Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 5, Issue 2
Crystalloid Fluid Pre-loading or Co-loading for Prevention of Spinal Anesthesia Induced Hypotension at Gandhi Memorial Hospital, 2016 Addis Ababa, Ethiopia: Comparative Cohort Study
Abebe Tiruneh1*, Simegnew Kibret1 and Meron Abrar22Department of Anesthesia, Health Science College, Addis Ababa, Ethiopia
Received: 25-Jan-2021 Published: 16-Feb-2021, DOI: 10.35248/2684-1606.21.5.143
Abstract
Introduction: Caesarean section is a common procedure done in hospitals including in Ethiopian hospitals. Spinal anesthesia remains the preferred choice for Cesarean deliveries across the world with a low failure rate. However spinal anesthesia-induced hypotension is the commonest complication and the incidence ranges from 53.3% to 83%.
Objectives: To compare the preventive effect of crystalloid fluid preloading and co-loading for spinal-induced hypotension and its incidence, severity, and use of vasoconstrictors in obstetric mothers undergoing cesarean section at Gandhi Memorial hospital 2016 Addis Ababa, Ethiopia.
Methods: Cohort study design was used with a total of 96 mothers (48 of them preloaded and 48 of them coloaded with 1000 ml ringer lactate) involved in the study. Preoperative and other variables filled on the questioner than the Blood Pressure measured on an anesthesia monitor every 5 and 10-minute intervals till 60 minutes after spinal anesthesia was given. The data inter into EPI info and SPSS then finally analyzed with student T-test, chi-square or Fisher exact test and P value less than 0.05 declared as statistically significant.
Results: Incidence of spinal anesthesia-induced hypotension was high in the preload group 81.2% (39/48) and low in coload group 35.4% (17/48) and the result is statistically significant. Frequent Episode and more sever spinal anesthesia-induced hypotension were also common in the preload group.
Conclusion: Crystalloid fluid coloading to the operating mothers during the cesarean section was a better option for the prevention of spinal anesthesia-induced hypotension.
Keywords
Spinal anesthesia; Hypotension; Preload; Coload; Fluid
Abbreviation/Acronyms
ANP: Atrial Natri Peptide; APGAR: Activity, Pulse, Grimace Appearance, Respiration; ASA: American Society of Anesthesiology; BP: Blood Pressure; CI: Confidence Interval; HT: Height; KG: Kilo Gram; RR: Relative Risk; SD: Standard Deviation; SPSS: Statistical Package for Social Science; WT: Weight; χ2: Chi-square
Introduction
Cesarean section is a common procedure done in hospitals. A study done in Pakistan showed that it accounts for 21.4% of in- hospital deliveries [1]. In Ethiopia also there is a higher percentage of cesarean section delivery with 31.1% in governmental and 48.3% in private hospitals [2]. Spinal anesthesia remains the preferred choice for Cesarean deliveries across the world with a low failure rate. From hospital operated delivery 72% of them performed by spinal anesthesia [3].
Spinal anesthesia has its complications like hypotension, nausea, vomiting, shivering, post-dural puncture headache, and high spinal. Spinal anesthesia-induced hypotension is the commonest complication and the incidence ranges from 53.3% to 83% [4]. Hypotension is the physiologic consequence of spinal anesthesia and can have a potentially deleterious impact on both the mother as well as the fetus. The risk factors for the development of severe hypotension include; age ≥ 35 years, obesity (body mass index ≥ 29-35 kg/m2 ), pre-operative hypertension, associated co-morbidities, Level of a block (block above Thoracic 6 causes more), baricity of the local anesthetic agent (hyperbaric cause more than the isobaric and hypobaric solution, speed of the local anesthesia (faster than 0.2 ml/second cause more hypotension) and Higher fetal Weight [5].
