Indexed In
- Open J Gate
- Genamics JournalSeek
- CiteFactor
- Cosmos IF
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Proquest Summons
- Scholarsteer
- ROAD
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2025) Volume 17, Issue 7
Delay in Return to Fertility after Discontinuation of Using Depo-Provera and Associated Factors among Currently Pregnant Women Attending Antenatal Care in Public Health Facilities in Gindeberet District, Oromia, Ethiopia, 2021: Facility based Cross Sectional Study
Tilahun Negero Tolera1*, Andinet Tesema Kubela2 and Gadisa Fitala Obssie22Department of Public Health, Dambi Dollo University, Dambi Dollo Town, Ethiopia
Received: 29-Jul-2024, Manuscript No. BLM-24-26613; Editor assigned: 01-Aug-2024, Pre QC No. BLM-24-26613 (PQ); Reviewed: 15-Aug-2024, QC No. BLM-24-26613; Revised: 15-Jun-2025, Manuscript No. BLM-24-26613 (R); Published: 23-Jun-2025, DOI: 10.35248/0974-8369.25.17.780
Abstract
Background: One of the of methods to control fertility is use of injectable depo-provera which has the side effect of delaying return to fertility after discontinuation of it. Delay of fertility return after the method termination remains a major concern for women who use it. This fear poses a negative impact on utilization and continuation of depoprovera in developing nations including Ethiopia. Therefore, determining the median delay of fertility return after discontinuation of depo-provera and identifying the associating factors are important for developing solutions to the issues of clients and health care providers.
Objective: To assess delay in fertility return after discontinuation depo-provera and associated factors among pregnant women attending ANC in public health facilities in Gindeberet district, Oromia, Ethiopia, 2021. Materials and methods: Facility based cross sectional study was conducted on 415 pregnant women attending antenatal care in public health facilities in Gindeberet district from August 10-October 10/2021. Consecutive sampling technique was used. Pretested structured interviewer-administered questionnaire was used to collect data. Data were entered into Epi info version 7 and then exported to SPSS version 25 for cleaning, analysis and summarized using descriptive statistics of frequencies and median. Bi-variate and multi-variable logistic regression was applied to estimate the crude and adjusted odds ratios with 95% CI to determine the presence and strength of association and P-value<0.05 as cut off point.
Result: The median delay of fertility return in this study was found to be 10 months from date of depo-provera discontinuation. The magnitude of fertility delay in this study was 45.5% (95% CI=38.4%, 52.6%). Multivariable analysis showed that being lower income ≤ 2500 ETB (AOR: 0.09 (0.042, 0.21)), age group from 15-24 years (AOR: 0.04 (0.006, 0.23)), age group from 30-34 years AOR: (0.23 (0.083, 0.66)), age at first sex 19-23 years (AOR: 0.4 (0.17, 0.93)), being sexually active 1 day/week (AOR: 5.5 (1.4, 20.8)) sexually active 2-3 days/week (AOR: 4.2 (1.7, 14.9)) had significant association with delay in return to fertility after discontinuation of using depo-provera.
Conclusion and recommendation: After discontinuation of depo-provera there is significant delay in return to fertility. Therefore, women should be counseled that there is a potential for delay in return to fertility following discontinuation of the method. Being older age, being higher income, infrequent sexual intercourse and delayed age at first sex were predictors of fertility delay after discontinuation of depo-provera.
Keywords
Fertility return; Depo-Provera; Ginde beret; Ethiopia
Introduction
Contraceptive injection is a contraceptive in the form of a liquid that is injected into a woman's body, which contains hormones and then it is absorbed into the blood vessels little by little by the body, which is useful for preventing pregnancy. Progestinonly injectable contraceptives come in two varieties: Those containing Depot Medroxy Progesterone Acetate (DMPA) and those containing Norethisterone Ethanate (NET-EN) [1].
Globally according to World Health Organization report around 922 million people use injectable contraceptives accounting for about 45% of all family planning consumers. Injection-based methods differ from other methods in the return to fertility since they are irreversible in the short-term. The most commonly used progestin-only injectable, DMPA is convenient and reversible for most women and adolescent girls of reproductive age. Compared to other progestin-only contraceptives, DMPA contains substantially higher levels of progestin [2].
