Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2023) Volume 9, Issue 1
Atresia of the Infrarenal Inferior Vena Cava in an Adolescent Presents with Bilateral Deep Vein Thrombosis
Tushar Menon1, Ameera C Mistry2*, Shahin Bhagwagar1 and Rahul Malhotra32Independent Researcher, International American University College of Medicine, Vieux Fort, Saint Lucia, USA
3Department of Cardiology, Abrazo Health Network, Glendale, AZ, USA
Received: 25-Jan-2023, Manuscript No. JTCOA-23-19960; Editor assigned: 30-Jan-2023, Pre QC No. JTCOA-23-19960 (PQ); Reviewed: 13-Feb-2023, QC No. JTCOA-23-19960; Revised: 20-Feb-2023, Manuscript No. JTCOA-23-19960 (R); Published: 28-Feb-2023, DOI: 10.35248/2572-9462.23.9.201
Abstract
Atresia of the Inferior Vena Cava (IVCA) is a rare congenital vascular anomaly that can predispose patients to venous stasis and thrombotic events like Deep Vein Thrombosis (DVT). Young patients with IVCA may be asymptomatic until provoked by another risk factor, such as Oral Contraceptives (OCPs) use, hypercoaguable states, surgery, trauma, and immobilization. Here we present a young female patient with a history of OCPs and marijuana use, and no other relative risk factors, which presented with signs and symptoms of a DVT. Further investigation revealed previously undiagnosed IVCA. Typically, the relative risk for thrombotic events in healthy, young patients is low when using OCPs. In young, healthy patients with new or extensive thrombotic events that have few risk factors and no personal or family history of inherited thrombophilia’s, further investigation and careful testing and imaging should be prompted, as structural anomalies like IVCA may be present.
Keywords
Deep vein thrombosis; Inferior vena cava; Vascular atresia; Atresia of the inferior vena cava; Thrombectomy
INTRODUCTION
Atresia of the Inferior Vena Cava (IVCA), also known as IVC agenesis or aplasia, is a rare vascular anomaly with an estimated prevalence of 1% in the general population [1]. While Deep Vein Thrombosis (DVT) in young patients is most often associated with risk factors like congenital or acquired thrombophilia, autoimmune diseases, neoplasms, pregnancy, OCPs use, or prolonged immobilization and trauma; IVCA is found in approximately 5% of cases of unprovoked lower extremity DVT in young adults (<30 years old) [2,3].
Case Presentation
A 19 year-old female patient, with a history of Pre Menstrual Syndrome (PMS) on OCPs, presented to the emergency department with right leg swelling and tenderness for 3 days that worsened over the course of 12 hours. The patient reported right leg pain that worsened with movement, located primarily in the back of her calf. Significant medical history included a recent pilonidal cyst removal and immobilization 4 weeks prior, and an increase in OCP dose 2 years ago. She admitted to occasional marijuana use weekly. She denied weakness or tingling of the right leg, chest pain, breathing difficulty, lightheadedness, dizziness, a past history of blood clots, or any family history of inherited thrombophilia.
The patient’s vitals were stable on admission. She had a markedly enlarged Right Lower Extremity (RLE) from hip to foot, with notable induration at the thigh. She also had a positive Homan’s sign and slightly darker color of her RLE compared to the contralateral Left Lower Extremity (LLE). No mottling or red, purple, or white discoloration was noted. Ultrasound (U/S) of the RLE was performed and revealed an extensive thrombus in the common femoral vein, superficial femoral vein, and the thrombus was partially imaged in the superior deep femoral, popliteal, posterior tibial, and great saphenous veins. Initial Computed Tomography Angiography (CTA) ruled out a Pulmonary Embolism (PE).
Interventional cardiology had planned for an Inari ClotTriever thrombectomy, with access through the right popliteal vein. A venography revealed an occlusion of the right popliteal and femoral veins, occlusion in the left common iliac vein extending from the common femoral vein to the proximal left external iliac vein, tortuous and dilated azygos system, and thrombus in lumbar accessories, as well as a congenitally absent Inferior Vena Cava (IVC). We considered catheter-based thrombectomy initially; however, due to the small caliber of the femoral and popliteal veins, we were unable to utilize the Inari ClotTriever. At that time, anticoagulation therapy with Lovenox was continued. CT with contrast of the chest, abdomen, and pelvis was utilized to optimally define what appeared to be anomalous anatomy (Figures 1, 2 and 3). Patient’s CT delayed phase venography revealed an extensive clot in the right lower extremity as described on venous U/S. Contralaterally, the LLE exhibited a significant clot from the inferior external iliac vein to the confluence of the iliac veins. IVC was found to be absent at the level of the common iliac vein confluence to just below the renal veins.
