Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2019) Volume 16, Issue 1
Breast Tuberculosis: A Case Report
Sara Mai1*, Siham Mansouri1, Nadia Ch’michi2, Manar Rhemimet2, Kaoutar Znati3, Aicha Kharbach2, Karima Senouci1 and Badredine Hassam12Department of Gynecology and Obstetrics, University Hospital Ibn Sina, Rabat, Morocco
3Department of Histopathology, University Hospital Ibn Sina, Rabat, Morocco
Received: 03-Dec-2018 Published: 02-Jan-2019, DOI: 10.4172/2090-7214.1000310
Abstract
Breast tuberculosis (BT) or Tuberculosis mastitis (TM) is a very rare condition that’s not usually obvious to diagnose since it resembles many other conditions especially breast malignant tumor. It usually manifests as an irregular unilateral lump. Radiological findings are nonspecific. Ziehl Neelsen stain, culture and PCR for detection of Mycobacterium tuberculosis are considered as the mainstay for the diagnosis. However, biopsy with epithelioid examination seems to be more sensitive. We report a case of isolated breast localization of tuberculosis in a young female patient.
Keywords
Breast tuberculosis; Female patient
Introduction
Breast tuberculosis is a very uncommon condition even in endemic countries. Its diagnosis can be very challenging since it can easily be mistaken, clinically and radiologically, for a pyogenic abscess or a breast malignancy. We report a case of breast tuberculosis in a young healthy woman.
Case Report
A 45-years-old female patient presented to our department with a 5 months history of painful slowly growing lumps of the right breast that later fistulized to the skin discharging yellowish material.
The patient had no personal medical history but had two grownup sons treated for pulmonary tuberculosis. She had already been treated with antibiotics by several physicians without any obvious improvement. In fact, the mammary masses continued to grow.
Physical examination revealed multiples confluent fixed hard and tender nodules of the central and outer quadrants of the right breast with retracted overlying skin (Figure 1).
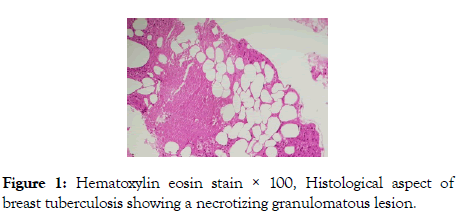
Figure 1: Hematoxylin eosin stain × 100, Histological aspect of breast tuberculosis showing a necrotizing granulomatous lesion.
There were also two small inflammatory periareolar fistulae with yellow seeping exudate and no axillary nodes. A mammography
was performed revealing ill-defined masses in the central and
outer quadrants of the right breast with very dense breasts. The
ultrasound examination showed heterogeneous solid masses
with abscessed areas connected to the skin by fistulae. A core
biopsy was then performed and histological examination showed
a granulomatous lesion with a great number of langhan’s cells
and areas of caseating suggestive of tuberculosis. Culture of the
material of the discharge from the fistula was also found positive
to Mycobacterium tuberculosis. The patient was treated with
antibacillar chemotherapy using the therapeutic regiment
recommended in Morocco which is 2 months of rifampicin, isoniazid, pyrazinamide and thambutol followed by 4 months
of rifampicin and isoniazid (Figure 1).
Discussion
Tuberculosis mastitis (TM) is the less frequent localization of extrapulmonary tuberculosis. The first case was reported by Astley Cooper in 1829 [1]. Its incidence is variable. It ranges from 0.1% in developed countries to 4.5% in India [2,3]. In North Africa the incidence of TM is about 0.4% [4]. It occurs far more often in women, especially in reproductive age, multiparous and lactating [3]. However, it can exceptionally affect older women or young men [2].
The rare incidence of this particular localization is mainly due to the fact that breast tissue is a particularly hostile environment for the Mycobacterium tuberculosis [2]. The most common clinical presentation of tuberculous mastitis is a solitary, ill-defined, unilateral hard lump of the central or upper outer quadrant. The lesion may be indistinguishable from breast carcinoma, being irregular, hard, and sometimes, fixed to either skin or muscle or both. Multiple and bilateral localizations are possible. It may also manifest as skin ulcerations in late stages or as breast abscess with or without discharging sinuses. Our patient had both hard tumefactions and fistulized abscesses.
