Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- The Global Impact Factor (GIF)
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
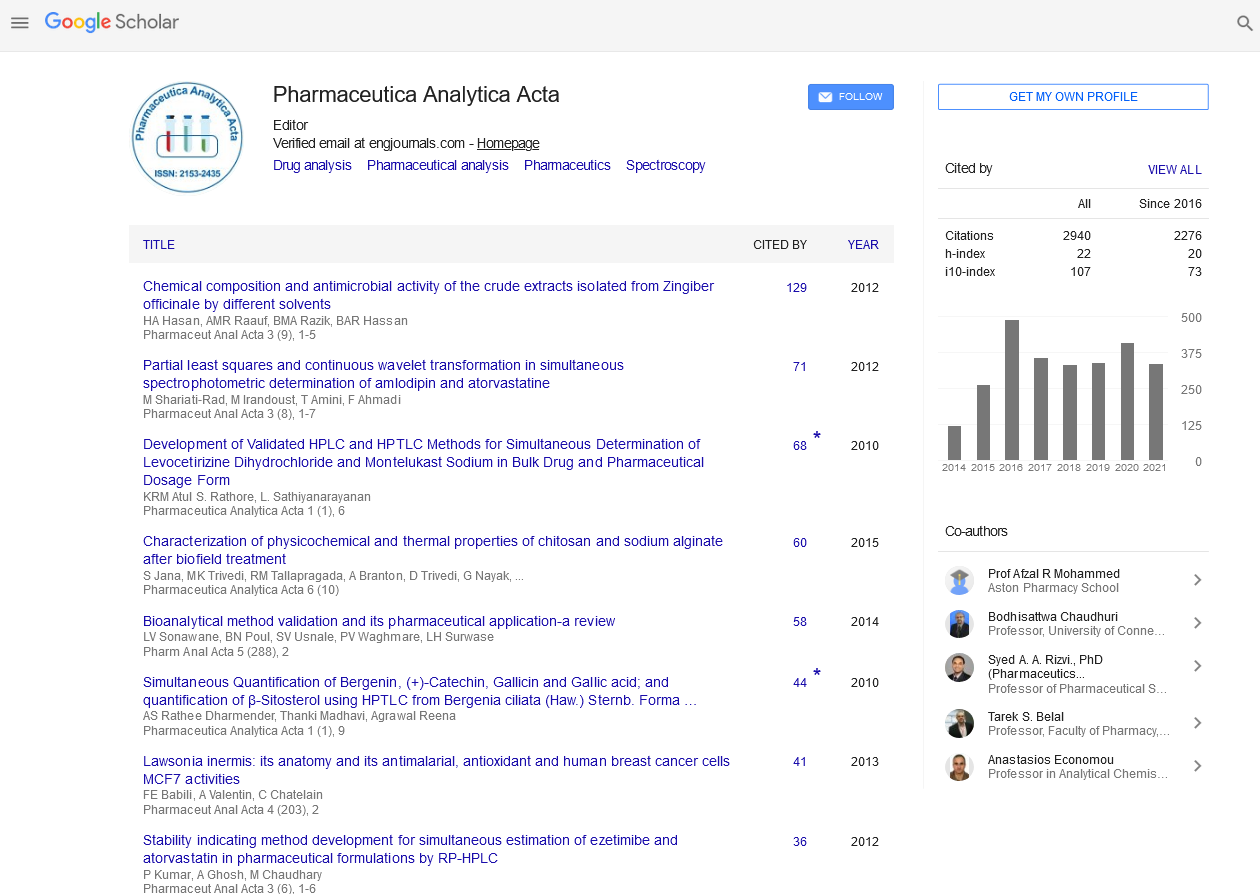
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion Article - (2022) Volume 13, Issue 3
Drug Resistance Markers within an Evolving Efficacy
Elis Haan*Received: 01-Mar-2022, Manuscript No. PAA-22-16450; Editor assigned: 04-Mar-2022, Pre QC No. PAA-22-16450(PQ); Reviewed: 18-Mar-2022, QC No. PAA-22-16450; Revised: 25-Mar-2022, Manuscript No. PAA-22-16450(R); Published: 01-Apr-2022, DOI: 10.4172/ 2153-2435.22.13.665
Description
The rapid development and dispersal of mutations associated with anti-malarial drug resistance influenced policy changes the away from the use of chloroquine, amodiaquine, and sulphadoxine-pyrimethamine in the treatment of uncomplicated falciparum malaria and toward the use of Artemisininbased Combination Therapies (ACTs). However, the influence of medication policy changes on the evolution of Plasmodium falciparum resistance genetic markers in Cameroon is still unknown. As a result, the goal of this systematic review and meta-analysis is to determine the prevalence and distribution of P. falciparum drug resistance markers in the context of antimalarial medication efficacy that is changing.
Malaria caused 228 million infections and 405,000 deaths worldwide in 2018, according to WHO statistics. Despite massive attempts to manage the disease, Cameroon continues to have a high malaria burden and effect. Between 2002 and 2004, the rapid emergence and spread of drug resistance in Cameroon caused the use of chloroquine (CQ) as the first-line therapy for uncomplicated Plasmodium falciparum malaria to be replaced by amodiaquine (AQ) monotherapy and sulphadoxinepyrimethamine (SP).
In 2004, the government of Cameroon made a significant pharmacological policy shift by adopting artesunateamodiaquine (ASAQ) and later Artemether-Lumefantrine (AL) as first-line therapies for uncomplicated malaria, as recommended by the World Health Organization (WHO). In public health facilities, ASAQ and AL medicines are distributed in proportions of 75 percent and 25 percent, respectively. The AL combination is rather common among private health care facilities and vendors. The presence or absence of parasites resistant to anti-malarial medications in the population determines their efficacy. As a result, malaria control programmes in endemic areas rely heavily on regular monitoring of drug resistance markers.
Malaria can be efficiently prevented and cured when antimalarial medications are used. The rapid development and distribution of drug resistance markers forced the Cameroon government to switch from immunotherapies based combination therapies in the early 2000s, in accordance with WHO recommendations. Trend analyses have shown the fall of the Pfcrt 76T mutant during the years since the use of Chroroquine was banned in many malaria-endemic countries, confirming the re-emergence of Chloroquine-sensitive to treat parasites. Furthermore, numerous investigations have shown that the Pfmdr1 YYY triple haplotype for ASAQ and Pfmdr1 NFD triple haplotype for AL have opposing effects. When both medications are used at the same time, this may help to delay the establishment of drug resistance.
The main goal of this review is to find and describe molecular markers that confer treatment resistance in Plasmodium falciparum parasites that have been circulating in Cameroon for more than 20 years. Data from previously published and unpublished investigations on anti-malarial medication resistance gene alterations will be pooled for this review. This will offer proof that ACTs can be used in the treatment of uncomplicated P. falciparum malaria indefinitely. Furthermore, the study's findings will be utilized as a starting point for the development and implementation of a worldwide anti-malarial medication resistance surveillance system, which currently does not exist.
Citation: Haan E (2022) Drug Resistance Markers within an Evolving Efficacy. Pharm Anal Acta. 13:665.
Copyright: © 2022 Haan E. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.