Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Scientific Indexing Services (SIS)
- Euro Pub
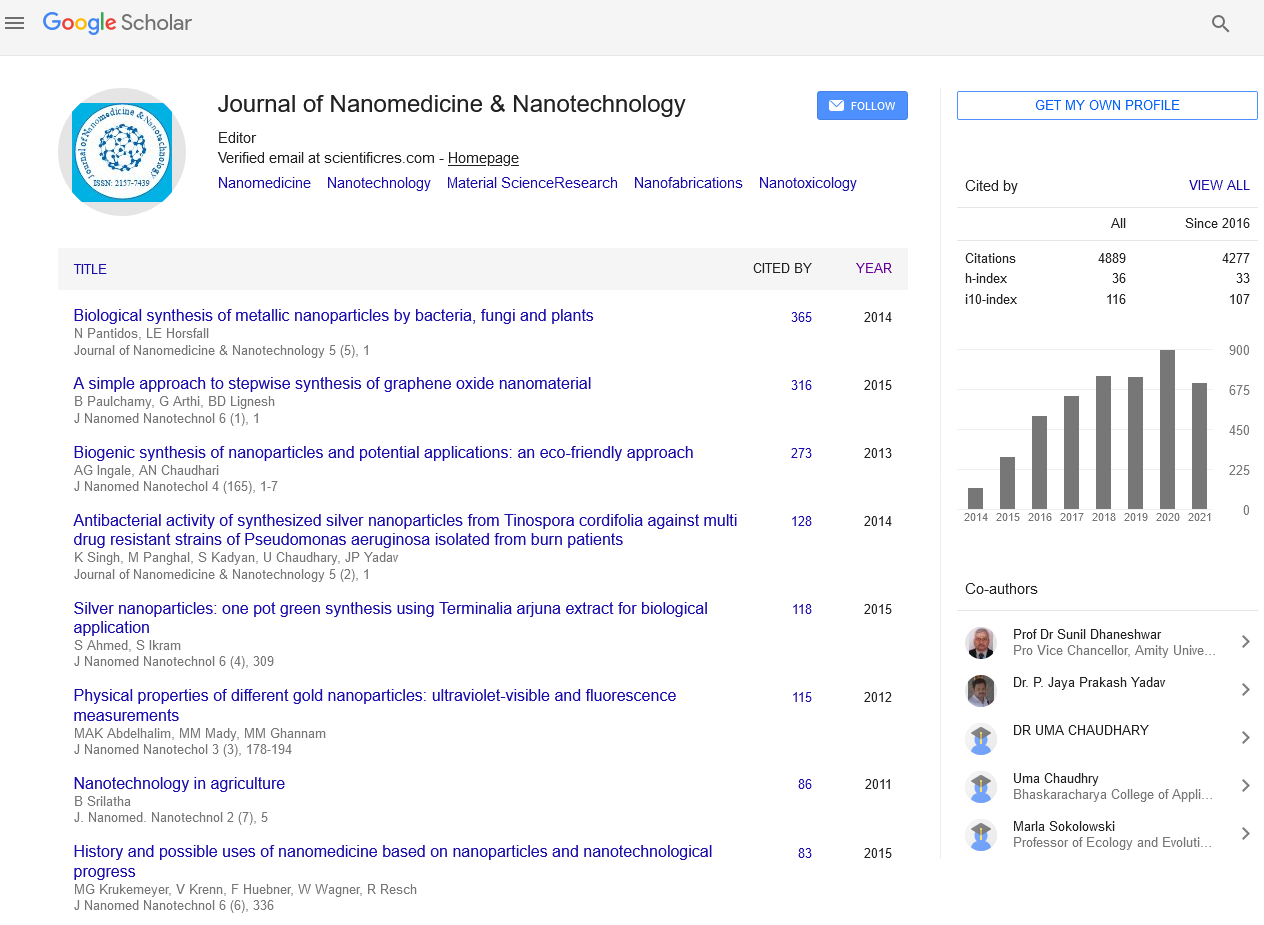
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2022) Volume 13, Issue 11
Chitosan Nanoparticles And Functional Repair Of CNS Tissue
Jun Lu*Received: 01-Nov-2022, Manuscript No. jnmnt-22-19106; Editor assigned: 04-Nov-2022, Pre QC No. jnmnt-22-19106; Reviewed: 18-Nov-2022, QC No. jnmnt-22-19106; Revised: 22-Nov-2022, Manuscript No. jnmnt-22-19106; Published: 30-Nov-2022, DOI: 10.35248/2157-7439.22.13.648.