Prophylaxis use of ephedrine has been used before spinal blockage but hypotension was still occurring in 12% of cases [6]. The large volume of fluid administration before the block also does not prevent the incidence of hypotension rather has fluid overload complication on mothers and the fetus [7]. 13 ml/kg fluids were recommended in addition to maintenance fluid to decrease the incidence of hypotension by 50% [8]. Administration of colloid or crystalloid fluid was used for the prevention method of spinal induced hypotension but there is no statistically significant difference between fluids [9].
There are two thoughts in the timing of fluid administration for the prevention of spinal-induced hypotension, Preloading and co-loading, preloading means the administration of fluid 10 to 20 minutes before spinal anesthesia administered whereas co-loading means fluid administration at the time of spinal blockage. Traditionally preload was considered as the best option for prevention of spinal induced hypotension, however such fluid administration, especially with crystalloids, results in rapid redistribution of the fluid into the extravascular compartment and may induce the secretion of atrial natriuretic peptide (ANP) which causes peripheral vasodilatation and excretion of the preload fluid hypotension occur in 15% from the coload group and 40% from the pre-load group [10]. This result is not the same for all scholars and some shows that both techniques fail to prevent effectively rather use both techniques with vasoconstrictor prophylaxis for a better option in the prevention of spinal-induced hypotension [11].
This study aims to compare the preventive effect of crystalloid fluid preloading and co-loading for spinal-induced hypotension incidence, severity, and use of vasoconstrictors in obstetric mothers undergoing cesarean section and expect to get the best choice for prevention of spinal anesthesia-induced hypotension.
Methods
This cohort study was conducted at Gandhi Memorial Hospital which is located in the capital city of Ethiopia, Addis Ababa. It is one of the thirteen government hospitals found in Addis Ababa and under the management of Addis Ababa Health Bureau. The Hospital primarily gives services for women and children. A study was conducted from November 2016 to February 2017. A comparison of two proportions with equal sample size formula for the independent cohort was used and by considering the previous study with the incidence of hypotension 40% from preload and 15% from coload group [9] then the final sample size was 96 (48 from each group). The systematic random sampling technique was used for the selection of the study subjects. The preload group used 1000 ml ringer lactate fluid within 10-20 minutes intravenously before spinal anesthesia is given and the coload group 1000 ml ringer lactate solution given within 5 minutes (with large size IV cannula rapidly intravenously) at the same time spinal anesthesia also given. All mothers were given spinal anesthesia in the sitting position plain Lidocaine with 26 gages cutting spinal needle. The questioner was prepared in English which includes socio- demographic data, preoperative Blood Pressure, parity, gestational age, ASA classification, time of fluid administration, the volume of fluid used, total estimated blood loss, type of local anesthesia, baricity, level of a block, used vasopressor, uterine contraction agent, neonatal Weight and APGAR score, the incidence of nausea and vomiting, Heart rate and Blood Pressure. The Blood Pressure was measured within 2 minutes and a 5 minute interval till 60 minutes from the start of spinal anesthesia given. The data collection was undertaken after gotten ethical clearance from the Addis Abbaba university college of health science ethical review committee and permission letter from Gandhi memorial hospital. Written consent from the patients obtained and Confidentiality of the information assured by using code numbers than personal identification names and keeping questionnaires locked.
Data were checked manually for completeness and then entered into EPI info version 7 then finally coded and transferred to SPSS version 20 computer program for cleaning and analysis. Descriptive statistics used to summarize data, tables and figures. Mothers recorded as having hypotension when systolic Blood Pressure recorded less than 100 mmhg during the recording times. The hypotension management depends on the responsible anesthetist that manages the mothers throughout the procedure. The student t-test, chi-square test, or Fisher exact test used for analysis, and p-value less than 0.05 were considered as statistically significant.
Operational definitions
Cesarean section: Is delivery of the fetus along with the placenta and membrane under anesthesia through the incision of the abdominal and intact uterine wall after the fetus reached viability.
