary artery and its branches.

Figure 4: Demonstrate the limbal anomalies: Right ulnar hypoplasia of the forearm.
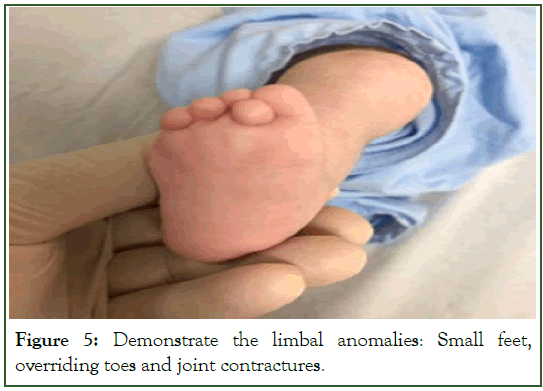
Figure 5: Demonstrate the limbal anomalies: Small feet, overriding toes and joint contractures.
On Ophthalmological examination, the child had bilateral megalo-cloudy corneas and Haab’s striae (Figures 6 and 7). Intraocular Pressure (IOP) measured using Perkin’s applanation tonometer was 30 mmHg in Right eye (Oculus Dexter (OD)) and 26 mmHg in Left eye (Oculus Sinister (OS)). Fundus examination showed both eyes (Oculus Uterque (OU)) large disc, Cup: disc ratio 0.7, attached Retina. In view of these ocular examination findings, a diagnosis of congenital glaucoma was made. The child was started on topical (10 mg/ml Brinzolamide+5 mg/ml Timolol) twice daily and Latanoprost (50 mcg/1 ml) at bedtime. Parents were informed about the need for surgery to treat glaucoma. IOP on previously mentioned glaucoma treatment was 31 mmHg and 25 mmHg in OD and OS respectively on review after 2 weeks.
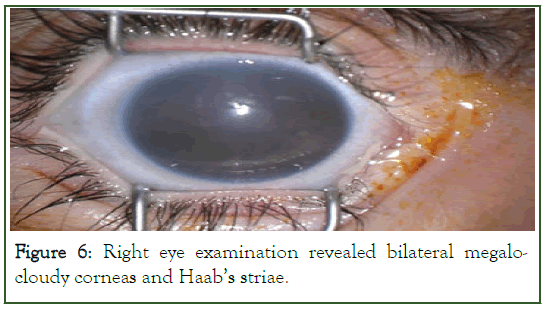
Figure 6: Right eye examination revealed bilateral megalocloudy corneas and Haab’s striae.
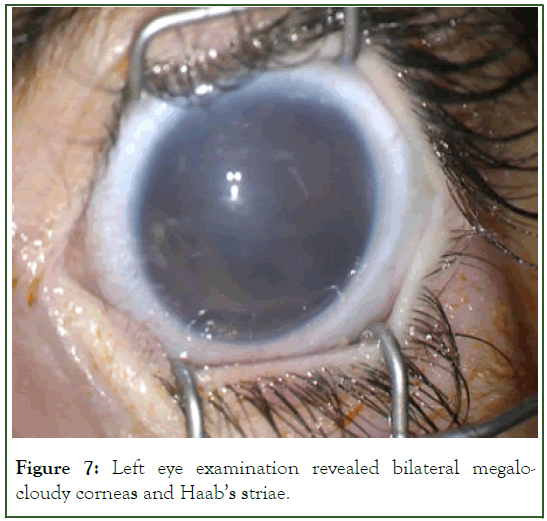
Figure 7: Left eye examination revealed bilateral megalocloudy corneas and Haab’s striae.
Patient was seen by anesthesiologist and high risk of death on table if patient taken under general anesthesia for examination and surgical intervention explained to the parents. After parents counselling, they decided to continue the eye drops till the baby grow up and can handle general anesthesia in a better way.
After more stabilization of the general condition, a High-Risk Anesthesia Consent was taken and examination under general anesthesia was done at the age of 8 months to confirm the diagnosis and management. On examination, IOP was 22 mmHg and 26 mmHg in OD and OS respectively by Perkin’s applanation tonometer. Fundus examination revealed Cup: disc ratio 0.8. Axial Length was 21.41 mm and 21.21 mm in OD and OS respectively. According to the high risk of any long duration surgery and frequent anesthesia, we decided to do transscleral Micropulse Cyclophotocoagulation (MPCPC) for Both Eyes. MPCPC was done according to the following parameters: OD: 2500 mW for 120 seconds inferior hemisphere and 2500 mW for 90 seconds superior hemisphere, OS: 2500 mW for 120 seconds inferior hemisphere and 2500 mW for 120 seconds superior hemisphere. After two weeks, IOP was 18 mmHg with timolol and brinzolamide in OU (measured using tonopen in the clinic) with less cloudiness of both corneas.