Researchers discovered that women who used DMPA contraception had a 20-fold higher risk of delay in fertility return after method discontinuation than women who used other long-acting reversible contraception in a massive prospective cohort study done in United states. Except for tubal ligation in females and vasectomy in males, no family planning method causes permanent infertility. Almost all short-term family planning methods, with the exception of depo-provera method, immediately return to fertility following discontinuation of usage is common [3].
Globally according to previously conducted studies the 12-month life-table discontinuation rate due to these side effects was 58%, with half of those who stopped after one injection. The study of the factors of drop out of DMPA injections in Indonesia discovered that they want to conceive or have children right away 35.13% and that the negative side effects like delay in return to fertility after method discountution is the reason for their abandonment. Medroxyprogesterone Acetate (MPA) tends to persist in the bloodstream and prevent ovulation for several months after DMPA administration is stopped [4].
Different reports indicate that there is a variable delay in the resumption of menstruation, ovulation and fertility after DMPA is discontinued. As a result some countries, such as Thailand, restrict the use of DMPA for birth spacing to women who already have two living children. Cohort studies on women discontinued the regimen of 150 mg at 3 months’ interval reported that about one-half to twothirds resumed fertility within 6 months of last injection of MPA and at least three-quarter resumed fertility within one year. Thus this study was intended to assess the duration of fertility return after discontinuation of depo-provera, as well as the factors that influence the delay in return to fertility among pregnant women attending ANC in public health facilities in Gindeberet district [5].
Materials and Methods
Study area and period
The study was conducted from August 10/2021 to October 10/2021 in Ginde Beret district public health facilities. Ginde Beret district is one of the districts in West Shoa zone Oromia region, Ethiopia. The district is located 193 kilometers from Addis Ababa toward North-west. The district is administratively divided into 33 kebele (smallest administrative unit), 3 urban and 30 rural. The district is bordered on the south by Jeldu, on the Southwest by Ambo district, on the west by the Guder River which separates it from the Horo Guduru Wollega zone, on the north by the Abay River which separates it from the Amhara Region, on the east by Abuna Ginde Beret district [6].
According to Ginde Beret district Health office, the district's population in 2021 was projected to be 159,016 (80,557 males and 78,459 females). There is one public hospital, six public health centers and thirty-three health posts in the district. Family planning services are available in all public health facilities in the district. The total numbers of reproductive age group in the district were 35,190 of them depo-provera users were 14,428 [7].
Study design
Facility based cross-sectional study was conducted in public health facilities of Gindeberet district, Oromia, Ethiopia.
Population
Source population: All pregnant women who were using DMPA before current pregnancy, attending ANC at public health facilities in Gindeberet district.
Study population: All pregnant women who were using DMPA before current pregnancy, attending ANC at public health facilities in Gindeberet district during the study period [8].
Inclusion and exclusion criteria
Inclusion criteria: Women who meet the following criteria were chosen as appropriate study participants.
- Used DMPA at least single injection prior to discontinuation
- Stated an expressed intention to become pregnant as the reason for discontinuation.
- Did not used any form of birth control (male or female) after discontinuation of DMPA.
- Married or living with her husband or sexual partner (having regular intercourse to become pregnant).
Exclusion criteria: Pregnant women, who used DMPA but became pregnant due to a method failure, as well as pregnant women who were seriously ill and unable to communicate were excluded. Women who were less than 18 years were not included in the study because of difficulties to get informed consent [9].
Sample size determination and sampling technique
Sample size determination: Sample size calculation for objective one sample size was calculated using single population proportion formula taking into account that 45.9% of women had delayed fertility return after discontinuing DMPA use (based on previous study conducted in Addis Ababa). Using 5% margin of error, and a 95% confidence level (d=0.05). Based on this assumption the actual sample sizes for the study was n=(Z α/2)2 (P (1-P)/d2 [10].
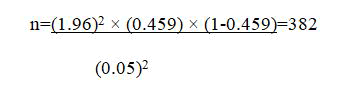
By considering 10% for non-response rate i.e., 38 and the final sample size was 420.
