Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- The Global Impact Factor (GIF)
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
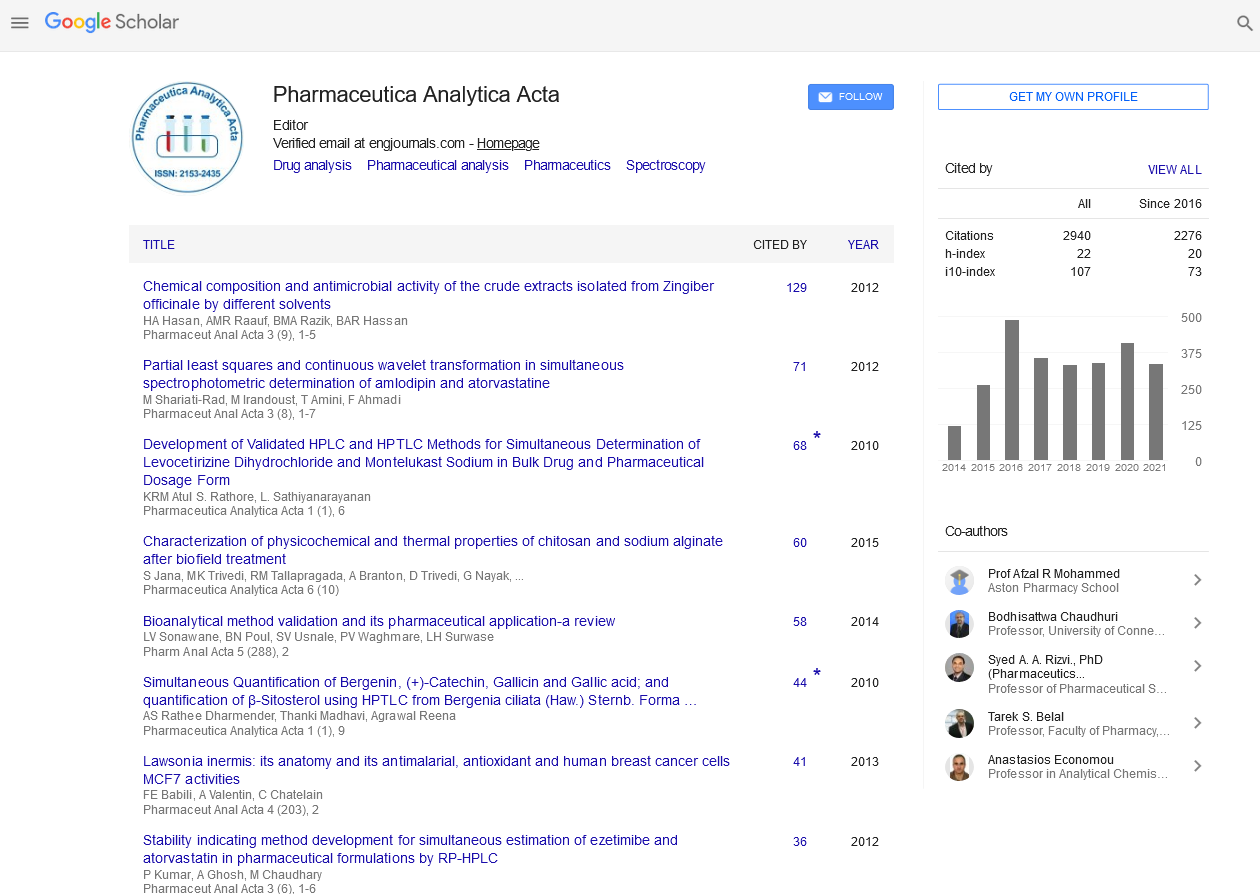
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion Article - (2025) Volume 16, Issue 1
Exploring the Role of Microbiomes in Drug Metabolism and Resistance
Emily Davis*Received: 27-Dec-2024, Manuscript No. PAA-25-28592; Editor assigned: 30-Dec-2024, Pre QC No. PAA-25-28592 (PQ); Reviewed: 13-Jan-2025, QC No. PAA-25-28592; Revised: 20-Jan-2025, Manuscript No. PAA-25-28592 (R); Published: 27-Jan-2025, DOI: 10.35248/2153-2435.25.16.806
Description
The role of microbiomes in the human body has become a major area of interest, particularly in how they influence drug metabolism and resistance. Microbiomes refer to the vast communities of microorganisms, including bacteria, fungi and viruses, that live within and on the human body. While these microbes are typically known for their involvement in digestion, immune system function and overall health, researchers are increasingly focusing on their potential impact on how the body processes medications and responds to treatments.
In addition to altering the potency of drugs, microbiomes can also influence the speed at which medications are processed. Some individuals may have a microbiome composition that allows for faster metabolism of a particular drug, leading to quicker clearance from the body. Others may have a slower metabolism, causing drugs to stay in the system longer and potentially lead to increased side effects or toxicity. These variations can significantly affect how patients respond to medication, as people with different microbiome compositions may experience vastly different outcomes when taking the same drug.
Another aspect of microbiomes influence on drug resistance lies in their interaction with the immune system. Microbial communities can play a role in how the immune system reacts to both infections and drugs. In the case of bacterial resistance to antibiotics, for instance, the microbiome can serve as a reservoir for resistant strains. These resistant bacteria can then transfer their resistance mechanisms to other bacteria in the body, making it harder to treat infections. The use of antibiotics, which can disrupt the balance of the microbiome, is often a contributing factor in the development of resistance. When antibiotics kill off beneficial bacteria, they leave space for harmful bacteria to thrive, which may be resistant to the drugs being used.
Interestingly, microbiomes can also have an effect on how cancer treatments work. Chemotherapy, which is designed to target and kill rapidly dividing cancer cells, can also harm normal cells, including those in the gut. This disruption can lead to changes in the microbiome that may affect the patient’s ability to tolerate treatment. Some studies have shown that a healthy microbiome may help reduce the side effects of chemotherapy, potentially allowing for higher doses or more frequent treatments. Conversely, an imbalance in the microbiome may increase the severity of side effects, reducing the effectiveness of the treatment and impairing the patient’s overall well-being.
The understanding of microbiomes’ role in drug metabolism and resistance is still in its early stages, but it has already led to a number of important insights. One of the most significant implications of this research is the potential for personalized medicine. As scientists learn more about how microbiomes affect drug responses, it may be possible to customize treatments for individuals based on their unique microbial composition. This approach could lead to more effective therapies with fewer side effects, as treatments would be designed to work with, rather than against, the patient’s microbiome.
In addition to personalized medicine, there is also growing interest in developing drugs that target the microbiome itself. By manipulating microbial communities, scientists may be able to influence drug metabolism and resistance in ways that enhance therapeutic outcomes. This could involve the use of probiotics, prebiotics, or other interventions aimed at restoring a healthy microbiome balance, potentially improving how drugs work and reducing the likelihood of resistance developing.
As research in this area continues to grow, it is clear that the microbiome plays a much larger role in drug metabolism and resistance than previously thought. By exploring the ways in which microorganisms interact with medications, researchers are opening up new avenues for more effective treatments, as well as strategies to combat drug resistance. The future of medicine may very well depend on our ability to understand and manipulate the complex relationship between the microbiome and drug responses, leading to therapies that are more effective and better suited to individual patient’s needs.
Citation: Davis E (2025). Exploring the Role of Microbiomes in Drug Metabolism and Resistance. Pharm Anal Acta. 16:806
Copyright: © 2025 Davis E. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.