After two months, the general condition of the child was more stable but still under high risk for general anesthesia and the intraocular pressure started to raise up again and the decision was made to proceed with Ahmed glaucoma valve implantation. We Avoided trabeculotomy or trabeculotomy combined with trabeculectomy because of the general health condition and the high risk of morbidity and mortality with frequent general anesthesia exposure that may be expected after these types of surgeries. So, Ahmed Glaucoma Valve Surgery was done first at the right eye at the age of 11 months (Figure 8). On review after 1 week in the clinic, IOP without topical medications was 14 mmHg in OD and 36 mmHg in OS on three glaucoma drugs: (timolol/ brinzolamide) and Latanoprost.
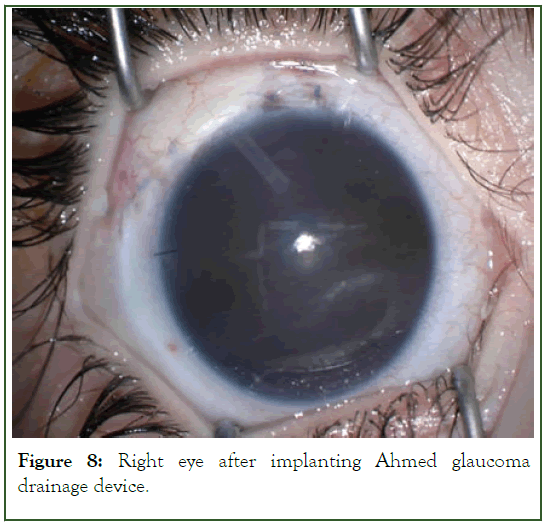
Figure 8: Right eye after implanting Ahmed glaucoma drainage device.
Depending on the anesthetist opinion after re-evaluating the general condition of the child, Ahmed Glaucoma Valve Surgery in the left eye was done one month later (Figure 9). On review after 1 week in the clinic, IOP without topical medications was 14 mmHg in both eyes.
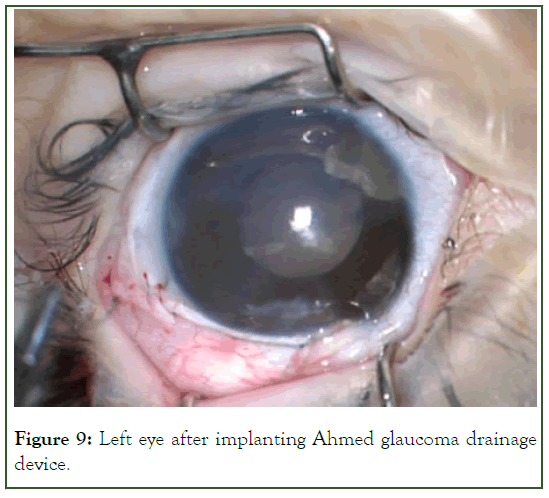
Figure 9: Left eye after implanting Ahmed glaucoma drainage device.
During follow ups after the surgery, IOP and other parameters (corneal diameter, axial length, and refraction) were stable. Last Follow up at the age of two years, IOP without topical medications was 14 and 12 mmHg in OD and OS respectively. Slit lamp examination revealed clear cornea and good tube position in both eyes, dilated fundus examination showed cup: disc ratio: 0.75 and 0.8 at OD and OS respectively. Axial Length was 21.81 mm and 20.69 mm in OD and OS respectively.
Discussion
Cornelia de Lange syndrome is a multisystem congenital disorder that is characterized by dysmorphic facial features, hirsutism, limb abnormalities, mental retardation, growth retardation, gastroesophageal dysfunction, cardiac, genitourinary, and ophthalmologic anomalies. Our reported patient had multiple systemic involvement as described in literature for CdLS.
The baby was the third born child of the married couple, born at age 35 weeks of gestation by emergency caesarean section due to severe polyhydramnios. Mother had Gestational diabetes mellitus. There was no history of consanguinity, but parents are from the same tribe. There was no family history of congenital anomalies or syndromes. The other two siblings were healthy. Clinical Geneticist was consulted, and normal Karyotyping and normal array comparative genomic hybridization were reported. No further genetic testing was done. The characteristic facial and multisystemic features led to the diagnosis of Cornelia de Lange syndrome.
There are few studies of ophthalmologic findings in CdLS. Levin et al published the largest study that involved complete ophthalmologic examinations, including 22 patients with CdLS demonstrating prevalence rates of 95% for synophrys, 90% for long arcuate eyelashes, 53% for hypertelorism, 50% for telecanthus, 60% for myopia, 59% for any degree of Nasolacrimal Duct Obstruction (NLDO), 45% for ptosis, 22% for strabismus, and 15% for nystagmus [9].
Our patient had synophrys, long arcuate eyelashes, hypertelorism, telecanthus, and Myopia. Bilateral congenital glaucoma was confirmed after consideration of all parameters (megalo-cloudy cornea with Haab’s striae, Axial length and IOP) and was managed successfully by MPCPC and later by Ahmed Glaucoma Valve implantation.