Spinal anesthesia: It is a type of regional anesthesia in which local anesthetic agents are administered in subarachnoid space.
The loading: Giving fluid within 5 minutes while we perform spinal anesthesia at the same time.
Preloading: Administration of fluid for 20 minutes before spinal anesthesia was initiated.
Hypotension: Decrement of systolic Blood Pressure by 20% and above from the baseline or SBP less than 100 mmhg.
Severe hypotension: Systolic hypotension less than 80 mmhg or reduction of 40% and above from the baseline.
Trendelenburg position: The body is laid flat on the back with the feet higher than the head by 15-30 degrees.
Results
A total of 96 mothers who operated upon under spinal anesthesia were included and completed the study. age, HT, baseline systolic BP and heart rate were comparable. From these patients, 48 were given preload and 48 were coloaded. Finally, the groups were compared in the study variables. Total blood loss during the surgery, duration of the surgery, APGAR score, and neonatal wt also comparable in the group (Table 1). All mothers used 40 mg (2 ml of 2%) hyperbaric plain Lidocaine between L3 and L4 interspace in a sitting position by 26 gauge spinal needle. For the level of the sensory block, only 5 mothers from the preload group and 3 mothers from coload groups achieved above T6 and the others below this. All mothers used a 1000 ml ringer lactate solution before spinal anesthesia (preload) and during anesthesia within 5 minutes (coload) intravenously. Used uterogenic agents were Oxytocin (20 IU), Ergometrine (1 mg), and combined form from preload groups 29,7,12 and from coload groups 28,13 and 26 mothers respectively.
| Variables | Preload group | Coload group | P-value |
|---|---|---|---|
| Age (year) | 30.3 ± 5.2 | 29.2 ± 5.1 | 0.3 |
| HT (cm) | 160.8 ± 7.7 | 159 ± 7.4 | 0.53 |
| Gravidity | 1(I-III) | I (I-III) | 0.4 |
| ASA status | II (I-II) | II (I-II) | 0.2 |
| Systolic BP before anesthesia | 129.85 ± 8.7 | 126 ± 10.2 | 0.52 |
| HR before anesthesia | 86.2 ± 10.8 | 87 ± 9.9 | 0.68 |
| Duration of surgery in min | <40 min (40-50 min) | <40 min (40-60 min) | 0.7 |
| Blood loss (ml) | 605 ± 72 | 610 ± 67 | 0.7 |
| Level of sensory block | T10 (T10-T6) | T10 (T10-T6) | 0.3 |
| APGARscoreat 1 min | 8 ± 0.8 | 8.1 ± 0.8 | 0.38 |
| APGARscoreat 5 min | 9 ± 0.6 | 8.9 ± 0.7 | 0.53 |
| Neonatal WT (kg) | 2.96 ± 0.38 | 2.96 ± 0.23 | 0.92 |
Values are given as mean ± SD or median and (range)
Table 1: Demographic data, patient the base line vs. characteristics, duration of surgery, and neonatal conditions in each group Addis Ababa, Gandhi Memorial Hospital Ethiopia, June 2017 (n=48 cohort index and n=48 reference cohort).
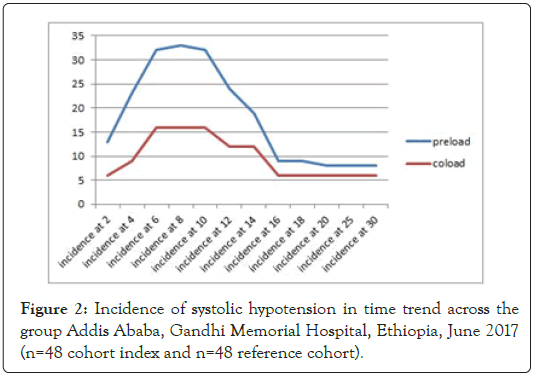
Incidence of systolic hypotension among the group
Systolic hypotension has occurred in high number of mothers within the first 30 minutes of both groups. There was a significant difference between the group on the incidence of systolic hypotension from 2 minutes to 30 minutes after spinal anesthesia was administered (Table 2).
