Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2021) Volume 5, Issue 1
Case Report of Possible Intra-Operative Diabetes Insipidus during Cerebral Revascularisation in a Patient with Moyamoya Syndrome
Sarra Wang, Valerie Lan-Pak-Kee* and Chhaya SharmaReceived: 19-Dec-2020 Published: 11-Jan-2021, DOI: 10.35248/2684-1606.21.5.137
Abstract
Moyamoya (MM) is a rare cerebrovascular occlusive disease affecting the terminal portion of the internal carotid artery. It can be of primary idiopathic origin or secondary, where it is associated with other conditions such as Sickle Cell Disease (SCD). We present the anaesthetic management of a 16 year old female with SCD and MM undergoing a cerebral revascularisation procedure which was complicated by possible Central Diabetes Insipidus (CDI) intra-operatively. We hope to raise awareness of this rare disorder and add to the paucity of literature describing the anaesthetic management and potential peri-operative challenges posed by such patients.
Keywords
Cerebrovascular condition; Hyperplasia; Stenosis; General anaesthesia
Abbrevations
AVP: Endogenous Arginine Vasopressin; CDI: Central Diabetes Insipidus; DDAVP: Deamino-8-Darginine Vasopressin; DI: Diabetes Insipidus; MAC: Minimum Alveolar Concentration; MM: Moyamoya; MMD: Moyamoya Disease; MMS: Moyamoya Syndrome; SCD: Sickle Cell Disease; STA-MCA: Superficial Temporal Artery-Middle Cerebral Artery Anastomosis; TCI; Target-Controlled Infusion
Introduction
Moyamoya Disease (MMD) is a rare cerebrovascular condition characterised by progressive stenosis or occlusion of the supraclinoid internal carotid arteries. This can lead to ischaemia and compensatory growth of small collateral vessels. The diagnosis centres on the pathognomonic angiographic pattern of these vessels, resembling a puff of smoke. Patients can present with both ischaemic and haemorrhagic strokes [1]. Aetiology is unclear, and while MMD describes the idiopathic condition, Moyamoya Syndrome (MMS) describes those with the characteristic vasculopathy in conjunction with a recognised associated condition which includes haematological disorders such as Sickle Cell Disease (SCD) [2].
In MMS secondary to Sickle Cell Disease, the proposed pathogenesis involves impaired cerebral autoregulation and chronic vascular injury from sickling of red blood cells, resulting in intimal hyperplasia and stenosis [3]. Approximately 11% of children with untreated SCD develop neurovascular complications by the time they are 20 years old [3]. SCD patients with MMS are more than twice as likely to suffer a recurrent cerebrovascular event than those without MMS, despite regular blood transfusions to maintain HbS below 30% [4].
Treatment of symptomatic MM is predominantly surgical, as medical treatment for MM has not shown promise. The aim of surgical treatment is to augment cerebral perfusion (in ischaemic forms) or reduce neovessel overload (in haemorrhagic forms) [1]. These cerebral revascularisation techniques can be divided into direct and indirect techniques, with a common direct procedure being extracranial-intracranial anastomosis (e.g. superficial temporal artery-middle cerebral artery [STA-MCA] anastomosis) (Figure 1).
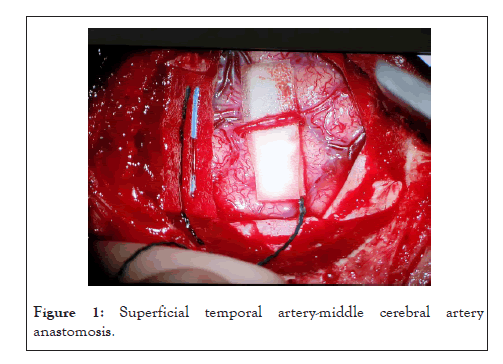
Figure 1:Superficial temporal artery-middle cerebral artery anastomosis.
There is limited research and guidance for the optimal peri- operative and anaesthetic management of MMS and SCD patients undergoing cerebral revascularisation surgery, other than optimisation of SCD and maintaining adequate cerebral blood flow peri-operatively. With this case report we hope to raise awareness of this disorder and add to the paucity of literature describing the anaesthetic management and potential peri- operative challenges posed by such patients.
Written consent for publication of this case report was obtained from the patient’s legal guardian.
Case Description
A 16 year old, 62 kg female with SCD and MMD presented for STA-MCA by pass. Her SCD was well controlled with infrequent intermittent transfusions maintaining HbS under 30%, but she had experienced both haemorrhagic and ischaemic intracranial events from MMS. There was no other history of note.
