Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research - (2021) Volume 7, Issue 6
Analyzing COVID-19 infection clusters formed when dining together using a time-Workflow Chart
Hitoshi Tsuchiya*, Taniguchi Anna, Hideki Kato, Tsugunori IWAI, Hiroki Saito and Masayuki KoikeReceived: 16-Nov-2021 Published: 07-Dec-2021, DOI: 10.35248/2573-4598.21.7.177
Abstract
Background and purpose: COVID-19 has caused serious damage globally. Some countries implemented short-term lockdowns to slow down the spread of COVID-19 while continuing basic economic activities; vaccinations have also been underway, but a significant impact of vaccinations is yet to be seen. In reality, infections continue to increase at a slow pace.
Although lockdowns and rules for limited operating hours for restaurants were implemented, infection clusters originating from restaurants still occur. Recently, clusters originating in families have also occurred. The present study attempts to analyse the specific causes of such infection clusters.
Method: In a group, infection through airborne droplets during conversation is possible. When dining in a group, most people do not put their masks back on later, which is clearly a ‘rule violation’. Therefore, the actual conditions of such instances were investigated using a time workflow chart (t-WFC), analyses of COVID-19 infection clusters were carried out, and countermeasures were proposed.
Results: There is no guarantee that dining in a group does not lead to infection. Consequently, in such instances one should wear a mask to prevent infection. Additionally, the efficacy of masks varies according to their type. Therefore, masks that are more effective should be used. Several rules should also be considered when dining together, such as maintaining social distancing and reducing the number of participants.
Conclusion: The misconception that individuals dining together are not infected with COVID-19 should be corrected.
Keywords
COVID-19; Cluster trials; Continuous quality improvement; Root cause analysis
Introduction
COVID-19 has caused serious damage globally. Certain efforts to control growing infection rates may have an uncertain impact on economic activities [1,2]. For instance, a second lockdown was imposed in some European countries leading to a decrease in economic activities and an increase in the following recovery time. Consequently, many countries cut their lockdown periods short, attempting to reduce its adverse impact on economic activities.
The initial symptoms of COVID-19 are now well known: slight fever, cough, fatigue, and cold-like symptoms. However, mild symptoms are seen only in some cases. Therefore, asymptomatic individuals can spread the virus without knowing whether they are infected.
The second and third waves of COVID-19 have exceeded their forecasts. Across the world, many people wear masks [3] to prevent infection, yet the virus continues to spread. This begs the question ‘Could there be other reasons?’
Problem
Generally, everyone entering a restaurant is required to wear a mask. Yet, when customers dine together, they remove their masks and do not always put them back on. If members of a group are not infected, this does not cause a problem, but identifying who may or may not be infected is not possible beforehand. It is therefore reasonable to consider that any person could be a carrier, who is still in the virus incubation period and unaware that he/she is infected. Considering this condition, removing the mask at the restaurant would be against the rules. Yet, hardly anyone wears a mask while dining in public and restaurants remain open even when infections may occur through the spread of airborne droplets during eating and drinking.
Ailake knowledge
Root cause analysis (RCA) was used to examine whether dining in a group results in COVID-19 infection clusters. Moreover, a time-workflow chart (t-WFC) was created [4,5]. This method was first adopted by the aviation industry and has also been used in the analysis of medical accidents in recent years. Generally, the workflow chart used in RCA involves simply aligning events sequentially. However, identifying potentially hazardous occurrences using only RCA is difficult. Therefore, instead of focusing only on potentially hazardous events, the possible scenarios that could occur were also carried out. Specifically, the time of the event was noted, along with all other observable details.
It is not possible to establish countermeasures by analysing COVID-19 infection clusters using only the t-WFC. However, a ‘Why Diagram’ based on the results of the t-WFC could be used to generate hypotheses regarding significant questions such as: Why did an individual take off their mask? How long did the mask stay off? Why did the mask stay off after eating and conversing with others? Why did no one point this out? According to the Socratic method [6, 7], it is possible to distinguish between valid and invalid hypotheses by repeatedly asking questions that cannot be answered with a simple yes or no.
Design
First, it was presumed that the spread of COVID-19 could be controlled by wearing a mask [8-10]. Although even while wearing a mask at work, there is an increasing likelihood of being infected during company operations and conferences. This spread is likely because of workers removing their masks to eat or to converse during a meal (e.g. lunch). Wearing a mask is a generally preventive measure, but frequently removing it and putting it back on reduces its efficacy.
A state of emergency was declared, since controlling the spread of infection when dining in a group was difficult. Restaurants closed and the economy stagnated. In order to reactivate the economy and be able to open up restaurants again, some important questions need to be examined:
1) Can asymptomatic individuals infect healthy people?
2) Are all types of masks and face shields equally effective?
3) Why do some people get infected, even though they wear masks?
4) Is it a mistake to think that wearing a mask can control infection?
5) Are there any other factors, which increase the infection rate?