| Time in minute | Preload | Coload | χ2 | RR | P value |
|---|---|---|---|---|---|
| 2 | 13 | 6 | 3.2 | 1.5 | 0.07 |
| 4 | 23 | 9 | 9.8 | 1.8 | 0.002 |
| 6 | 32 | 16 | 10.6 | 2 | 0.001 |
| 8 | 33 | 16 | 12 | 2.1 | 0.001 |
| 10 | 32 | 16 | 9.8 | 1.8 | 0.002 |
| 12 | 24 | 12 | 6 | 1.6 | 0.01 |
| 14 | 19 | 12 | 2.2 | 1.3 | 0.1 |
| 16 | 9 | 6 | 0.7 | 1.2 | 0.3 |
| 18 | 9 | 6 | 0.7 | 1.2 | 0.3 |
| 20 | 8 | 6 | 0.3 | 1.1 | 0.3 |
| 25 | 8 | 6 | 0.3 | 1.1 | 0.3 |
| 30 | 8 | 6 | 0.3 | 1.1 | 0.3 |
Note: χ2: chi-square, RR: Relative Risk
Table 2: Incidence of systolic hypotension in the first 60 minutes after spinal anesthesia in the groups Addis Ababa, Gandhi Memorial Hospital Ethiopia, June 2017 (n=48 cohort index, and n=48 reference cohort).
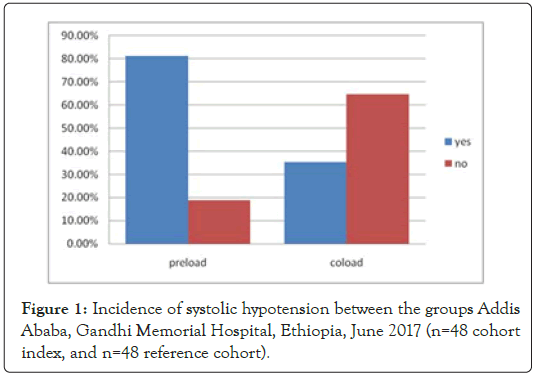
The incidence of systolic hypotension after spinal anesthesia was 81.2% (39/48) in the preload group and 35.4% (17/48) in the coload group which is statistically significant (p<0.05). More number of mothers develop spinal anesthesia-induced systolic hypotension was from the preloaded group (RR=2.55, 95% CI- 1.52-3.44) (Figure 1). Diastolic hypotension (79% vs. 39%) and mean hypotension incidence (75% vs. 37%) were also almost the same with systolic hypotension in preload and coload group respectively. More hypotension was recorded in the first 20 minutes (Figure 2). 5 mothers from preload and 1 mother from coload group develop sever form of hypotension (reduced more than 40% from the baseline).
Figure 1: Incidence of systolic hypotension between the groups Addis Ababa, Gandhi Memorial Hospital, Ethiopia, June 2017 (n=48 cohort index, and n=48 reference cohort).
Figure 2: Incidence of systolic hypotension in time trend across the group Addis Ababa, Gandhi Memorial Hospital, Ethiopia, June 2017 (n=48 cohort index and n=48 reference cohort).
21 mothers from preload and 11 mothers from coload group develop 4 and above episodes of hypotension during the measuring time.1 mother from preload and 2 mothers from coload group use drugs in addition to fluid for hypotension management (adrenaline, atropine) but the difference is not statistically significant. In both groups, no mothers need of blood transfusion during the operation and no further complication was recorded like hysterectomy.
The volume of fluid required for hypotension management was also high among preloaded mothers. Of preloaded mothers, 12 of them need more than 1500 ml fluid whereas from coload groups only 1 mother needs more than 1500 ml fluid for hypotension management.