Tuberculous infection of breast is either secondary, via lymphatic, hematogenous, or contiguous contamination from adjacent structures (lung, pleura); or primary, after direct inoculation of the bacilli through abrasions in the nipple [5]. Lymphatic retrograde transmission seems to be the most frequent way of breast contamination since many patients with breast tuberculosis have also lymph node involvement [3,5,6]. Direct Inoculation is rare and usually occurs in lactating women. Our patient had no axillary nodes and no pulmonary infection. The way of transmission in this case remains unknown [7].
Imaging findings in TM are nonspecific. It usually presents as an irregular mass on mammography and as a heterogeneous hypoechoic mass on ultrasound examination. There are three main radiographic subtypes: nodular, disseminated, and sclerosing [8]. Although highly specific for the diagnosis, M. tuberculosis stain, culture or PCR are not very sensitive. In fact, bacilli are isolated in only 25% of patients with tuberculous mastitis as the lesions are for the most paucibacillary (Figure 2). Histopathological examination is very useful for the diagnosis of TM, as it can reveal the granulomas associated with the typical caseous necrosis. Core biopsy should be preferred to fine-needle aspiration [9]. The treatment of breast TM is based on medical antituberculous therapy usually associating many antibacillar treatments for a long period, typically 6 months. The prognosis is excellent after treatment [10].
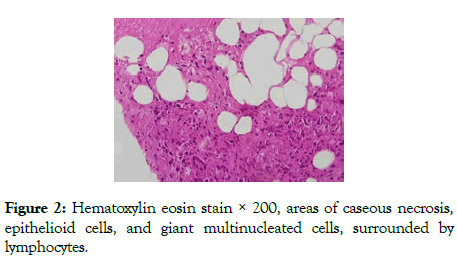
Figure 2: Hematoxylin eosin stain × 200, areas of caseous necrosis, epithelioid cells, and giant multinucleated cells, surrounded by lymphocytes.
Conclusion
Breast tuberculosis is a very rare condition that can easily be mistaken for a breast carcinoma. A better awareness of this condition may prevent unnecessary treatments and surgical procedures.
REFERENCES
- Cooper A. Illustrations of the Diseases of the Breast, Longman, Rees, Orme, Brown and Green, London.
- Thimmappa D, Mallikarjuna MN, Vijayakumar A. Breast tuberculosis. Indian J Surg 2015;77:1378-1384.
- Kilic MO, Saglam C, Ağca FD, Terzioğlu SG. Clinical, diagnostic and therapeutic management of patients with breast tuberculosis: analysis of 46 cases. Kaohsiung J Med Sci. 2016;32:27.
- Direction des soins de santé de base, Ministère de la Santé publique. République tunisienne. Bull Epidemiol. 2001;23:9.
- Efared B, Sidibé IS, Erregad F, Hammas N, Chbani L. Breast tuberculosis: a report of five cases. Trop Med Health. 2017;45:40.
- Da Silva BB, Lopes-Costa PV, Pires CG, Pereira-Filho JD, dos Santos AR. Tuberculosis of the breast: analysis of 20 cases and a literature review. Trans R Soc Trop Med Hyg. 2000;103:559.
- Marinopoulos S, Lourantou D, Gatzionis T, Dimitrakakis C, Papaspyrou I. Breast tuberculosis: Diagnosis, management and treatment. Int J Surg Case Rep. 2012;3:548.
- Longman CF, Campion T, Butler B, Suaris TD, Khanam A. Imaging features and diagnosis of tuberculosis of the breast. Clin Radiol 2017;72:217.
- Strazzanti A., Trovato C, Gangi S, Basile F. Breast tuberculosis cases rising in Sicily. Int J Surg Case Rep. 2018;53:9.
- Jalali U, Rasul S, Khan A, Baig N, Khan A. Tuberculous mastitis. J Coll Physicians Surg Pak. 2005;15:234.
Citation: Mai S, Mansouri S, Ch’michi N, Rhemimet M, Zanti K, Kharbacha A, et al. Breast tuberculosis: a case report. Clinics Mother Child Health. 2019;16:310.
Copyright: © 2019 Mai S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