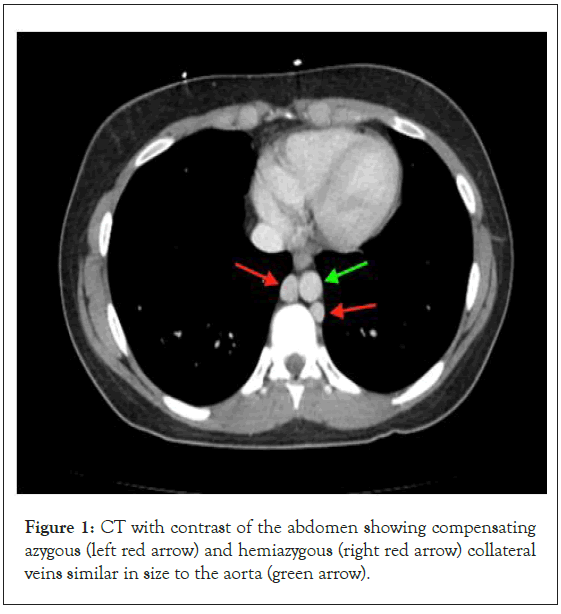
Figure 1: CT with contrast of the abdomen showing compensating azygous (left red arrow) and hemiazygous (right red arrow) collateral veins similar in size to the aorta (green arrow).
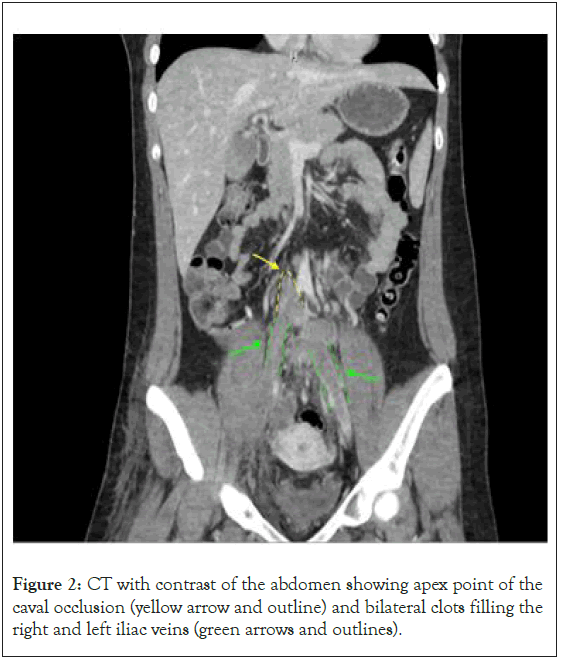
Figure 2: CT with contrast of the abdomen showing apex point of the caval occlusion (yellow arrow and outline) and bilateral clots filling the right and left iliac veins (green arrows and outlines).
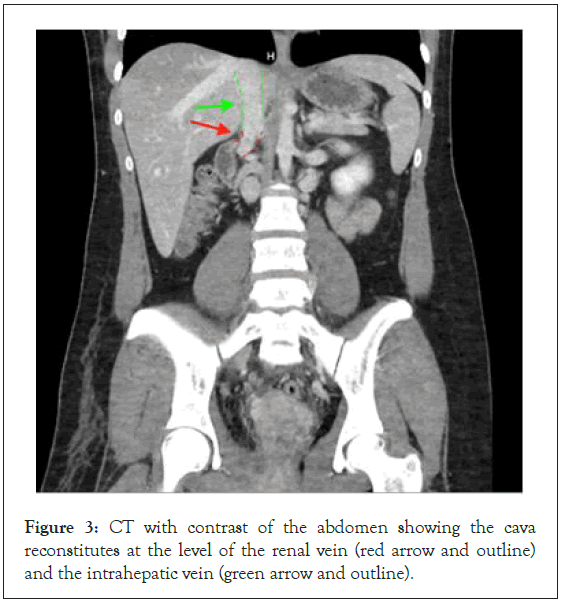
Figure 3: CT with contrast of the abdomen showing the cava reconstitutes at the level of the renal vein (red arrow and outline) and the intrahepatic vein (green arrow and outline).