Five cases of congenital glaucoma have been reported to our knowledge [10-13]. In three of these cases, the patient had a frameshift mutation in the NIPBL gene, one patient had a de novo mutation in chromosome 11, and the other patient had no genotyping analysis. One of these patients had mosaic Turner syndrome as well [11,13]. Another child had glaucoma and retinoblastoma in one eye [14]. CdLS and Peters abnormality have been documented in one case in an infant who received corneal transplantation and later acquired glaucoma [15]. Ahmed glaucoma valve was used to treat the case of congenital glaucoma associated with aniridia [12].
In our patient both eyes were treated with Ahmed glaucoma valve and successfully showed reduction of intraocular pressure without the use of topical anti-glaucoma medications.
Conclusion
Diagnosis of CdLS depends on the characteristic facial features and physical features. Although congenital glaucoma is a rare manifestation of the disease, it should be kept in mind in the presence of typical ocular signs or symptoms. Management of such cases is a challenging task for glaucoma specialist. Sometimes, surgeons have to change their choice of surgical intervention in pediatric patients depends on their general health status to reduce the risk of morbidity and mortality in such cases.
Author Contributions
• Al Mahrezi B. is the first author who had a direct patient contact and wrote the largest share of the report. She is also the one who wrote the final revised report and submitted it to the journal.
• Al Farsi H. is the second author who is taking care of the patient and contributes in designing, drafting, and revising the case report and also giving the final approval of the submitted version.
• Alsheikheh Ali is the senior author and the main caregiver of the patient. He contributes in analyzing the data of the report and revise it critically and give the final approval of the version to be published.
Acknowledgements
The Authors would like to thank the patient's family for their cooperation.
Funding
None
Conflict of Interest
The Authors declare that there are no competing interests.
References
- Lange D. Sur un type nouveau de degeneration (typus Amstelodamensis). Arch Ned Enfant. 1933;36:713-719.
- Brachmann W, Erziehung JK. A case of symmetrical monodactyly representing ulnar deficiency, with symmetrical antecubital webbing and other abnormalities (dwarfish, cervical ribs, hirsutism). Jahrb Kinderheilkd Physische Erziehung. 1916;84:225-235.
- Opitz JM. The Brachmann–de Lange syndrome. Am J Med Genet. 1985;22(1):89- 102
- Russell KL, Ming JE, Patel K, Jukofsky L, Magnusson M, Krantz ID. Dominant paternal transmission of Cornelia de Lange syndrome: A new case and review of 25 previously reported familial recurrences. Am J Med Genet. 2001;104(4):267-276.
- Gillis LA, McCallum J, Kaur M, DeScipio C, Yaeger D, Mariani A, et al. NIPBL mutational analysis in 120 individuals with Cornelia de Lange syndrome and evaluation of genotype-phenotype correlations. Am J Hum Genet. 2004;75(4):610-623.
- Boyle MI, Jespersgaard C, Brondum-Nielsen K, Bisgaard AM, Tumer Z. Cornelia de Lange syndrome. Clin Genet. 2015; 88 (1):1–12.
[Crossref]
- Jackson L, Kline AD, Barr MA, Koch SD. de Lange syndrome: A clinical review of 310 individuals. Am J Hum Genet. 1993;47(7):940-946.
- Shi A, Levin AV. Ophthalmologic findings in the Cornelia de Lange syndrome. Ophthalmic Genet. 2019;40(1):1-6.
- Levin AV, Seidman DJ, Nelson LB, Jackson LG. Ophthalmologic findings in the Cornelia de Lange syndrome. J Pediatr Ophthalmol Strabismus. 1990;27(2):94-99.
- Nallasamy S, Kherani F, Yaeger D, McCallum J, Kaur M, Devoto M, et al. Ophthalmologic findings in Cornelia de Lange syndrome: a genotype-phenotype correlation study. Arch Ophthalmol. 2006;124(4):552-527.
- Wierzba J, Gil-Rodríguez MC, Polucha A, Puisac B, Arnedo M, Teresa-Rodrigo Me, et al. Cornelia de Lange syndrome with NIPBL mutation and mosaic Turner syndrome in the same individual. BMC Med Genet. 2012;13:1-8.
- Lee WB, Brandt JD, Mannis MJ, Huang CQ, Rabin GJ. Aniridia and Brachmann-de Lange syndrome: A review of ocular surface and anterior segment findings. Cornea. 2003;22(2):178-180.
- Pai V, Rander A. Cornelia de Lange Syndrome with Congenital Glaucoma. J Eye Dis Disord. 2017;2(106):1-2.
- Lim KH, Wong HB. Retinoblastoma in a Chinese girl with de Lange syndrome. Asian J Mod Med. 1974;10:272-273.
- Ponder SW, Cynamon HA, Isenberg JN, Elder FF, Lockhart L. Cornelia de Lange syndrome with Peters anomaly and fat malabsorption. Dysmorphol Clin Genet. 1988;2(1):2-5.
Citation: Al-Mahrezi B, Al-Farsi HA, Alsheikheh AMD (2023) Glaucoma Implant Surgery in Cornelia de Lange Syndrome Associated Congenital Glaucoma. J Eye Dis Disord. 8:227.
Copyright: © 2023 Al-Mahrezi B, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