Abstract
Maintaining the physiological structure and function of a cell necessitates maintaining the integrity of the cell membrane. After cell membrane disruption, for instance, immediate function loss, progressive degeneration, and the death of neurons following acute spinal cord injury (SCI). After damage, spontaneous membrane self-repair is frequently initiated, but it fails to overcome the overwhelming tissue distortion and physiological disturbance, such as unregulated Ca2+ influx, the generation of reactive oxygen species (ROS), and subsequent lipid peroxidation (LPO). In the early stages of Central Nervous System (CNS) damage interfering with progressive secondary injury; it would be most important of all therapies to restore membrane integrity quickly and effectively.
Keywords
Central Nervous; Progressive Degeneration; Peroxidation; Nanotechnology; Silver nanoparticle
INTRODUCTION
It has been demonstrated that water-soluble polymers like polyethylene glycol (PEG) can satisfy a number of the aforementioned requirements. PEG and other synthetic polymers break down membranes quickly and effectively [1]. In addition, it has the capability of preserving significant structural, physiological, and behavioral function following SCI, TBI, and even localized peripheral nerve damage. However, following acute clinical neurotrauma, its administration must be limited in both concentration and timing due to the viscosity of high molecular weight (MW) and the toxicity of low molecular weight (MW) following PEG degradation. Thirty-one demonstrates that PEG can be extremely toxic to CNS tissue under certain conditions .Recuperation of Social and Physiological Capability in Vivo page 128 in Borgens 2003. Studies conducted in a parallel field of study demonstrated that Chitosan also possessed sealing properties that were comparable to PEG but even more significant. In point of fact, the effect of chitosan, a non-toxic biodegradable polysaccharide polymer [2], has already been extensively studied and utilized in a variety of biomedical and industrial applications. These applications include beverage clarification, wound healing, surgical adhesion, and drug delivery.
Steps Involved
Chitosan's chemical properties are mostly determined by two variables: the MW and acetylation degree (DA).The number of free amino groups in the chitosan polymer is inversely proportional to the degree of protonation and is determined by the DA. In contrast, when the polymer is presented to targets like cells and tissues in solution, the MW determines the length of the main chain, which may have an impact on the solution's viscosity and shape [3]. According to previous research, the DA is essential for artificial membrane incorporation, mammalian membrane sealing, and ex vivo restoration of neurophysiological function. It has been proposed that the primary physical driving force for the chitosan backbone's cationic deacetylated unit, -(1–4)-linked D-glucosamine's membrane adsorption and incorporation is the electrostatic interaction between the cell membrane's negative charged lipid headgroups and the primary amines [4].
METHODS
After chitosan adsorption onto the membrane surface, it is also claimed that the effect of the hydrophobic interaction between the inner non-polar hydrocarbon chain of the membrane and the nonionic acetylation unit, N-acetyl-D-glucosamine, on the backbone of chitosan completes membrane insertion. The morphological structure of chitosan in the aqueous solution is closely related to MW, as previously stated. According to previous research, the physical shape and viscosity of chitosan in its aqueous form play a significant role in biomedical applications [5]. In addition, we have discovered that, regardless of viscosity, chitosan in an injectable solution moves throughout the systemic circulation. As a result, it does not appear to matter which route of administration is used, intraperitoneal, intravenous, or subcutaneous, as with PEG .The concentration of the polysaccharide that is circulating throughout the body decreases when nanoparticles and microparticles offer increased targeting to damaged cells.This study is the first to test whether chitosan nanoparticles can reach and repair damaged tissues like chitosan in aqueous solution in spinal injured animals with vascular trauma [6].
RESULT
Additionally, the influence of chitosan's MW on membrane organization has been discussed, primarily in the context of artificial lipid membranes as a simplified cell model. The issue, however, was not resolved .Fang reported that lipid bilayers had stronger interactions with chitosan with higher MWs, as evidenced by significantly fewer cooperative units than with lower MWs [7]. Quemeneur, on the other hand, observed the independent effect of chitosan's MW on membrane adsorption in environments with controlled ph. We present the first functional test of subcutaneous injection of chitosan nanoparticles (100–200 nm diameters) to adult guinea pigs with crush/compression injury to the midthoracic spinal cord, advancing our laboratory's success in using Chitosan as an acutely applied membrane "sealant."
By utilizing nanoparticles larger than 100 nm, Chitosan can be delivered to only the interface of damaged cells—which, of course, make up damaged tissues—without having to distribute the polymer throughout the body, as we have previously reported [8]. We further tested the "membrane repair" activity of Chitosan with various degrees of acetylation and molecular weight to determine the best composition/fabrication for further clinical and clinically oriented studies after demonstrating a functional benefit of nanoparticle administration. In these tests of membrane integrity, chemically modified chitosan in solution was used. The assessing the transfer of a significant enzyme from the cytoplasm to the extracellular environment; and B), a dye molecule entering the cytoplasm through a damaged membrane [9]. Provides a more in-depth discussion as well as technical details regarding these "dye exclusion" techniques.In the long run, our goal is to develop a biodegradable alternative to PEG for use in acute neurotrauma [10].
