Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- The Global Impact Factor (GIF)
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
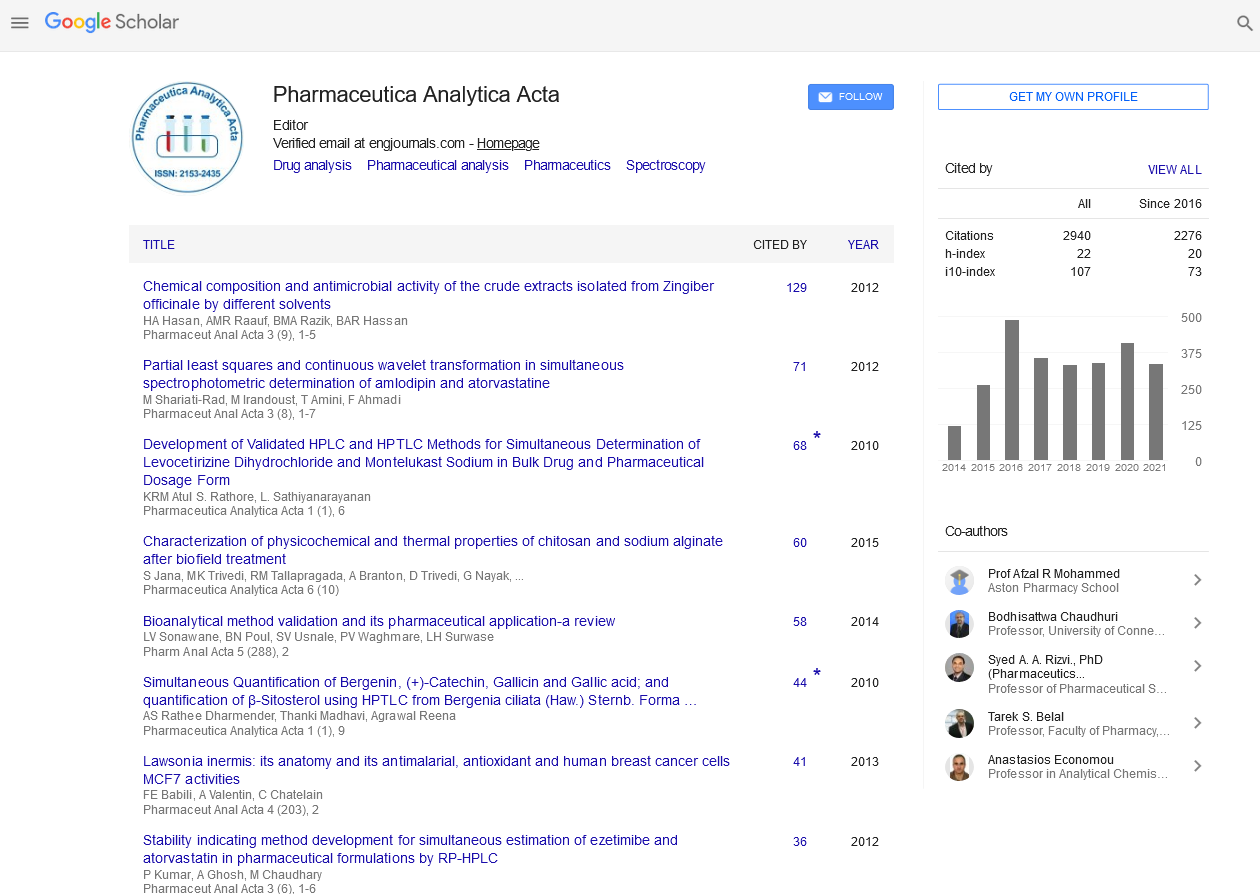
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2025) Volume 16, Issue 1
Exploring the Intersection of Drug Resistance Mechanisms and Immunotherapy
Andreas Schmidt*Received: 27-Dec-2024, Manuscript No. PAA-25-28589; Editor assigned: 30-Dec-2024, Pre QC No. PAA-25-28589 (PQ); Reviewed: 13-Jan-2025, QC No. PAA-25-28589; Revised: 20-Jan-2025, Manuscript No. PAA-25-28589 (R); Published: 27-Jan-2025, DOI: 10.35248/2153-2435.25.16.803
Description
Drug resistance and immunotherapy are two of the most significant areas of research in modern medicine. These subjects are interrelated, with drug resistance presenting a major challenge in the development of effective treatments, while immunotherapy is emerging as a promising avenue for addressing various diseases, particularly cancer. Understanding how drug resistance evolves in the context of immunotherapy is vital to improving treatment outcomes and helping to overcome the barriers that hinder long-term effectiveness.