Discussion
Spinal anesthesia is considered to be safe compared with general anesthesia for cesarean section. General anesthesia is associated with a higher mortality rate in comparison with regional anesthesia. However, spinal anesthesia is not without risk. Hypotension is the most common side effect after spinal anesthesia. Cesarean section under spinal block requires sensory block from T4 to T6 this level of high block induces widespread vasodilation with resultant hypotension with the incidence of up to 90%. The sympathetic blockade after spinal anesthesia causes arterial and vasodilation resulting in hypotension; this is further aggravated by aortocaval compression.
But fluid preloading for cesarean section under regional anesthesia has been established as routine and considered to be a safe and effective method of reducing the incidence of hypotension previously.
In our study, 81% of patients in the preload group and 35% in the coload group develop hypotension.
The results of this study were close to other studies they showed that spinal induced hypotension high among pre-load groups than co-load groups [4,10,12,13].
Two mothers from coload use adrenaline and 1 mother from the preload group use adrenaline and atropine but the difference was not statistically significant. This result varies from other researches; Khan et al. showed that ephedrine and phenylephrine requirement was high in the preload group to manage spinal induced hypotension [13]. The difference was related to the protocol of hypotension management at its center.
Incidence of nausea and vomiting was higher in the preload group than coload group 52% vs. 27% respectively (χ2=6.27, RR=1.65 95%CI1.24-6.86) and which was associated with the incidence of systolic hypotension with χ2=13.9, RR=1.9, 95%CI=1.4-2.6 and P-value<0.05. This result was related to the work of Ah-young oh et al. they showed that 60% vs. 27% incidence of nausea vomiting in preload and coload group respectively.
Conclusion
Crystalloid fluid coloading to the operating mothers during the cesarean section was a better option for the prevention of spinal anesthesia-induced hypotension. No need of delaying the surgery and spinal anesthesia for fluid preloading mothers rather administering crystalloid fluid and spinal anesthesia at the same time was the better way of technique.
Limitation of the Study
We had used non-invasive Blood Pressure measurement and could not get beat to beat or every minute measurement of mother’s Blood Pressure and other limitations also we couldn’t appreciate the duration of hypotension in-between episodes of hypotension.
Acknowledgment
We want to also thank Addis Ababa University to support financially during data collection, and also Gandhi Memorial Hospital to permit us to do the research. And finally our friends for giving us language help and writing assistance.
Conflict of Interest
The authors confirmed that there is no conflict of interest.
Authors Contribution
All authors contribute from topic selection, proposal writing, analysis and manuscript writing.
REFERENCES
- Hafeez M, Yasin A, Badar N, Pasha MI, Akram N, Gulzar B. Prevalence and indications of caesarean section in a teaching hospital. JIMSA. 2014; 27(1): 92-93.
- Aman H, Negash S, Yusuf L. Original article cesarean delivery practices in teaching public and non- government/private MCH hospitals, Addis Ababa. Ethiop J Heal Dev. 2014; 28(1): 22-28.
- Ljubicic S, Nizic Z, Vukovic A, Car N, Ljubicic T. Cesarean section under spinal anesthesia in General Hospital of Dubrovnik; A decade after. Period Bio. 2013; 115(2): 257-260.
- Oh A, Hwang J, Song I, Kim M, Ryu J, Park H. Influence of the timing of administration of crystalloid on maternal hypotension during spinal anesthesia for cesarean delivery: Preload versus coload. BMC Anesthesiol. 2014; 14(36): 1-5.
- Hartmann B, Junger A, Klasen J, Benson M, Jost A, Banzhaf A, et al. The incidence and risk factors for hypotension after spinal anesthesia induction: An analysis with automated data collection. Anesth Analg. 2002; 94(6): 1521-1529.
- Salama AK, Goma HM, Hamid BMA. Fluid preloading versus ephedrine in the management of spinal anesthesia-induced hypotension in parturients undergoing cesarean delivery: A comparative study. J Anaesthesiol. 2016; 9: 72-75.