DISCUSSIONS
After a severe crush of the mid-thoracic spinal cord in an adult guinea pig, our preliminary findings from the "whole animal" suggest that subcutaneous injection of Chitosan nanoparticles significantly improves nerve impulse conduction through the lesion and upwards to the cerebral sensory centers. Conduction remained silent in the absence of this experimental treatment. This is the first study of chitosan nanofabrications in any in vivo neurotrauma model, according to our knowledge. These findings are consistent with a previous in vitro study that demonstrated a significant interference with membrane sealing, the unique capacity of chitosan particles to transport a "drug cargo," and progressive secondary injury mechanisms in acrolein-infected cell samples. Its therapeutic potential is significantly increased as a result.
CONCLUSION
Our outcomes uncover that Chitosan nanoparticles can to be sure capability as a significant mediation in intense spinal line injury by enhancing the impacts of intense pressure/pulverize to the grownup guinea pig spinal rope. The basis for the functional recovery of motor, sensory, and autonomic functioning following neurotrauma is laid out here by the physiological recovery of conduction. However, with caution, this promise will not be realized until behavioral outcome measure recovery that is clinically meaningful is demonstrated. In addition, we do not believe that MW or DA played a significant role in the development of this use of a safe biodegradable polysaccharide for the clinical treatment of SCI or TBI after evaluating various compositions of chitosan in controlled solutions ex vivo. To put it another way, regardless of DA and MW, chitosan had a strong membrane-sealing effect on damaged spinal cord tissues. In particular, the TMR and LDH studies confirmed that chitosan significantly inhibited. The application of an external dye into damaged spinal cord cells in addition to the large endogenous enzyme LDH's escape through membrane defects.
REFERENCES
- Merlin JPJ, Li X. Role of Nanotechnology and Their Perspectives in the Treatment of Kidney Diseases. Front Genet. 2022; 12:817974.
- Balderrama-González AS, Piñón-Castillo HA, Ramírez-Valdespino CA, Landeros-Martínez LL, Orrantia-Borunda E, Esparza-Ponce HE. Antimicrobial Resistance and Inorganic Nanoparticles. Int J Mol Sci. 2021; 22(23):12890.
- Allahverdiyev AM, Kon KV, Abamor ES, Bagirova M, Rafailovich M. Coping with antibiotic resistance: combining nanoparticles with antibiotics and other antimicrobial agents. Expert Rev Anti Infect Ther. 2011; 9(11):1035-52.
- Alabresm A, Chandler SL, Benicewicz BC, Decho AW. Nanotargeting of Resistant Infections with a Special Emphasis on the Biofilm Landscape. Bioconjug Chem. 2021; 32(8):1411-1430.
- Gupta A, Mumtaz S, Li CH, Hussain I, Rotello VM. Combatting antibiotic-resistant bacteria using nanomaterials. Chem Soc Rev. 2019; 48(2):415-427.
- Makabenta JMV, Nabawy A, Li CH, Schmidt-Malan S, Patel R. Nanomaterial-based therapeutics for antibiotic-resistant bacterial infections. Nat Rev Microbiol. 2021; 19(1):23-36.
- Van Giau V, An SSA, Hulme J. Recent advances in the treatment of pathogenic infections using antibiotics and nano-drug delivery vehicles. Drug Des Devel Ther. 2019; 13:327-343.
- Lai MJ, Huang YW, Chen HC, Tsao LI, Chang Chien CF, Singh B, et al. Effect of Size and Concentration of Copper Nanoparticles on the Antimicrobial Activity in Escherichia coli through Multiple Mechanisms. Nanomaterials (Basel). 2022; 12(21):3715.
- Chen H, Zhang Y, Yu T, Song G, Xu T, Xin T, et al. Nano-Based Drug Delivery Systems for Periodontal Tissue Regeneration. Pharmaceutics. 2022; 14(10):22- 50.
- Kukushkina EA, Mateos H, Altun N, Sportelli MC, Gonzalez P, Picca RA, et al. Highly Stable Core-Shell Nanocolloids: Synergy between Nano-Silver and Natural Polymers to Prevent Biofilm Formation. Antibiotics (Basel). 2022; 11(10):1396.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Lu J (2022) Chitosan Nanoparticles and Functional Repair of CNS Tissue. J Nanomed Nanotech. 13: 648.
Copyright: ©2022 Lu J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.