Although it has been stated that a cluster will not occur if wearing a mask is mandated, infections continue to grow through the food and drinks industry, mainly because people remove their masks while dining. This is an example of a rule violation caused by human errors. This non-medical issue has not yet been addressed using RCA. Given the public concern regarding the death toll crossing thousands due to COVID-19, infection clusters should be analysed and research-based countermeasures should be proposed.
We considered establishing a countermeasure plan focusing on non-infected people because 1) asymptomatic persons do not inherently want to infect healthy people, and 2) non-infected persons do not consider the possibility that the other people dining with them could be infected.
RCA and t-WFC were used to analyse human error with five individuals who enjoyed drinking parties. However, a drawback in this case analysis is that a strong desire for justice has gained mainstream importance and loses the pleasure of justice. As a last resort, we decided to ‘set penalty rules for restaurants that did not adopt prevention measures’, or ‘set penalty rules when an asymptomatic person causes a cluster by dining in a group.’ To avoid this, our analyses periodically changed the targeted members (e.g. men, women, and people who do not drink alcohol).
Case Study
1. The case study evaluated COVID-19 infection clusters related to dining in groups in Japan.
2. Course of the case
Four co-workers of a company (A [boss], B [vice-president], C [employee], and D [employee]) were targeted. All of them reported wearing masks: Mr. A and Mr. B wore urethane masks, and Mr. C and Mr. D wore non-woven (surgical) masks. After a work conference, the subjects decided to eat at a restaurant that was not crowded. When they entered the restaurant, the waiter, who wore a mask, guided them to a table for four people. They sat 60 cm in front of each other and 30 cm adjacent to each other. Once the food and drinks were served, everyone took off their masks and made a toast. After the toast, they did not put their masks back on. They stayed at the restaurant for approximately 2 h and then went their separate ways.
3. Report from participants
Four days after the group meal, Mr. A reported that he lost his sense of taste. Two days later, he had a high fever, went to the hospital, and tested positive for COVID-19. Given that he had participated in another group meal three days before dining with his co-workers, the source of COVID-19 infection could not be ascertained. Regarding other members, he commented that ‘someone other than me may have been infected’.
4. Comments and reflections from the other three participants in the group:
‘I did not think that Mr. A was infected with COVID-19. He came to work the next day without any problems, and no one else was infected in the workplace’. In addition, a test to determine where he contracted COVID was conducted, and all his co-workers were found to be infected as well (they were asymptomatic).
They wore a mask before they started to eat because they were concerned about getting infected. They took off their masks to eat and drink. Although they were all aware of social distancing, they did not think of applying it between themselves. They were not worried about getting infected because they were more than 1 m away from people other than their own group. They also did not think that someone in their own group would be infected.
5. Comment from the restaurant chef
The restaurant was not crowded at that time. I had instructed the staff ‘to not have long conversations with customers’ [11].
Methods
Step 1. The date and length of time spent dining were recorded in the workflow chart on the horizontal axis. Each participant who joined a group meal filled up the upper row to create the overall flow chart image.
Step 2. Deviation from the overall flowchart image (risk during group meals): conditions during group meals were recorded. Confirmation: Any changes in the procedures of the group meals were added into the flowchart, along with reasons (including information from interviews with COVID-19 carriers). The time zone when the risk carriers are thought to be infected were shown as (✕), and the actual time of COVID-19 infection was shown as (✸). The two were then connected with a straight line. Time zones in which the risk carrier’s health is observably the same as the non-infected people (incubation period) are shown as a dotted line; time zones in which the person starts feeling unusual about their physical condition is shown as a solid line. If the condition of the infected carrier patient gradually worsens due to the effect of infection, this can be identified by changing the thickness of the arrow ( ->). The model diagram is shown in Figure 1.
Step 3. Analysis of potential risk factors at group meals was conducted: The participant was asked to check the “during group meals” report, and confirm and acknowledge the details of the status of their infection.
Step 4. Cognitive psychological factor analysis was conducted: The cognitive and psychological factors of the risk carriers and meal participants were included.
Step 5. Based on the emerging principles from analysis of the “Group Meals Flow Chart”, countermeasures were developed. The participant was asked to determine the cause of the improper behaviour, communication, and environment, etc., recreate the “Why Diagram”, and develop a countermeasures- proposal [12].
Step 6. Review of the countermeasures-proposal for group meal times: the participant verifies the proposal using the Why Diagram.