Where; n=the required sample size
p=Proportion of women delayed return to fertility after discontinuation of using DMPA
Z α/2=the value of Z in a standard normal distribution (95% confidence level corresponding to alpha level of 0.05 which is equal to 1.96)
d=the Margin of error between the sample and the population (0.05)
Sample size calculation for the second objective: Variable which has strong association with delay in fertility return from study conducted at Addis Ababa was selected, at 95% of confidence level, at 80% of power, ratio of unexposed to exposed [10].
In which, the maximum sample size was taken (n=420) from objective one.
Sampling technique: The study was conducted in all seven public health facilities found in Gindeberet district. In all health facilities, the numbers of women who have stopped DMPA in the past two years were 2405 and the required numbers of sample was allocated proportionally based on their respective number of clients who discontinued DMPA in each health facility. Since the number of women who had used DMPA and currently pregnant were limited, all eligible participants were recruited as they come to health facilities based on the inclusion criteria until required number was meet and consecutive sampling technique was used to select study subjects. Study participants were chosen using the following formula based on proportional allocation for each health facility:
n=nf × N Depo-Provera discontinued in respective health facility/N total
n=sample size in their respective health facility
nf=n1+n2+n3+n4+n5+n6+n7 estimated final sample size
N total=N1+N2…. (Numbers women who discontinued DMPA in each health facility
Variables
Dependent variable: Delay in fertility return after discountution of DMPA
Independent variables
Socio demographic characteristics: Age, family income, years stayed in marriage.
Reproductive variables: Gravidity, sexual frequency, age at first sex, previous utilization of contraception.
DMPA related factor: Number of DMPA used in cycles.
Operational definition
Return of fertility after discontinuation of DMPA: Defined as the establishment of a proven pregnancy later than 15 weeks following the last 3-month injection (the assumed normal protection period of 12 weeks plus an arbitrarily defined and clinically valid safety-period of 3 weeks [11].
Delay in fertility return after discontinuation of using DMPA: Resumption of fertility after 10 months of discontinuation of using DMPA while having regular sexual intercourse.
Not delay in fertility return after discontinuation of using DMPA: Resumption of fertility at or before 10 months after discontinuation of using DMPA while having regular sexual intercourse.
Regular sexual intercourse: Sexually active at least once per week with couple or sexual partner.
Fertility returns to current pregnancy: Obtained from duration of current pregnancy estimated by U/S or GA on the day of data collection date minus date of depo-provera discontinuation [12].
Date of depo-provera discontinuation: Calculated from the last date of depo-provera injection protection period of 12 weeks plus clinically valid safety-period of 3 weeks while not using any contraception method [13].
Data collection tool and techniques
An interviewer-administered structured questionnaire with reviewing client’s record was used to collect the data. The questionnaire was adapted to the local situation and the study area from previously conducted studies to fit to the purpose of the study. The domains of questions included in the tool were socio-demographic characteristics, reproductive characteristics and depo-provera related characteristics. The questionnaire was first prepared in English and then translated into Afan Oromo by language expert. The questionnaire was translated back into English by another language expert in order to check if the translation was consistent with the English version. Finally, Afan Oromo questionnaire was administered by seven trained female midwives who were working in the health facilities with close follow-up of one supervisor. In addition, the participants were interviewed after they completed their follow up visit as an exit interview.
Data quality assurance
Both the data collectors and the supervisor were trained for one day on the purpose, sampling technique, ethical concerns, data collection tools and the data collection process in order to ensure the quality of data. In the entire data collection period, the investigator supervised them and the collected data were examined for completeness every two days by the supervisor. Incomplete questionnaires were excluded from further analysis. The questionnaire was pretested on 5% of the sample size (21 women) in Bake Kelate Health Centre, Abuna Gindeberet prior to the actual data collection. Some modifications were made on the questionnaire based on the findings of the pretest. Also, the reliability of the tool was tested with Cronbach’s alpha coefficient and it was found 0.83 [14].
