Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 0, Issue 0
Evaluation of Patient Preferences for Treatments to Prevent Preterm Births in Singleton and Twin Pregnancies with a Short Cervix
Sabrina de Andrade Fernandes Collier Perrusi1, Maria de Lourdes Brizot1, Sckarlet Ernandes Biancolin Garavazzo2, Camila Luiza Meira Pucci1, Ursula Trovato Gomez2, Stela Verzinhasse Peres2, Juliana Valente Codato Marinelli1, Rossana Pulcineli Vieira Francisco1 and Mario Henrique Burlacchini de Carvalho1*2Obstetrics Clinic Division, HCFMUSP Clinics Hospital, Medical School, University of São Paulo, São Paulo, Brazil
Received: 20-Jul-2023, Manuscript No. CMCH-23-22262; Editor assigned: 24-Jul-2023, Pre QC No. CMCH-23-22262 (PQ); Reviewed: 07-Aug-2023, QC No. CMCH-23-22262; Revised: 14-Aug-2023, Manuscript No. CMCH-23-22262 (R); Published: 21-Aug-2023, DOI: 10.35248/2090-7214.23.S17.001
Abstract
Background: Prematurity is the primary cause of neonatal morbidity and mortality. Despite some treatment methods, the preferences and concerns of women regarding the prevention of premature births have not yet been elucidated. Thus, this study analyzed singleton and twin pregnancies with an increased risk of prematurity to evaluate patient preferences for treatment and the factors that may influence such preferences.
Methods: Self-administered questionnaires in Portuguese were administered to pregnant women to collect data about their knowledge and concerns regarding prematurity and treatment methods (pessary, progesterone ovules and combination of a pessary and progesterone) as well as their preferred methods. Questionnaires were also used to assess the anxiety and quality of life of the participants. The chi-square, Fisher’s Exact, and Linear-by-Linear association tests were used to compare qualitative independent variables and qualitative outcomes. The Student’s t-test and Analysis of Variance (ANOVA) were used to compare the quantitative independent variables and qualitative outcomes. The Mann–Whitney or Kruskal–Wallis tests were used for non-parametric data.
Results: The study included 123 pregnant women with a short cervix (twin pregnancies, n=61; singleton pregnancies, n=62) from May 2009 to January 2022. As for their preferences, women with singleton pregnancies preferred to use a pessary (53.2%), but with no significant difference (P=0.703) compared to progesterone (46.8%). Women with twin pregnancies preferred the combination of a pessary and progesterone (P+P) (60.7%), followed by ovules (26.2%) and a pessary (8%), with a significant difference in this choice (P<0.001). Previous knowledge of the pessary by pregnant women with twins resulted in a significantly higher preference for the use of the pessary alone compared to P+P (37.5% vs. 5.7%; P=0.04), and no patients chose ovules.
Conclusion: The higher risk of prematurity in twin pregnancies and the lack of studies showing effective treatments for twin pregnancies may have contributed to the higher preference for the combined use of P+P. Women with singleton pregnancies showed no preference between the methods. This may be due to the fact that use of pessary and progesterone has already been proven to be effective in singleton pregnancies.
Keywords
Preterm birth prevention; Treatment preference; Pessary; Progesterone; Singleton pregnancy; Twin pregnancy; Anxiety; Quality of life.
Introduction
Prematurity is the main cause of neonatal morbidity and mortality with significant impact on public health [1]. Notably, Brazil is in the tenth place in the world ranking of prematurity [2]. According to the Brazilian Unified Health System (Sistema Único de Saúde- SUS), 11% of live births were preterm in 2019, increasing to 12.19% in 2021 [2]. In addition, prematurity causes fear anxiety, and questions about pregnancy, and its possible outcomes to pregnant women.
Among the intervention options to prevent prematurity, vaginal progesterone and use of cervical pessary have been extensively studied in women with a short cervix due to the high risk of prematurity. These methods significantly reduced the prematurity in high-risk singleton pregnancies [3]. However, there is no consensus among studies on the effectiveness of these methods in twin pregnancies with a short cervix. Therefore, studies are still investigating this subject [4].
We found no studies in the literature evaluating the preference for the method of prevention (pessary or progesterone) in pregnant women at risk of premature delivery. A study on pregnant women with and without risk for prematurity showed a higher preference for interventions (cervix length measurement and progesterone administration) in the risk group compared to the group without risk, in which the highest preference was for no management during pregnancy [5]. However, a recent study on third-trimester pregnancies with no real risk of prematurity used questionnaires to evaluate the preferences and concerns of women regarding prematurity prevention methods (pessary, progesterone, or cerclage) [6]. The study showed a higher preference of pregnant women (65.8%) for not using methods to prevent prematurity in case of a higher risk of preterm delivery. In addition, women who opted for prevention chose a single treatment rather than a combined one, and progesterone was the treatment of choice for the majority of pregnant women (84.9%) [6]. However, we assumed that the outcomes of hypothetical and real studies may differ according to the situations of risk or not. Therefore, the preferences for prematurity prevention methods are still vague in the literature.