The patient was admitted the day before surgery for transfusion of 2 units of red blood cells. Upon arrival in the anaesthetic room, her blood pressure was 105/63 mmHg, similar to that measured pre-operatively. General anaesthesia was induced with midazolam 3 mg, fentanyl 200 mcg and propofol 80 mg. Tracheal intubation was facilitated with vecuronium 6 mg and a size 7.0 reinforced endotracheal tube was inserted without difficulty. Anaesthesia was maintained using a mixture of 0.6-0.7 Minimum Alveolar Concentration (MAC) of sevoflurane and Target-Controlled Infusion (TCI) of propofol and remifentanil (effect site concentrations of 1 mcg/ml and 1 ng/ml respectively). A 16 G cannula was inserted in addition to the 20 G cannula used for induction. A radial arterial line was placed to facilitate intra-operative haemodynamic and cardiac output monitoring, and to monitor arterial gases and electrolytes.
The intra-operative goals were to avoid any triggers for a sickle cell crisis in addition to maintaining adequate cerebral perfusion in the setting of MMS. Systolic blood pressure was maintained between 100-130 mmHg using a metaraminol infusion.
Balanced crystalloid solution (Plasma-LyteTM, Baxter Healthcare Corp, Deerfield, IL) was used for goal-directed fluid therapy (via FloTracTM, Edwards, Irvine, CA, USA). Cardiac index was maintained between 3.5-4 L/kg/min, stroke volume variation <15% and stroke volume 64-82 ml/beat. Her core body temperature was maintained between 36.5-37°C using warmed fluids and forced air warmer. End tidal carbon dioxide and arterial carbon dioxide tension measurements were used to maintain normocapnia between 4.0-4.5 kPa.
Urine output was initially normal but gradually increased and became markedly raised 4 hours following induction. This was in the absence of diuretic medications, hypertonic saline or mannitol administration. Six hours following induction, total urine output exceeded 4000 ml. At this stage, 4000 ml of balanced crystalloid solution had been administered to maintain euvolaemia and haemodynamic stability, cardiac output monitoring demonstrated ongoing fluid responsiveness. Blood gas analysis showed a rise in sodium from 138 mmol/L at the start of the case to 150 mmol/L. Urine appearance was noted to be very dilute and we hypothesised the possibility of Diabetes Insipidus (DI) causing the observed signs. We administered deamino-8- darginine vasopressin (DDAVP) 0.5 mcg intravenously six hours into the case. This appeared to decrease urine output and halt the rise of serum sodium as measured by blood gas analysis.
The patient was successfully extubated following a 9 hour bypass procedure. Total urine output was 6100 ml, with 6000 ml of balanced crystalloid solution administered to maintain euvolaemia.
No focal neurological deficit was noted in the immediate post- operative period and the patient did not require further DDAVP. Urine output normalised immediately post-operatively and serum sodium had fallen to 142 mmol/L in the formal blood panel taken several hours following the operation.
Discussion
Intra-operatively, this patient showed rising serum sodium and urine output (prior to DDAVP administration) would have approximated to 320 ml/kg/day prior to DDAVP administration, which exceeds the 40 ml/kg/day suggestive of Diabetes Insipidus [5]. Both serum sodium and urine output returned to acceptable levels following DDAVP administration, which is suggestive of Central Diabetes Insipidus (CDI).
Disruption to any part of the production, transport, storage and release of the Endogenous Arginine Vasopressin (AVP) may result in CDI. The risk of intraoperative cerebral ischaemia during revascularisation surgery for MM is well recognised, although subsequent post-operative neurological consequences are rare if strict peri-operative neuroprotective measures are applied [6]. In this patient, there were multiple risk factors for disruption of blood flow to the hypothalamus and pituitary- MMS, SCD and surgery. There is evidence to suggest that the characteristics of MMS in SCD may be different, these patients experience more unilateral MMS with moderate steno-occlusive disease, and posterior cerebral artery involvement is less common [7]. However, the clinical significance of these differences is yet to be determined.
We speculate that baseline blood supply to the hypothalamus may be disrupted at a subclinical level due to the pathophysiology of MMS. Consequently, clinically evident CDI was precipitated relatively easily by anaesthetic factors which we will explore.
There is no conclusive evidence on the optimal anaesthetic agent for patients with MM undergoing revascularisation surgery. In this case, anaesthesia was maintained with a combination of sevoflurane and TCI of propofol and remifentanil for approximately 9 hours. Metaraminol infusion was used for blood pressure maintenance. As these drugs were given for the longest period of time, we postulate that they are the potential culprits for precipitating CDI.
The use of [alpha]-1 receptor agonists theoretically could cause cerebral vasoconstriction, but direct effect on cerebral blood flow is not well understood [8]. We are unable to find evidence of any correlation between the use of metaraminol and development of DI
Sevoflurane was chosen as there is a large body of evidence in animal studies to indicate that it provides neuroprotection against ischaemic injury and is better at preserving flow-metabolism coupling of the brain when MAC <1 [9]. There is inconclusive evidence regarding use of sevoflurane in MM patients for revascularisation surgery [10] and no direct correlation between sevoflurane and development of DI.