Data processing and analysis
After data collection, each questionnaire was checked for its completeness and the data were coded and entered using Epiinfo version 7 and exported to the Statistical Package for Social Sciences (SPSS) version 25 to be cleaned and analyzed by the investigator. Descriptive statistics were calculated and summarized using frequencies and median. The delay in return to fertility after discontinuation of using DMPA was dichotomized using the median months of delay in return to fertility as a threshold.
Then, the description of study participants by their different socio-demographic, reproductive health characteristics and depoprovera related characteristics were presented using tables, chart and text. Bivariate and multivariable logistic regressions were applied to analyze the association between the dependent and independent variables. Variables with p-value<0.2 with COR on bivariate logistic regression were considered as candidates for multivariable logistic regression. Model fitness was checked through Hosmer-Lemeshow goodness of fit test and it was fitted. Multi-collinearity test was done and no multi-collinearity was found. In multivariable analysis, the association between independent variables and the outcome variable was measured using AOR, 95% CI and PV<0.05 were considered as statistically significant [15].
Results
Socio-demographic characteristics
In this study 415 pregnant women attending ANC participated which made the response rate of 98.8%. The median age of the respondents was 28 years and 406 (97.8%) respondents were married (in union). Regarding the educational status of respondents, about 255 (61.4%) were attained primary education, followed by secondary and above 91 (21.9%) in their educational status. Regarding the occupation status of respondents about 260 (62.7%) were engaged in farming, followed by private employees 66 (15.9%).
Reproductive characteristics of the respondents
Regarding the age at first sex of the respondents, the minimum age at first sex was 16 years and maximum was 31 years. Concerning years lived in marriage, majority 306 (73.3%) of the respondents were married for less than or equal to nine years. Among mothers interviewed majority 298 (71.8%) had ever given birth. Regarding weekly sexual intercourse frequency before current pregnancy majority 250 (60.2%) were sexually active 2-3 days per week to become pregnant [16].
Depo-provera related characteristics
The median delay of fertility return in this study was found to be 10 months from date of depo-provera discontinuation. Majority 262 (63.1%) of the respondent did not used any modern FP methods before using depo-provera. About 386 (93%) of study women have been on depo-provera for a period of less than five cycle. Majority 329 (79.3%) of the women were not told about side effect of depo-provera concerning delay in return to fertility after discontinuation of using it. The magnitude of fertility delay in this study was 45.5% (95% CI=38.4.4%, 52.6%).
Factors associated with delay in return to fertility after discontinuation of DMPA
In this study to measure factors associated with delay of fertility return after discontinuation of using depo-provera bivariate and multivariable logistic regressions were conducted and associated factors for delay of fertility return after discontinuation of using depo-provera were analyzed as below.
Bivariate analysis
To measure the association between delay of fertility return after discontinuation of using depo-provera and factors associated with delay of fertility return after discontinuation of using depoprovera binary logistic regression was conducted. The result of the bivariate analysis showed that being in age group from 25-29 year (COR: 3.88 (1.93, 7.81)), age group from 30-34 year (COR: 12.7 (6.2, 26.1)) and age group ≥ 35 year (COR: 104 (39.9, 273)), being in lower income ≤ 2500 ETB (COR: 8.5 (4.7, 15.1)) age at first sex ≤ 18 years (COR: 29.4 (14, 61.8)), age at first sex from 19-23 years (COR: 3.61 (1.97, 6.6)), being nulliparous (COR: 8.74: (4.91, 15.5)), being not previous user modern FP (COR: 3.06 (2.02, 4.63)), being stayed in marriage for ≤ 9 years [7.91 (4.7, 13.4)], being sexually active 1 day/week (COR: 25.5 (8.44, 77.0)), being sexually active 2-3 days/week (COR: 5.6 (1.93, 16.1)) were significantly associated with delay in return to fertility after discontinuation of using depo-provera at pv<0.2 with 95% CI [17].
Multivariable analysis
In the bivariate analysis variables those showed p-value<0.2 were transferred in to multivariable logistic regression analysis to control confounding variables and test the association of independent variables with the dependent variable. Multivariate logistic regression was done among all significant factors on binary logistic regression which were age group, monthly family income, age at first sex and weekly sexual intercourse of respondents were significantly associated with delay in return to fertility after discontinuation of DMPA [18].