Considering the patients’ values and preferences often helps physicians understand their different choices, such as a more active or palliative treatment. Knowledge of patient preference by treatment methods can also assist in the counseling and use of the same. Futhermore, method preference can influence adherence to patient treatment and satisfaction in relation to the proposed treatment.
Research on intervention methods to prevent prematurity is ongoing in our department, both in singleton and twin pregnancies with a short cervix; therefore, the present study evaluates the preferences of these pregnant women for the investigated treatments (pessary, progesterone, combined use of pessary and progesterone (P+P), or no method) and the factors that may influence this preference.
Materials and Methods
Recruitment
This prospective study included patients participating in two studies ongoing at the Department of Obstetrics and Gynecology, Clinics Hospital of the Medical School of the University of São Paulo (Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo-HCFMUSP) comparing methods for preventing prematurity in twin and singleton pregnancies with a short cervix from May 2019 to January 2022. Participants in the above-mentioned studies were informed regarding the risks of prematurity and on the methods of investigation for preventing it. The study on singleton pregnancies compared the pessary and progesterone ovule methods and the patients were told that both treatments were effective. The study on twin pregnancies compared the methods of isolated pessary, P+P, or isolated ovules that could contain progesterone or placebo. Moreover, these pregnant women were informed that such methods have not yet been proven to be effective in this type of pregnancy. The patients were instructed on the use of ovules in the vagina and the method of placing the pessary through vaginal examination, maintaining the randomized treatment for up to 37 weeks in singleton pregnancies or up to 36 weeks in twin pregnancies. Before the randomization of the described studies, the patients were invited to participate in the research on patient preferences for prematurity prevention methods using self-administered questionnaires in Portuguese. Figure 1 shows the study flowchart 1. All the study participants signed an informed consent form and received prenatal care at this service. The project was approved by the HCFMUSP Research Ethics Committee (CAAE: 15278819.0.0000.0068).
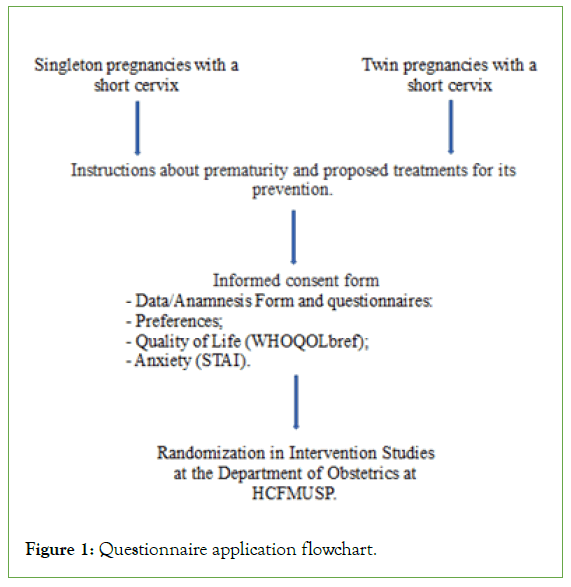
Figure 1: Questionnaire application flowchart.
Eligibility criteria
The patients participating in the studies “Comparison between natural progesterone and cervical pessary in the prevention of spontaneous preterm delivery in singleton pregnancies with a cervix less than or equal to 25 mm” (ClinicalTrials.gov Identifier: NCT02511574) and “Natural progesterone combined with a cervical pessary in twin pregnancies with a short cervix: Prospective and randomized study for the prevention of preterm birth” (ClinicalTrials.gov Identifier: NCT03058536) were eligible to participate in this study. The inclusion criteria for the study with singleton pregnancies were singleton pregnancies, gestational age between 20 weeks and 23 weeks and 6 days with asymptomatic short cervical length (less than or equal to 25 mm). For twin pregnancies, the inclusion criteria were twin pregnancy (dichorionic or monochorionic diamniotic), gestational age between 16 weeks and 27 weeks and 6 days, asymptomatic short cervical length according to the gestational age (measurement less or equal 30 mm between 16 weeks+0 days and 22 weeks+0 days, less or equal 25 mm between 22 weeks+1 day and 24 weeks+0 days and less or equal 20 mm between 24 weeks+1 day and 27 weeks+6 days). The inclusion criteria common to both studies were live fetuses without fetal malformations at ultrasound scan, intact fetal membranes, absence of bulging fetal membranes into the vagina, and an absence of placenta previa. The exclusion criteria were patients who do not understand the questionnaires, or patients who do not speak or read in Portuguese.