Drug resistance refers to the ability of a disease, particularly cancer or infectious diseases, to evolve in response to treatment. When a patient undergoes treatment with a particular drug, most of the cells affected by the drug are eliminated. However, a small fraction of cells may survive and adapt to the drug, ultimately rendering the treatment less effective or even ineffective. In the context of cancer, this can result in the recurrence of the disease, as drug-resistant cancer cells proliferate and spread. Similarly, in the treatment of bacterial or viral infections, resistance can emerge when pathogens evolve mechanisms that make them immune to the effects of antibiotics or antiviral drugs.
The intersection of drug resistance mechanisms and immunotherapy is a complex issue. Several factors contribute to the development of resistance, including genetic mutations, the tumor microenvironment and the ability of cancer cells to evade immune detection. In many cases, resistance mechanisms that have been established against traditional chemotherapy drugs also contribute to resistance to immunotherapy. For example, tumors may develop the ability to repair the damage caused by immune system attacks, or they may adapt by altering their surface proteins to avoid recognition by immune cells.
One of the most significant challenges in immunotherapy is the phenomenon of immune checkpoint inhibition resistance. Immune checkpoints are regulatory pathways in the immune system that help maintain balance and prevent overactivation of immune responses, which could damage healthy tissues. Many immunotherapies work by blocking these checkpoints, effectively allowing the immune system to attack cancer cells more aggressively. However, some tumors develop ways to bypass this inhibition, leading to immune escape and resistance to treatment.
The evolution of drug resistance also involves changes within the immune system itself. Tumor cells may secrete substances that suppress immune activity or promote an environment that hinders immune cells' ability to infiltrate and attack the tumor. In addition, immune cells can become exhausted or less responsive over time, reducing their effectiveness in attacking cancer cells. These immune adaptations play a crucial role in limiting the success of immunotherapy, often resulting in reduced clinical outcomes and shorter survival times for patients.
Research into overcoming drug resistance mechanisms in the context of immunotherapy is ongoing. Scientists are exploring various strategies to address the challenges posed by resistance. One approach is the combination of immunotherapy with other treatments, such as targeted therapies or chemotherapy. By using multiple modalities of treatment, researchers hope to overcome the mechanisms that contribute to resistance. For example, combining immune checkpoint inhibitors with targeted therapies could help to prevent tumors from adapting and evading the immune response.
Another strategy involves modifying the tumor microenvironment to make it more conducive to immune system activity. Some researchers are investigating ways to alter the tumor's ability to suppress immune cells or limit their access to the tumor site. Additionally, advancements in personalized medicine allow for the identification of specific genetic mutations and resistance markers in individual patients. By tailoring treatment plans to each patient's unique genetic profile, it may be possible to more effectively combat resistance and enhance the efficacy of immunotherapy.
Furthermore, developing new drugs and therapies that specifically target resistant cancer cells is an area of significant focus. As more becomes known about the genetic mutations and molecular pathways involved in drug resistance, researchers are finding new ways to target these mechanisms. These novel approaches aim to prevent or reverse resistance, allowing immunotherapy to continue working as intended.
Citation: Schmidt A (2025). Exploring the Intersection of Drug Resistance Mechanisms and Immunotherapy. Pharm Anal Acta. 16:803
Copyright: © 2025 Schmidt A. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.