Based on the result of multivariable logistic regression analysis showed respondents who were from lower family income were 91% times less likely delay in return to fertility after discontinuation of DMPA compared to higher income (AOR: 0.09 (0.042, 0.21)), age group from 15-24 years were 96% less likely delay in return to fertility after discontinuation of DMPA compared to age group ≥ 35 years (AOR: 0.04 (0.006, 0.23)) and age group from 25-29 years were 85% less likely delay in return to fertility after discontinuation of DMPA compared to age group ≥ 35 years (AOR: 0.15 (0.042, 0.55)), age group from 30-34 years were 77% less likely delay in return to fertility after discontinuation of depo-provera compared to age group ≥ 35 years (AOR: 0.23 (0.083, 0.66)), respondent with age at first sex from 19-23 years were 61% less likely delay in return to fertility after discontinuation of DMPA compared to age at first sex ≥ 24 years (AOR: 0.39 (0.16, 0.93)), women who were sexually active 1 day per week were 5.5 more likely delay in return to fertility after discontinuation of DMPA compared to women were sexually active ≥ 4 days/week (AOR: 5.5 (1.45, 20.8)), women who were sexually active 2-3 days/week were 4.2 more likely delay in return to fertility after discontinuation of DMPA compared to women were sexually active ≥ 4 days/week (AOR: 4.2 (1.17, 14.99)) all these variables had significant association with delay in return to fertility after discontinuation of using depo-provera (Figure 1) [19].
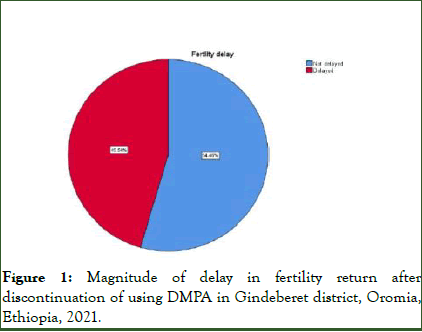
Figure 1: Magnitude of delay in fertility return after discontinuation of using DMPA in Gindeberet district, Oromia, Ethiopia, 2021.
Discussion
The study showed that 45.5% of the participants had fertility delay after discontinuation of DMPA. This result was slightly lower than study conducted in Addis Ababa which was 45.9%. The discrepancy might be due to socio-economic status difference of study population. The finding of this study demonstrated that depo-provera users had significant delay of fertility return after discontinuation of using depo-provera. The median delay of fertility return in this study was found to be 10 months from date of depo-provera discontinuation. This is in agreement with a facility based cross-sectional study conducted on 773 in Addis Ababa, Ethiopian women and communitybased cross-sectional survey undertaken on 849 women aimed to determine duration of return to fertility after discontinuation of depo-provera in South Africa. However, the result of this study was slightly higher than the prospective cohort study conducted on 796 Thailand women which documented the median delay in return of fertility after discontinuation of DMPA was 9 months and slightly lower than the studies conducted in Australia which documented the median delay in fertility return was 10.8 months and 11 months in India respectively. The variation in the duration of delay of fertility return might be attributed to genetic, ethnic variation of study population and methodological differences.
A woman’s age is an important factor affecting fertility return after discontinuation of depo-provera. The younger age group women experienced a faster return to fertility after discontinuing DMPA than older women. This demonstrates that a woman's age influences the length of time it takes for her fertility return after discontinuation of DMPA. This finding is in line with prospective cohort study conducted in Northern Thailand and Chiang Mai women on return of fertility after discontinuation of depo-provera. The higher proportion delay of fertility return in the older women of DMPA users is what one would expect in the general population. Because women's fertility declines as they aged, regardless of whether or not they used depo-provera.
The study revealed that, monthly family income was significantly associated with delay in return to fertility after discontinuation of depo-provera. This means that as household income increases, the likelihood of a delay in return to fertility after discontinuation of depo-provera use increases as well. This finding is in line with studies conducted in Addis Ababa, Denmark and North America [20].