Questionnaire
The questionnaire to evaluate the preferences (S1) on preterm birth prevention in pregnant women at real risk of prematurity was based on practical issues that could relate to the choice of methods studied. Therefore, this questionnaire included questions on the following aspects: 1. knowing about prematurity; 2. knowing about the methods studied; 3. whether they would use the methods; 4. preferable methods; and 5. concerns about the side effects of the methods. The questions 1,2,6,7,8, and 9 presented Likert-type five- point responses (not at all (0), a little (1), moderately (2), a lot (3), and extremely (4)) [7]. The statements 3,4, and 5 were multiple- choice questions with a single answer (S1). This instrument was developed by the researchers specifically for the present study after a search in the scientific literature for tools that met the research objectives. The questionnaires were reviewed by three professors from the Department of Obstetrics, who discussed the topic and the wording of the elaborated items. The final version of the instrument was administered to ten pregnant patients who were not necessarily at risk of prematurity. These patients were asked to evaluate each item in the questionnaire, in addition to filling out their perception of prematurity and method preferences. A five- point numerical scale (from 0–4) was used to assess the easiness to understand the instrument as a whole and each question separately (0=I did not understand anything, to 4=I understood perfectly and I have no questions). Values above three were considered indicators of sufficient understanding. Comprehension was considered sufficient when at least 80% of the participants demonstrated full understanding of the evaluated item. Cronbach’s α was used to evaluate the internal consistency, with the nine items of the questionnaire showing high internal consistency (α=0.927). The medians of the responses were between 3 and 3.5, reaching 80% of the expected understanding.
The questionnaires WHOQOL-bref and STAI were subsequently administered [8-11].
The Quality of Life (QoL) questionnaire was assessed using the World Health Organization Quality of Life-Bref (WHOQOL-bref) instrument, validated for Portuguese [8,9]. The responses ranged from 1-5 on a Likert scale, from the worst to the best scenario [7]. The formula Domain X=(Domain X-4) × (100/16) was applied to transform the results into a scale from 0-100. Thus, the scores between 81 and 100 represent very good QoL; scores between 61 and 80 represent good QoL; scores between 41 and 60 represent neither bad nor good QoL; scores between 21 and 40 represent poor QoL; and scores between 81 and 20 represent very poor QoL [9].
The State-Trait Anxiety Inventory (STAI) questionnaire has two parallel scales, one to measure the T-Anxiety and the other E-Anxiety, each with 20 items [10,11]. In the STAI analysis, the total score was calculated by the simple sum of the questions ranging from 20-80 for each scale (trait and state). The anxiety levels were classified as low (score ≤ 32), moderate (score between 33-41), and high (score ≥ 42) [10].
Outcomes
The main outcome measure is the preferable method to treat short cervix (pessary, progesterone ovules, P+P, or no method) chosen by the pregnant women with short cervical length. The secondary outcomes included the influence of QoL, state, and trait anxiety on method preferences.
Sample size calculation
The sample size was calculated based on the hypothetical study by Ha and McDonald, which evaluated the degree of preference for methods to prevent premature births in patients with no real risk for prematurity [6]. In single pregnancies, the sample calculation considered the difference between the proportions of progesterone (85%) or pessary (6%) choices in the study [6]. Considering an alpha of 5% in a two-tailed hypothesis for a fixed sample, and reaching a minimum power of 80%, a sample of 32 patients was calculated for the pessary treatment and a sample of 30 patients was calculated for the progesterone treatment.
In twin pregnancies, the sample calculation considered the difference between the proportions of pessary (6%), P+P (50%), and progesterone (85%) observed in the study [6]. Considering an alpha of 5% in a two-tailed hypothesis for a fixed sample, and reaching a minimum power of 80%, the sample sizes were calculated for the pessary treatment (n=17), P+P treatment (n=16), and for the progesterone treatment (n=28).
Statistical analysis
A descriptive analysis of the data was performed using absolute (n) and relative (%) frequencies, central tendency measures (mean and median), and dispersion (standard deviation, minimum and maximum values, and percentiles).
The treatment preference distributions were compared using the binomial test for singleton pregnancies and the one-sample Chi- square test for twin pregnancies. Independent qualitative variables and qualitative outcomes (singleton or twin pregnancy, types of treatment methods, preference for methods, anxiety and QoL, and adherence to treatment according to preference) were compared using the chi-square, Fisher’s Exact, and Linear-by-Linear association tests, according to the characteristics of the variables. The Mantel– Haenszel test was used to compare the groups according to the preference of method. The Student’s t-test and ANOVA were used to compare quantitative independent variables and qualitative outcomes when the data were parametric. The Mann–Whitney or Kruskal–Wallis tests were used for non-parametric data.
The level of significance was set at 5% (P<0.05). The data were entered in an Excel spreadsheet and analyzed using the SPSS software version 20.