- Ackson RJ, Eid JAR, Horburn JT. Volume preloading is not essential to prevent spinal-induced hypotension at caesarean section. Br J Anaesth. 1995; 75: 262-265.
- Xu S, Wu H, Zhao Q, Shen X, Guo X, Wang F. The median effective volume of crystalloid in preventing hypotension in patients undergoing cesarean delivery with spinal anesthesia. Rev Bras Anestesiol. 2012; 62(3): 312-324.
- Tamilselvan P, Fernando R, Bray J, Sodhi M. The effects of crystalloid and colloid preload on cardiac output in the parturient undergoing planned cesarean delivery under spinal anesthesia: A randomized trial. Anesth Analg. 2009; 109(6): 1916-1921.
- Varshney RK, Kapoor K. A Randomised prospective double blind study to compare the effects of fluid preloading and co-loading during spinal anaesthesia for caesarean delivery. Ann Int Med Den Res. 2016; 2(1): 410-414.
- Jit S, Bajwa S, Kulshrestha A, Jindal R. Anesthesia: Essays and researches co-loading or pre-loading for prevention of hypotension after spinal anaesthesia! A therapeutic dilemma. Anesth Essays Res. 2013; 7(2).
- Rao AR, Vijaya G, Mahendra BVVN. Comparison of effects of preloading and coloading with ringer lactate in elective caesarean section cases under spinal anaesthesia. J Dent Med Sci. 2015; 14(10): 57-64.
- Khan M, Farooqi A, Ahmad N, Qaz S. Crystalloid co-load: A better option than crystalloid pre-load for prevention of postspinal hypotension in elective caesarean section. Internet J Anesthesiol. 2013; 32(1): 6-13.
- Banerjee A, Stocche RM, Angle P, Halpern SH. Preload or coload for spinal anesthesia for elective cesarean delivery: A meta-analysis. Can J Anesth. 2010; 57: 24-31.
- Farid Z, Mushtaq R, Ashraf S, Zaeem K. Comparative efficacy of crystalloid preloading and co-loading to prevent spinal anesthesia induced hypotension in elective caesarean section. PJMHS. 2016; 10(1): 42-45.
- Khan MU, Memon AS, Ishaq M, Aqil M. Preload versus coload and vasopressor requirement for the prevention of spinal anesthesia induced hypotension in non-obstetric patients. J Coll Physicians Surg Pakistan. 2015; 25(12): 851-855.
- Kulkarni AG, Asai O, Tarkase AS. Comparative evaluation of co-loading versus preloading for prevention of post-spinal hypotension in elective caesarean section. Indian J Clin Anaesth. 2016; 3(3): 335-341.
- Sailo L. To compare the haemodynamic changes between colloid preload and co-load in preventing maternal haemodynamic changes during spinal anaesthesia for elective caesarean delivery. Abstract: Exp. 2015; 30(1): 1970-1966.
- Sharma A, Gupta PK, Singh SN, Uprety D. Crystalloid prehydration versus cohydration for prevention of hypotension during spinal anaesthesia for elective caesarean section. Heal Renaissanc. 2014; 12(3): 190-196.
- Tawfik MM, Hayes SM, Jacoub FY, Badran BA, Gohar FM, Shabana AM, et al. Comparison between colloid preload and crystalloid co-load in cesarean section under spinal anesthesia: A randomized controlled trial. Int J Obstet Anesth. 2014; 23(4): 317-323.
Citation: Tiruneh A, Kibret S, Abrar M (2021) Crystalloid Fluid Pre-loading or Co-loading for Prevention of Spinal Anesthesia Induced Hypotension at Gandhi Memorial Hospital, 2016 Addis Ababa, Ethiopia: Comparative Cohort Study. J Surg Anesth. 5:143.
Copyright: © 2021 Tiruneh A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.