Delay of fertility return increases as the age at first sex increases. This finding is consistent with previous reports supporting the importance of age at sexual debut to determine delay in return to fertility after discontinuation of depo-provera conducted in the United States and Addis Ababa. Regarding weekly sexual intercourse frequency, as weekly sexual intercourse frequency increases the odds of delay in return to fertility after discontinuing DMPA use decreases. This finding is in line with findings of studies conducted in Denmark, Japan and Addis Ababa.
There was no evidence that long-term use of depo-provera increases the time it takes to return to fertility after discontinuation of using depo-provera. Since there is no accumulation of depo-provera in the circulation over time, the time required to resume fertility after discontinuing depoprovera is solely dependent upon the duration of effective circulating levels of provera after the last injection. This is supported by the absence of relationship between the number of injections received and subsequent time to conception. Which is in line with study conducted in Thailand and USA. There was no difference in delay of fertility return after discontinuation of DMPA between nulliparous and parous women, which is supported by prospective cohort studies conducted on return of fertility after use of the injectable contraceptive depo-provera in London and Thailand.
Limitation of the study
Participants might have recall bias because some questions rely on their self-report of historical events. In this case it is difficult to validate claims made by respondents.
Conclusion
After discontinuation of depo-provera there is significant delay in the return to fertility. Fertility returns after discontinuation of using depo-provera was found to be associated with age group, monthly family income, age at first sex and weekly sexual intercourse frequency.
The amount of previous use of DMPA did not show significant association with the delay of fertility return after discontinuation of using depo-provera. Moreover, no difference was seen in the return of fertility between null gravid and gravid women after discontinuation of DMPA, indicating that use of injectable contraceptives does not need to be restricted to women who have completed their family sizes.
Recommendations
- Health professionals at health facility may refer this finding to counsel their clients concerning the median time it takes to fertility return after discontinuing DMPA.
- Health professionals may recommend other types of modern family planning methods for clients who want to resume their fertility right away after stopping family planning depending on client’s choice.
- All women have to talked about side effect of depo-provera concerning delay in return to fertility after discontinuation of using it prior depo-provera use.
Acknowledgments
The authors would like to thank all respondents for their willingness to participate in the study.
Competing Interests
No conflicts of interest in this work among authors.
Ethics Approval and Consent to Participate
All methods of this study were carried out under the Declaration of Helsinki’s ethical principle for medical research involving human subjects. Ethical approval to conduct this study was obtained from the ethical review board of Ambo University (Ref. No: DRE/005/21). An official letter was sent to the Gindeberet woreda health office. A permission letter was delivered to the Woreda health office. Then, the woreda health office sent supportive letters to respective public health facilities. For uneducated participants informed consent was obtained from their parents or friends and for educated participants it was taken from the participants themselves. Confidentiality and privacy of the information was maintained. The participants were informed that participation is voluntary.
Publication Consent
All authors of the study agreed to publish the study in Dove Press. Publication consent was obtained from the publication office of Dambi Dollo University after reviewing the mother document.
Availability of Data
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Authors Contribution
AT has been working on data analysis and writing up the final results, GF has been working on proposal preparation and TN has been working on overall activities.
Funding
No any source of Fund for this research.
References
- Curtis KM, Jatlaoui TC, Tepper NK. US selected practice recommendations for contraceptive use, 2016. Morbidity and Mortality Weekly Report: Recommendations and Reports. 2016;65(4):1-66.
[Crossref] [Google Scholar] [PubMed]
- Odwe G, Gray K, Kyarimpa A, Obare F, Nagendi G. Introduction of subcutaneous depot medroxyprogesterone acetate (DMPA-SC) injectable contraception at facility and community levels: pilot results from 4 districts of Uganda. Glob Health Sci Pract. 2018;6(4):711-722.
[Crossref] [Google Scholar] [PubMed]
- Fotherby K, Howard G. Return of fertility in women discontinuing injectable contraceptives. J Obstet Gynaecol. 1986;6:S110-S115.
[Crossref] [Google Scholar] [PubMed]
- Idowu A, Osinusi E, Awubite LE, Obisesan IO. Contraceptive self-injection knowledge, attitude and practices among female students of a tertiary health institution in south west Nigeria. Int J Rep Contracept Obstet Gynecol. 2022;11:323-332.