Results
The intervention studies for the prevention of prematurity included 123 pregnant women with a short cervix (twin pregnancies, n=61; singleton pregnancies, n=62) and all pregnant women were selected and accepted to participate in the study period. There were no differences between the populations of singleton and twin pregnancies (Table 1).
| Characteristics | Singleton, N=62 (50.4%) | Twin, N=61 (49.6%) | |||||
|---|---|---|---|---|---|---|---|
| Pessary n=30 |
Progesterone n=32 |
P | Pessary n=17 |
P+P n=16 |
Ovules n=28 |
P | |
| Maternal | |||||||
| Age-years | 28.60 (7.4) | 26.41 (8.8) | 0.29 | 30 (5.1) | 27.2 (3.6) | 27.64 (5.3) | 0.21 |
| Lives with partner | 25 (83.3) | 23 (71.9) | 0.28 | 15 (88.2) | 13 (81.3) | 21 (75) | 0.60 |
| Study-years | 11 (9-11) | 11 (9-11) | 0.62 | 11 (10-13) | 11 (9-13) | 11 (11-12) | 0.94 |
| Paid work | 27 (90) | 26 (81.3) | 0.47 | 15 (88.2) | 13 (81.3) | 25 (92.6) | 0.37 |
| Working hours/day | 8 (8-12) | 10 (7-12) | 0.84 | 8 (8-10) | 10 (8-12) | 9 (7-10) | 0.36 |
| White | 16 (57.1) | 12 (42.9) | 0.28 | 8 (50) | 7 (46.7) | 13 (46.4) | 0.97 |
| Obstetrics | |||||||
| Nuliparous | 14 (46.7) | 15 (46.9) | 0.99 | 7 (41.2) | 7 (43.8) | 11 (39.3) | 0.96 |
| History of prematurity | 5 (38.5) | 7 (46.7) | 0.66 | 2 (20) | 2 (25) | 5 (29.4) | 0.89 |
| Previous treatment for prematurity | 0 | 3 (37.5) | 0.23 | NA | NA | NA | - |
| Planned pregnancy | 16 (53.3) | 13 (40.6) | 0.32 | 6 (35.3) | 5 (31.3) | 6 (21.4) | 0.54 |
| Desired pregnancy | 30 (100) | 31 (96.9) | 1.00 | 17 (100) | 16 (100) | 28 (100) | 0.26 |
| Gestational age, weeks | 22.86 (22.28-23.43) |
22.64 (22.07-23.14) |
0.25 | 24.28 (22.57-25.14) |
21.79 (18-24.5) |
24.14 (22.36-26.71) |
0.08 |
| Cervical length, mm | 20 (15.7-22) |
19.2 (14.45-21.40) |
0.67 | 19 (17.7-21.6) |
22.5 (18.7-25.3) |
18.75 (16.1-23) |
0.15 |
Note: Data have been expressed as number and percentage, Mean (SD), and Median (interquartile range); n=Absolute value; P=Significant difference; SD: Standard Deviation; P+P=Pessary and Progesterone; NA=Not Applicable (patients did not undergo the procedure).
Table 1: Characteristics of the population at study inclusion between the allocated groups.
As for the preferable method, women with singleton pregnancies preferred to use a pessary (53.2%); however, no significant difference (P=0.703) was observed compared to progesterone (46.8%). Women with twin pregnancies preferred P+P (60.7%), followed by ovules (26.2%), and a pessary (8%), with a significant difference in this choice (P<0.001, Table 2).
| Characteristics | Singleton, N=62 | Twin, N=60 | |||||
|---|---|---|---|---|---|---|---|
| Preferable method | Preferable method | ||||||
| Pessary n=33 (53.2%) |
Progesterone n=29 (46.8%) |
P 0.70 |
Pessary n=8 (13.1%) |
P+P n=37 (60.7%) |
Ovules n=16 (26.2%) |
P 0.001 |
|
| Maternal | |||||||
| Age, years | 26.94 (8.3) | 28.07 (8.1) | 25.88 (2.2) | 28.56 (5.3) | 28.56 (5.0) | 0.59 | |
| Lives with partner | 27 (81.8) | 21 (72.4) | 0.54 | 6 (75) | 30 (81.1) | 13 (81.3) | 0.90 |
| Study - years | 11 (8-11) | 11 (10-11) | 0.64 | 10 (9-13) | 11 (10-12) | 11 (11-13) | 0.89 |
| Paid work | 26 (78.8) | 27 (93.1) | 0.30 | 7 (87.5) | 31 (86.1) | 15 (93.7) | 0.97 |
| Working hours/day | 8 (8-12) | 8 (8-12) | 0.78 | 9 (9-10) | 9 (8-11) | 8 (8-10) | 0.02 |
| White | 19 (63.3) | 9 (34.6) | 0.60 | 4 (57.1) | 20 (54.1) | 4 (26.7) | 0.19 |
| Obstetrics | |||||||
| Nuliparous | 15 (45.5) | 14 (48.3) | 0.82 | 4 (50) | 14 (37.8) | 7 (43.8) | 0.81 |
| History of prematurity | 7 (53.8) | 5 (33.3) | 0.44 | 1 (25) | 6 (27.3) | 2 (22.2) | 1.00 |
| Previous treatment for prematurity | 2 (28.6) | 1 (16.7) | 1.00 | NA | NA | NA | |
| Planned pregnancy | 15 (45.5) | 14 (48.3) | 0.82 | 0 | 11 (29.7) | 6 (37.5) | 0.16 |
| Desired pregnancy | 33 (100) | 29 (96.6) | 0.47 | 7 (87.5) | 37 (100) | 16 (100) | 0.13 |
| Gestational age, weeks | 22.71 (22-23.14) |
22.71 (22.28-23.43) |
0.60 | 21.86 (19.72-23.93) |
24 (21.28-26.57) |
24.07 (22.43-25.43) |
1.62 |
| Cervical length, mm | 18 (14.4-21.7) |
20 (17-22.10) |
0.27 | 21.5 (18.85-24) |
19 (17.3-23) |
19.1 (17-24) |
0.96 |
Note: Data have been expressed as number and percentage, Mean (SD), and Median (interquartile range); n=Absolute value; P=Significant difference; SD: Standard Deviation; P+P=Pessary and Progesterone; NA=Not Applicable (patients did not undergo the procedure).