Propofol and [mu]-opioid agonists have been shown to inhibit AVP release in rats when administered at clinically relevant concentrations [11,12]. There are no human studies to correlate CDI with opioid administration in humans. We identified 2 case reports of CDI associated with propofol administration in humans [13,14].
Both cases reported transient intra-operative CDI during neurosurgery (in patients without MM), associated with administration of intermittent propofol infusion. CDI resolved following cessation of propofol, without the need for DDAVP [13,14] Kassebaum et al postulated that the patient had subclinical CDI which was unmasked by propofol [13] whereas Soo et al speculated that perhaps propofol itself was not the culprit, but rather the mixture other preservative agents mixed with it [14,15] Propofol and/or opioids are potentially a rare cause of CDI and may explain the cause of presumed CDI in this case.
Conclusion
In conclusion, we have described a case of presumed CDI developing during revascularisation surgery for MMS in a patient with SCD, requiring treatment with DDAVP. It is possible that anaesthetic factors caused an exacerbation of underlying chronic subclinical CDI, the most likely culprit being propofol. This is the same conclusion reached by Hong et al. who reported two similar cases of intra-operative CDI in MM patients undergoing revascularisation procedures, both terminated by DDAVP. Optimal choice of anaesthetic agent is still controversial and research is limited by the rarity of the disease. We hope this case report will alert anaesthetists to the potential for development of peri-operative CDI in MM patients undergoing revascularisation surgery.
Conflict of Interest
The author declares none.
Funds Received
The author declares none.
REFERENCES
- Thines L, Petyt G, Aguettaz. Surgical management of Moyamoya disease and syndrome: Current concepts and personal experience. Rev Neurol (Paris) 2015; 171(1): 31-44.
- Parray T, Martin TW, Siddiqui S. Moyamoya disease: a review of the disease and anesthetic management. J Neurosurg Anesthesiol 2011; 23(2): 100-109.
- Hankinson TC, Bohman LE, Heyer G. Surgical treatment of moyamoya syndrome in patients with sickle cell anemia: outcome following encephaloduroarteriosynangiosis. J Neurosurg Pediatr 2008; 1: 211-216.
- Dobson SR, Holden KR, Nietert PJ. Moyamoya syndrome in childhood sickle cell disease: A predictive factor for recurrent cerebrovascular events. Blood 2002; 99(9): 3144.
- Ball SG. Vasopressin and disorders of water balance: the physiology and pathophysiology of vasopressin. Ann Clin Biochem 2007; 44(5): 417-431.
- Fujimura M, Tominaga T. Current status of revascularization surgery for moyamoya disease: Special consideration for its 'internal carotid-external carotid (IC- EC) conversion' as the physiological reorganization system. Tohoku J Exp Med 2015; 236(1): 45-53.
- Kauv P, Gaudré N, Hodel J. Characteristics of moyamoya syndrome in sickle-cell disease by magnetic resonance angiography: an adult-cohort study. Front Neurol 2019;10:15.
- Thiele RH, Nemergut EC, Lynch C. The physiologic implications of isolated alpha (1) adrenergic stimulation. Anesth Analg 2011; 113(2): 284-296.
- Stetler RA, Leak RK, Gan Y, Li P, Zhang F, Hu X, et al. Pre-conditioning provides neuroprotection in models of CNS disease: Paradigms and clinical significance. Prog Neurobiol 2014; 114: 58-83.
- Sato K, Shirane R, Kato M, Yoshimoto T. Effect of inhalational anesthesia on cerebral circulation in Moyamoya disease. J Neurosurg Anesthesiol 1999; 11: 25-30.
- Inoue Y, Shibuya I, Kabashima N, Noguchi J, Harayama N, Ueta Y, et al. The mechanism of inhibitory actions of propofol on rat supraoptic neurons. Anesthesiology 1999; 91: 167-178.
- Soldo BL, Moises HC. mu-Opioid receptor activation inhibits N- and P-type Ca2+ channel currents in magnocellular neurones of the rat supraoptic nucleus. J Physiol 1998; 513: 787-804
- Kassebaum N, Hairr J, Goldsmith W, Barwise J, Pandharipande P. Diabetes insipidus associated with propofol anesthesia. J Clin Anesth 2008; 20: 466-468.
- Soo J, Gray J, Manecke G. Propofol and diabetes insipidus. J Clin Anesth 2014; 26(8): 679-683.
- Hong JC, Ramos E, Copeland CC, Ziv K. Transient Intraoperative Central Diabetes Insipidus in Moyamoya Patients Undergoing Revascularization Surgery: A Mere Coincidence? A Case Rep 2016; 6(8): 224-227.
Citation: Wang S, Lan-Pak-Kee V, Sharma C (2021) Case Report of Possible Intra-Operative Diabetes Insipidus During Cerebral Revascularisation in a Patient with Moyamoya Syndrome.J Surg Anesth. 5:137.
Copyright: © 2021 Wang S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