Treatment was initiated with Ekosonic Endovascular System (EKOS) catheter directed acoustic pulse wave thrombolysis of the left common iliac vein, right iliofemoral vein, and accessory IVC; with continuous IV alteplase and heparin drip. Following the procedure, a bilateral iliofemoral venography revealed overall improved straight-line flow. The right iliofemoral thrombus was markedly resolved and the right accessory vein showed improved flow. The left common iliac vein showed improved flow, despite persistence of the thrombus, with a decrease in volume extending into the proximal external iliac vein. Ultimately, the EKOS acoustic pulse thrombolytic system was removed, and treatment preceded with pharmacomechanical thrombectomy with Zelante AngioJet of the right popliteal and right iliofemoral veins. Right common femoral vein with right leg iliofemoral venography revealed significant resolution. There was markedly improved flow in the right popliteal, femoral, and accessory veins. Although there was improved flow, a partially occluding thrombus in the right deep venous system, including the right iliofemoral segment, remained. The left iliofemoral venography showed improved rate line flow and near complete resolution of the thrombus in the left common iliac vein.
EKOS catheter placement with acoustic pulse wave thrombolysis with TPA and pharmacomechanical thrombectomy with Zelante AngioJet resulted in removal of about 80% of the clot burden. The patient was transferred back to the ICU where she remained thermodynamically stable over a 24-hour period and was then cleared for discharge. She was transitioned from IV heparin to full dose subcutaneous Lovenox, followed by Eliquis. Lifelong anticoagulation was recommended to the patient, as the IVCA predisposes her to venous stasis and future thromboembolism. The patient was educated on medical consultation for future pregnancy and avoidance of birth control and cigarette smoking.
Results and Discussion
Atresia of the IVC can be congenital or acquired and is related to embryonic dysgenesis or thrombosis during the intrauterine or perinatal period [2,4]. At 4-8 weeks of gestation, the IVC develops from the fusion of the posterior cardinal, sub cardinal and supra cardinal veins [5]. Absence of the infra renal IVC, as seen in our patient, results from failure of development of the posterior cardinal and supra cardinal veins, with preservation of the suprarenal segment of the IVC [6]. In total absence of the infra renal IVC, increased venous flow is compensated by the collateral azygos and/or hemiazygous systems [7]. Over time, the collateral venous system is unable to meet the demands of increased blood flow resulting in overflow and stasis [8]. Venous stasis predisposes patients to DVT and a variety of other clinical sequelae, such as lower extremity venous insufficiency or Pelvic Congestion Syndrome (PCS). Phlegmasia Cerulea Dolens (PCD) is another complication of acute, massive venous thromboembolism, as seen in our patient [9,10]. PCD is a life-threatening manifestation of DVT that can lead to critical limb ischemia, gangrene, and limb loss, without acute and aggressive intervention [9].
Many young adults with IVCA are asymptomatic unless provoked by another risk factor (estrogen oral contraceptives, pregnancy, cancer, smoking, high-impact exercise, hypercoagulability, surgery, trauma, and immobilization) [11]. The relative risk of a thrombotic event in a patient using combined OCPs is three to five-folds; however, the absolute risk decreases to only 0.05% per year for a healthy adolescent on this therapy [12]. Inherited thrombophilia is the most commonly observed risk factor for developing lower extremity thrombosis among patients younger than 50 years [13]. In young patients with extensive thrombotic events without a personal or family history of hypercoagulopathy, further questioning should be prompted, as the relative risk for such events with OCPs alone is minimal.
Our patient was previously diagnosed with PMS at a young age and treated with OCPs. She admitted to regular marijuana use for PMS, which leads us to ask if this too, was a precipitating factor to a hypercoagulable state. The subject has been poorly investigated; however, recent data points to Tetrahydrocannabinoids (THC) use as placing patients at an increased risk for Thromboembolic Complications (TECs), such as DVT in patients with trauma [14]. A smaller study also indicated that marijuana exposure increased enzymatic and platelet-based clot formation as well as relative thrombocytosis [15]. We considered the patient a subject of trauma due to her recent surgery, however, studies were not clear as to the time frame or the magnitude of trauma that places patients at a higher risk for TECs. It is important to consider each risk factor individually, as well as all factors combined. Our patient exhibited both IVCA in addition to two risk factors that have been well described in the literature: recent surgery immobilization and estrogen-containing oral contraceptive use. Here, we note the synergistic effects of IVCA, surgical immobilization, OCPs, and medical marijuana as predisposition for development of a DVT.