Table 2: Association of population characteristics regarding the preference of treatment method.
Table 2 shows the analysis of the association between the population characteristics and preference for a method of prematurity prevention. The only characteristic that showed a significant association with method preference was the higher number of working hours in women with twin pregnancies, who preferred the pessary and P+P than ovules, with nine hours (9-10 h), nine hours (8-11 h), and eight hours (8-10 h), respectively (P=0.02).
The analysis of the influence of maternal actions and knowledge about prematurity on preference for prematurity prevention methods, pregnant women with twins with prior knowledge of the pessary showed a significantly higher preference for the use of the pessary alone in relation to P+P (37.5% vs. 5.7%; P=0.04), and none of the patients chose ovules (Table 3).
| Variables | Singleton, N=62 | Twin, N=61 | |||||
|---|---|---|---|---|---|---|---|
| Pessary n=33 (53.2%) |
Progesterone n=29 (46.80%) |
P | Pessary n=8 (13.1%) |
P+P n=37 (60.70%) |
Ovules n=16 (26.20%) |
P | |
| Concern about prematurity | |||||||
| Low | 6 (18.2) | 2 (6.9) | 0.3 | 1 (12.5) | 0 (0) | 2 (12.5) | 0.14 |
| Moderate | 3 (9.1) | 1 (3.4) | 0 (0) | 2 (5.4) | 1 (6.3) | ||
| High | 24 (72.7) | 26 (89.7) | 7 (87.5) | 35 (94.6) | 13 (81.3) | ||
| Would use the treatment | |||||||
| Yes | 33 (100) | 29 (100) | NA | 8 (100) | 37 (100) | 15 (93.8) | 0.39 |
| No | NA | NA | 0 (0) | 0 (0) | 1 (6.3) | ||
| Knowledge of prematurity prevention methods | |||||||
| Pessary | 6 (18.8) | 2 (7.1) | 0.16 | 3 (37.5) | 2 (5.7) | 0 | 0.04 |
| Progesterone | 6 (18.8) | 11 (39.3) | 0 | 11 (31.4) | 5 (33.3) | ||
| None | 20 (62.5) | 15 (53.6) | 5 (62.5) | 22 (62.9) | 10 (66.7) | ||
| Concerns about side effects | |||||||
| Pessary in the fetus | |||||||
| Not at all/a little | 30 (90.9) | 23 (82.1) | 0.23 | 8 (100) | 33 (89.2) | 16 (100) | 0.44 |
| Moderately | 2 (6.1) | 5 (17.9) | 0 (0) | 4 (10.8) | 0 (0) | ||
| Very much/extremely | 1 (3.0) | 0 (0) | NA | NA | NA | ||
| Pessary in the pregnant woman | |||||||
| Not at all/a little | 30 (90.9) | 25 (86.2) | 0.7 | 8 (100) | 34 (91.9) | 16 (100) | 0.7 |
| Moderately | 3 (9.1) | 4 (13.8) | 0 (0) | 3 (8.1) | 0 (0) | ||
| Very much/extremely | NA | NA | NA | NA | NA | ||
| Progesterone in the fetus | |||||||
| Not at all/a little | 28 (84.8) | 29 (69) | 0.26 | 8 (100) | 29 (78.4) | 16 (100) | 0.07 |
| Moderately | 3 (9.1) | 7 (24.1) | 0 (0) | 8 (21.6) | 0 (0) | ||
| Very much/extremely | 2 (6.1) | 2 (6.9) | NA | NA | NA | ||
| Progesterone in the pregnant woman | |||||||
| Not at all/a little | 28 (84.8) | 20 (69) | 0.42 | 8 (100) | 29 (78.4) | 16 (100) | 0.07 |
| Moderately | 2 (6.1) | 8 (27.6) | 0 (0) | 8 (21.6) | 0 (0) | ||
| Very much/extremely | 3 (9.1) | 1 (3.4) | NA | NA | NA | ||
Note: Data have been expressed as number and percentage, Mean (SD); SD: Standard Deviation; n=Absolute value; P=Significant difference; P+P=Pessary and Progesterone; NA=Not Applicable (patients did not undergo the procedure).