- Johnson SA, Kaggwa MN, Lathrop E. How it started, and how it’s going: global family planning programs. Clin Obst Gynecol. 2021;64:422-434.
[Crossref] [Google Scholar] [PubMed]
- Itriyeva K. Use of Long-Acting Reversible Contraception (LARC) and the Depo-Provera shot in adolescents. Current Prob Ped Adol Heal Care. 2018;48(12):321-332.
[Crossref] [Google Scholar] [PubMed]
- Girum T, Wasie A. Return of fertility after discontinuation of contraception: A systematic review and meta-analysis. Contracept Reproduct Med. 2018;3:1-9.
[Crossref] [Google Scholar] [PubMed]
- Mulatu T, Sintayehu Y, Dessie Y, Deressa M. Modern family planning utilization and its associated factors among currently married women in rural eastern Ethiopia: A community-based study. Bio Med Res Int. 2020;2020:1-9.
[Crossref] [Google Scholar] [PubMed]
- Ijasan O, Upeh ER. A 10-year review of progestogen-only injectable contraceptive use at a private facility in Lagos, Southwest Nigeria. New Nigerian J Clin Res. 2020;9:81.
- Zerihun T, Bekele D, Birhanu E, Worku Y, Deyesa N, Tesfaye M. Family planning awareness, utilization and associated factors among women of reproductive age attending psychiatric outpatient care, a cross-sectional study, Addis Ababa, Ethiopia. Plos One. 2020;15(9):e0238766.
- McDaniel EB. Return of fertility following discontinuation of three-month contraceptive injections of DMPA plus routine oral estrogen supplement: A preliminary report. Fertility Sterility. 1971;22(12):802-806.
[Crossref] [Google Scholar] [PubMed]
- Pardthaisong T. Return of fertility after use of the injectable contraceptive depo provera: Up-dated data analysis. J Bio Sci. 1984;16(1):23-34.
- Spevack E. The long-term health implications of depo-provera. Integrative Medicine. 2013;27.
[Crossref] [Google Scholar] [PubMed]
- Pardthaisong T, Gray R, Mcdaniel E. Return of fertility after discontinuation of depot medroxyprogesterone acetate and intra-uterine devices in Northern Thailand. Lancet. 1980;315:509-512.
[Crossref] [Google Scholar] [PubMed]
- Veisi F, Zangeneh M. Comparison of two different injectable contraceptive methods: Depo-Medroxy Progesterone Acetate (DMPA) and cyclofem. J Family Reproduct Health. 2013;7(3):109.
[Google Scholar] [PubMed]
- Dahan-Farkas N, Irhuma M. Long-acting reversible hormonal contraception. South African Fami Pract. 2016;58(5):64-67.
- Guo J, Li Y, Hou M, Han S, Ren J. Recognition of daily activities of two residents in a smart home based on time clustering. Sensor. 2020;20(5):1457.
[Crossref] [Google Scholar] [PubMed]
- Lafort Y, Jocitala O, Candrinho B. Are HIV and reproductive health services adapted to the needs of female sex workers? Results of a policy and situational analysis in Tete, Mozambique. BMC Health Services Research. 2016;16(1):1-9.
- Mcdaniel EB, Pardthaisong T. Return of menstruation and fertility in Thai women after contraceptive injections. J Bio Sci. 1971;3(2):209-222.
[Crossref] [Google Scholar] [PubMed]
- Mane NS, Rokade JV. Study the acceptance, compliance and efficacy of injection depot medroxy progesterone acetate as contraception: A prospective observational study. Int J Reprodt Contra Obstetric Gynecol. 2021;10(1):303-308.
Citation: Tolera TN, Kubela AT, Obssie GF (2025) Delay in Return to Fertility after Discontinuation of Using Depo-Provera and Associated Factors among Currently Pregnant Women Attending Antenatal Care in Public Health Facilities in Gindeberet District, Oromia, Ethiopia, 2021: Facility based Cross Sectional Study. Bio Med. 17:780.
Copyright: © 2025 Tolera TN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Sources of funding : No any source of Fund for this research.