Conclusion
After initial diagnostic work up of common hyper coagulation abnormalities, other risk factors such as IVC anomalies must be considered as a possible differential diagnosis in the adolescent patient. Despite its rarity, thrombosis secondary to IVC anomalies is a well-defined cause of bilateral lower extremity DVTs, especially in young adults (<30 years old). The diagnosis of IVCA poses a clinical challenge and requires detailed imaging studies. In this case, the patient required extensive pharmacomechanical therapy including acoustic pulse wave thrombolysis and Zelante AngioJet technology. The patient must adhere to lifelong anticoagulation with avoidance and careful consideration of risk factors such as smoking, estrogen containing oral contraceptives, and pregnancy to reduce risk of future thrombotic events.
Conflict of Interest
All authors agree for the publication. For all authors, there are no competing interests to declare.
References
- Eifert S, Villavicencio JL, Kao TC, Taute BM, Rich NM. Prevalence of deep venous anomalies in congenital vascular malformations of venous predominance. J Vasc Surg. 2000;31(3):462-471.
[Crossref] [Google Scholar] [PubMed]
- Mustafa HM, Muhamad H, Abdulfaraj A. Absent inferior vena cava with recurrent deep venous thrombosis. Int J Vasc Surg Med. 2015;(1):1-3.
- Obernosterer A, Aschauer M, Schnedl W, Lipp RW. Anomalies of the inferior vena cava in patients with iliac venous thrombosis. Ann Intern Med. 2002;136(1):37-41.
[Crossref] [Google Scholar] [PubMed]
- Ramanathan T, Hughes TM, Richardson AJ. Perinatal inferior vena cava thrombosis and absence of the infrarenal inferior vena cava. J Vasc Surg. 2001;33(5):1097-1099.
[Crossref] [Google Scholar] [PubMed]
- Koppisetty S, Smith AG, Dhillon RK. Incidental finding of inferior vena cava atresia presenting with deep venous thrombosis following physical exertion. Case Rep Emerg Med. 2015;2015:1-4.
[Crossref] [Google Scholar] [PubMed]
- Petik B. Inferior vena cava anomalies and variations: imaging and rare clinical findings. Insights Imaging . 2015;6:631-639.
[Crossref] [Google Scholar] [PubMed]
- Ghandour A, Partovi S, Karuppasamy K, Rajiah P. Congenital anomalies of the IVC-embryological perspective and clinical relevance. Cardiovasc Diagn Ther. 2016;6(6):482-492.
[Crossref] [Google Scholar] [PubMed]
- Lambert M, Marboeuf P, Midulla M, Trillot N, Beregi JP, Mounier-Vehier C, et al. Inferior vena cava agenesis and deep vein thrombosis: 10 patients and review of the literature. Vasc Med. 2010;15(6):451-459.
[Crossref] [Google Scholar] [PubMed]
- Gardella L, Faulk J. Phlegmasia alba and cerulea dolens. StatPearls [Internet]. 2022.
- Morita S, Higuchi M, Saito N, Mitsuhashi N. Pelvic venous variations in patients with congenital inferior vena cava anomalies: classification with computed tomography. Acta Radiol. 2007;48(9):974-979.
[Crossref] [Google Scholar] [PubMed]
- Muscianese L, Seese RR, Graham W, Williams JH. Congenital atresia of the inferior vena cava and antithrombin III deficiency in a young adult: compounding risk factors for deep vein thrombosis. BMJ Case Rep. 2015;2015:bcr2014205729.
[Crossref] [Google Scholar] [PubMed]
- Trenor III CC, Chung RJ, Michelson AD, Neufeld EJ, Gordon CM, Laufer MR. Hormonal contraception and thrombotic risk: A multidisciplinary approach. Pediatrics. 2011;127(2):347-357.
[Crossref] [Google Scholar] [PubMed]
- Kreidy R, Salameh P, Waked M. Lower extremity venous thrombosis in patients younger than 50 years of age. Vasc Health Risk Manag. 2012;161-167.
[Crossref] [Google Scholar] [PubMed]
- Stupinski J, Bible L, Asmar S, Chehab M, Douglas M, Ditillo M, et al. Impact of marijuana on venous thromboembolic events: Cannabinoids cause clots in trauma patients. J Trauma Acute Care Surg. 2020;89(1):125-131.
[Crossref] [Google Scholar] [PubMed]
- Carter K, Patki D, Kutcher M. 1742: Marijuana exposure is associated with hypercoagulability after injury. Crit Care Med. 2019;47(1):844.
Citation: Menon T, Mistry AC, Bhagwagar S, Malhotra R (2023) Atresia of the Infrarenal Inferior Vena Cava in an Adolescent Presents with Bilateral Deep Vein Thrombosis. J Thrombo Cir. 9:201.
Copyright: © 2023 Menon T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