Table 3: Influence of maternal actions and knowledge about prematurity on the preference for prematurity prevention methods.
Table 4 shows the evaluation of the association between the anxiety scores (state and trait) and QoL in relation to the preference for prematurity prevention method. Women pregnant with twins with a moderate and high level of trait anxiety had a significantly greater preference (P=0.02) for the pessary alone (87.5%) and P+P (100%) than for ovules (60%).
As for the QoL, singleton pregnancies showed a significant difference in the environment domain (Table 4). Patients who opted for progesterone had lower scores compared to those who preferred the pessary (57.81 vs. 71.43; P=0.007).
| Variables | Singleton, N=60 | Twin, N=59 | |||||
|---|---|---|---|---|---|---|---|
| Pessary n=33 |
Progesterone n=27 |
P | Pessary n=8 |
P+P n=36 |
Ovules n=15 |
P | |
| State anxiety | |||||||
| Low | NA | NA | 0.16 | 0 | 0 | 2 (12.5) | 0.21 |
| Moderate | 23 (69.7) | 14 (51.9) | 4 (57.1) | 21 (60) | 10 (62.5) | ||
| High | 10 (30.3) | 13 (48.1) | 3 (42.9) | 14 (40) | 4 (25) | ||
| Trait anxiety | |||||||
| Low | 5 (15.6) | 0 (0.0) | 0.11 | 1 (12.5) | 0 (0.0) | 6 (40) | 0.002 |
| Moderate | 20 (6.5) | 20 (74.1) | 5 (62.5) | 27 (75) | 7 (46.7) | ||
| High | 7 (21.9) | 7 (25.9) | 2 (25) | 9 (25) | 2 (13.3) | ||
| QoL | |||||||
| General QoL | 4 (4-5) | 4 (4-4) | 0.07 | 4 (3-4) | 4 (4-4) | 4 (4-5) | 0.27 |
| Pregnancy satisfaction | 5 (4-5) | 5 (4-5) | 0.28 | 5 (3-5) | 4 (4-5) | 5 (4-5) | 0.45 |
| Physical domain | 62.5 (53.57-73.21) | 57.14 (50-67.86) | 0.17 | 57.14 (41.07-75) | 50 (46.43-64.29) | 58.93 (46.43-71.43) | 0.45 |
| Psychological domain | 70.83 (62.50) | 70.83 (55-79.17) | 0.33 | 72.92 (62.50-77.08) | 70.83 (58.33-79.17) | 79.17 (66.67-85.42) | 0.14 |
| Environment domain | 71.43 (62.50-75) | 57.81 (48.44-68.75) | 0.007 | 62.50 (53.13-70.31) | 66.67 (56.25-83.33) | 64.06 (53.13-68.75) | 0.96 |
| Social Relations domain | 75 (66.67-91.67) | 75 (70.83-75) | 0.28 | 83.33 (58.33-95.83) | 60.94 (56.25-75) | 79.17 (66.67-100) | 0.23 |
Note: Data have been expressed as number and percentage, Mean (SD), and Median (interquartile range); n=Absolute value; P=Significant difference; SD: Standard Deviation; P+P=Pessary and Progesterone; NA=Not Applicable (patients did not undergo the procedure).
Table 4: Trait anxiety, state anxiety, and QoL scores in relation to the preference for the method of prematurity prevention.
Discussion
Main findings of the study
The results of this prospective single-center study with women pregnant with singletons and twins with a real risk of prematurity first demonstrated that women pregnant with twins showed a greater preference for the use of P+P than ovules and pessary alone; while women pregnant with singletons showed no differences between pessary and progesterone treatments. Second, the group of women pregnant with twins with the highest number of hours worked per day showed a greater preference for P+P. Third, the knowledge of prematurity prevention methods influenced the choice of treatment in twin pregnancies, but not in singleton pregnancies. Previous knowledge of the pessary in twin pregnancies resulted in a greater choice for this method. Fourth, women pregnant with twins with higher trait anxiety scores preferred to use P+P. Finally, in singleton pregnancies, lower scores in the environment domain of QoL are associated with a preference for progesterone.
Comparison with the results of previous studies
The absence of differences in the preferences of methods between singleton mothers can be attributed to the information provided to them regarding the effectiveness of the pessary and progesterone to prevent prematurity in singleton pregnancies, since they were informed that both methods were effective in reducing the prematurity. They were also informed that the study was being conducted to assess whether there was a difference in the effectiveness between the two methods [3].
The highest preference for the P+P method in the group of twin pregnancies was probably due to the lack of a treatment method with proven efficacy for this type of pregnancy, since studies are still controversial [4]. Twin pregnancies are at a greater risk of prematurity and associated comorbidities that trigger preterm birth and fetal death [12]. This may have contributed to the choice of the P+P method, which increased the safety of these pregnant women. Another factor that may have contributed to the preference for the P+P method in twin pregnancies was the number of hours worked per day, since a longer working day results in lesser rest and a greater risk of preterm birth. However, the influence of previous knowledge on the use of a pessary in twin pregnancies resulted in a preference for the pessary over the P+P or ovule methods, probably because there is still no effective method for these pregnancies, resulting in the choice of a method already known by the patients.
Another factor influencing the choice of a method for a given treatment is the anxiety level of the patient. Estimates show that 20% of women experience anxiety symptoms during pregnancy, which can negatively affect the pregnancy for being a mediator of endocrine changes, also increasing the risk of prematurity [13]. In addition, several pregnancy adaptations increase the vulnerability of women to the onset of anxiety disorders [14]. A previous study evaluating trait and state anxiety levels in pregnant women at risk of preterm birth using the STAI reported significantly high levels, with 73.6% of the patients presenting a high level of state anxiety and 69.8% presenting a high level of trait anxiety [15]. The present study showed that higher trait anxiety scores in twin pregnancies resulted in a greater preference for pessary alone and P+P compared to ovules. Trait anxiety refers to individual and relatively stable differences of an individual and how they react to situations; thus, methods, such as the pessary convey greater safety and QoL, influencing the preference of these patients [10]. This was observed in a study involving 166 pregnant women at the risk of prematurity in which the experience of using a pessary resulted in 77.1% of them reporting better QoL, with 75.3% reporting that their expectations were exceeded and 91.6% reporting that they would choose the pessary again or recommend it to another woman in a similar situation. The study also reported that the positive changes during the pessary treatment seemed to be related to a decreased concern about the risk of premature birth and to the relief of intrauterine pressure during daily activities [16].
The QoL may also play a role in the choice of treatment methods, particularly in cases of increased gestational risk resulting in unfavorable outcomes for both mother and fetus [17,18]. In singleton pregnancies, patients with a preference for the pessary over progesterone had higher scores in the environment domain. The environment domain concerns safety, health of the physical environment, financial life, information level, leisure, housing conditions, and access to health services, and means of transport [19]. Thus, a better socioeconomic level and knowledge about the method may be associated with the choice of the pessary, reflecting greater security perception with this method. The use of a QoL instrument helped identify the life domain or dimension that had a more positive or negative evaluation from the perspective of the pregnant woman and how it can influence the patients’ decisions [19]. The present study showed a generally good QoL, which did not result in significant differences regarding the choices of methods.
Implications for clinical practice or research contributions
This study identified some aspects that may influence the preference of a pregnant woman at real risk of prematurity for a particular treatment method and how this may favor a more comprehensive approach. Understanding the particularities of patients’ choices will help direct clinical practices toward better adherence and results during pregnancy, and promoting greater maternal and fetal well-being.
Strengths and limitations
The strength of this study lies in its design, being a prospective study with pregnant women at real risk of prematurity and the use of simple questionnaires answered in person at the time of the risk. The lack of widespread knowledge of the patients about prematurity prevention methods may have increased the difficulty when choosing the methods, making it impossible to accurately relate the factors associated with the patient’s preference. Other factors that may have contributed to these results may have been the number of treatment groups studied and the fact that the study was conducted at a single center with a single socioeconomic profile of patients.
Conclusion
Unlike some previous studies on prematurity treatment preferences, in which the patients were not at real risk of prematurity, the present study included pregnant women with a short cervix, demonstrating an important aspect for the treatment. In addition, the study identified no preferences between the use of cervical pessary and progesterone in singleton pregnancies, since both treatments were already proven effective, allowing patients to choose the treatment that best suits their daily lives. In twin pregnancies, there was a higher preference for the P+P method, in part due to the lack of proven efficacy for this type of pregnancy and prior knowledge of the pessary by twin pregnant women. Factors, such as the working time, degree of trait anxiety, and prior knowledge about a certain method influenced the choices in twin pregnancies, while lower scores in the environment domain of QoL played a role in singleton pregnancies.
Although the results of this research cannot be generalized, they can contribute to the understanding of certain individual characteristics occasionally not considered important by the health team.
Declaration
Statement of ethics
This study was performed in line with the principles of the Declaration of Helsinki. Ethical approval for this study was obtained from Hospital das Clínicas da Faculdade de Medicina de São Paulo (HCFMUSP) Research Ethics Committee (CAAE:15278819.0.0000.0068). All participants provided written informed consent. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not Applicable
Availability of data and materials
The datasets are not publicly available due to the hospital policy and personal privacy but are available from the corresponding author on reasonable request.
Conflict of Interest
The authors have no conflicts of interest to declare.
Funding
This study received no funding.
Authors’ Contributions
Study concept and design: SAFCP and MLB. Data collection: SAFCP, CLMP, and JCM. Data analysis and interpretation: SAFCP, MLB, MHB, and SV. Article preparation and approval for submission: SAFCP, MLB, MHB, SEBG, UTG, and RP.
Acknowledgement
We would like to thank the patients who participated in this study and the prenatal team at the HCFMUSP that supported the research.
References
- Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371(9606):75-84.
[Crossref] [Google Scholar] [PubMed]
- Unified Health System (SUS). 2003.
- Romero R, Nicolaides KH, Conde-Agudelo A, O'Brien JM, Cetingoz E, Da Fonseca E, et al. Vaginal progesterone decreases preterm birth ≤ 34 weeks of gestation in women with a singleton pregnancy and a short cervix: An updated meta-analysis including data from the OPPTIMUM study. Ultrasound Obstet Gynecol. 2016;48:308-317.
[Crossref] [Google Scholar] [PubMed]
- Goya M, Pratcorona L, Merced C, Rodó C, Valle L, Romero A, et al. Cervical pessary in pregnant women with a short cervix (PECEP): An open-label randomised controlled trial. Lancet. 2012;379(9828):1800-1806.
[Crossref] [Google Scholar] [PubMed]
- van der Ven AJ, van Os M, van den Wijngaard L, Mochtar MH, de Bekker-Grob EW, Kazemier BM. Patient’s preferences for management options in relation to preterm birth. J Health Med Informat. 2015;6(3):189.
- Ha V, McDonald SD. Pregnant women’s preferences for and concerns about preterm birth prevention: A cross-sectional survey. BMC Pregnancy Childbirth. 2017;17(1):49.
[Crossref] [Google Scholar] [PubMed]
- Likert R. A technique for the measurement of attitudes. Archives of Psychology. 1932;22(140):1-55.
- WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28(3):551-558.
[Crossref] [Google Scholar] [PubMed]
- Fleck M, Louzada S, Xavier M, Chachamovich E, Vieira G, Santos L, et al. Application of the Portuguese version of the abbreviated instrument of quality life WHOQOL-bref. Rev Saúde Pública. 2000;34 (2):178-183.
[Crossref] [Google Scholar] [PubMed]
- Biaggio A, Natalicio LF, Spielberger CD. Desenvolvimento da forma experimental em português do Inventário de Ansiedade Traço-Estado (IDATE). Arquivos Brasileiros de Psicologia Aplicada. 1977;29(3):33-44.
- Spielberger CD, Gorsuch RL, Lushene RE. Manual for the state-trait anxiety inventory. Consulting Psychologist Press, Palo Alto. 1970.
- Thorpe K, Golding J, MacGillivray I, Greenwood R. Comparison of prevalence of depression in mothers of twins and mothers of singletons. BMJ. 1991;302(6781), 875-878.
[Crossref] [Google Scholar] [PubMed]
- Correia LL, Linhares MBM. Maternal anxiety in the pre- and postnatal period: A literature review. Rev Lat Am Enfermagem. 2007;15(4):677-683.
[Crossref] [Google Scholar] [PubMed]
- Ferrari AG, Donelli TMS. Tornar-se mãe e prematuridade: Considerações sobre a constituição da maternidade no contexto do nascimento de um bebê com muito baixo peso. Contextos Clínicos. 2010;3(2):106-112.
- Duarte EG. Avaliação da ansiedade nas gestantes de risco para o parto prematuro por meio do inventário IDATE. 2013.
- Seravalli V, Strambi N, D'Arienzo A, Magni F, Bernardi L, Morucchio A, et al. Patient’s experience with the Arabin cervical pessary during pregnancy: A questionnaire survey. PLoS One. 2022;17(1):e0261830.
[Crossref] [Google Scholar] [PubMed]
- Gadelha IP, Aquino PS, Balsells MMD, Diniz FF, Pinheiro AKB, Ribeiro SG, et al. Quality of life of high risk pregnant women during prenatal care. Rev Bras Enferm. 2020;73(Suppl 5):e20190595.
[Crossref] [Google Scholar] [PubMed]
- Ananth CV, Vintzillos AM. Epidemiology of preterm birth and its clinical subtypes. J Matern Fetal Neonatal Med. 2006;19:73-82.
[Crossref] [Google Scholar] [PubMed]
- Castro DFA. Qualidade de vida de gestantes assistidas pela estratégia saúde da família [dissertação]. Universidade de São Paulo. 2010.
Citation: Perrusi SDAFC, Brizot MDL, Garavazzo SEB, Pucci CLM, Gomez UT, Peres SV, et al. (2023) Evaluation of Patient Preferences for Treatments to Prevent Preterm Births in Singleton and Twin Pregnancies with a Short Cervix. Clinics Mother Child Health. S17:001.
Copyright: © 2023 Perrusi SDAFC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