Step 7. Countermeasure suggestions for group meals: participants shall verify new risks, which can be predicted in the future, and consider the prevention results. A model chart is shown in Figure 1. (Figures 1 and 2)
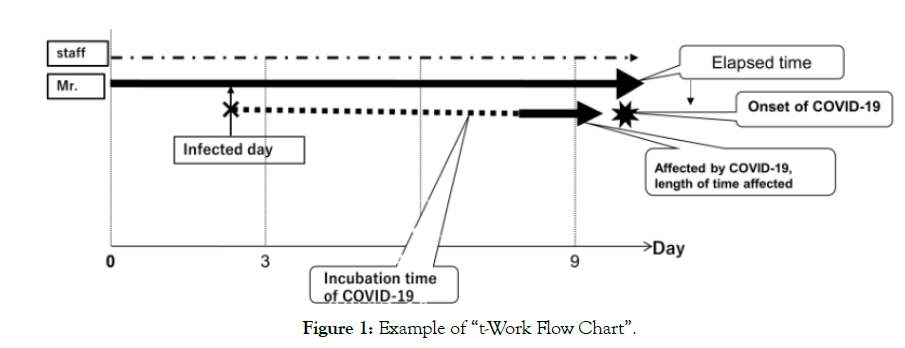
Figure 1: Example of “t-Work Flow Chart”.
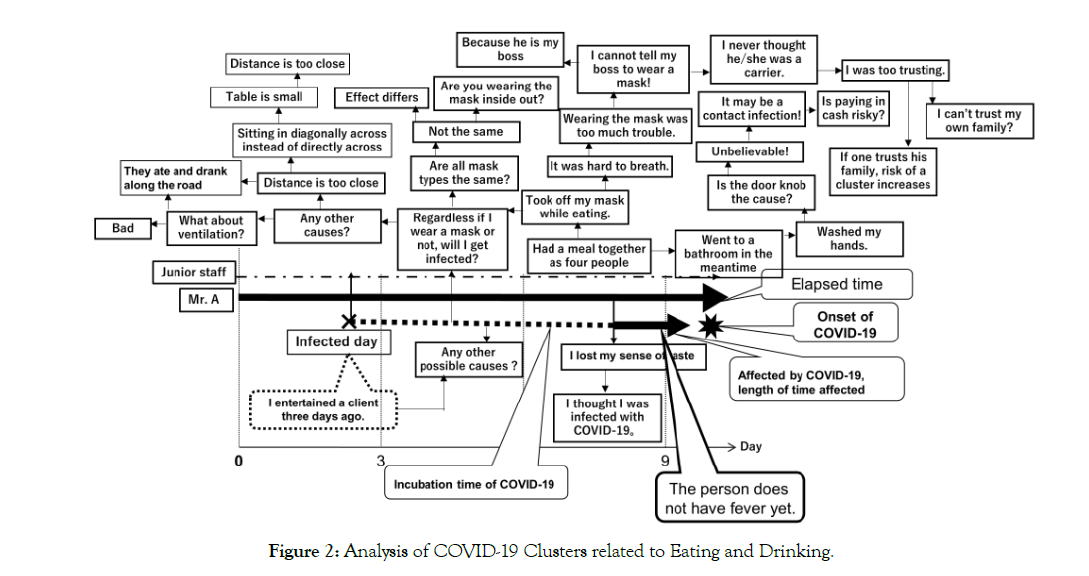
Figure 2: Analysis of COVID-19 Clusters related to Eating and Drinking.
Results
Figure 2 shows the results of the analysis of the COVID-19 infection clusters related to dining in restaurants.
Four company workers who dined together were targeted. Their activities were organised in the order of time and date sequence according to the t-WFC, and the progress of each person was displayed. Next, the Why diagram from the t-WFC was created, and a countermeasures- proposal was presented.
Countermeasures- Proposal based on the Analysis Result
1) Many countries have been concerned about an economic downturn and have restricted the operating hours of restaurants to reduce the risk of infection. However, when an infected person participates in a group meal, infection clusters can be generated, especially when the carrier is asymptomatic and unaware of infection. According to studies from various Asian countries, including China, transmission from an infected person to others is said to increase on the second and third days after infection, and then decreases within 7 days. In other words, even if a person is asymptomatic, he or she can still transmit the virus. At the same time, reports of transmission from a person during the incubation period are rare [13].
One countermeasure when participating in group meals is that one should operate on the assumption that everyone is infected with COVID-19. Hence, one should be sure to wear a mask while conversing, to avoid infection by airborne droplets, and ask others to do the same.
2) Types of masks
The efficacy of a mask varies depending on its type [14]. Excluding medical staff masks, nonwoven (surgical) masks are more effective (discharged airborne droplet amount and inhaled droplet amount = 20 %–30%) [15]. However, mistakenly wearing a mask inside out greatly reduces its efficacy. The amount of discharged airborne droplets from a fabric mask is 18%–34%, the inhaled droplet amount is 55 %–65%, and the efficacy of the urethane mask is 50%. Regarding mouth shields, more than 80% of both discharged airborne droplets and inhaled airborne droplets have been reported during their usage, making them ineffective in preventing the spread of small airborne droplets. Hence, wearing a mouth shield while cooking and providing food services is not effective.
3) Social distancing
At a conference, people wear masks and maintain social distancing of approximately 1 m. However, the dining conditions are not the same as those in a conference room. A sophisticated restaurant might have a table wide enough to maintain the distance between people. However, in places such as bars, the tables are smaller and social distancing is not possible, increasing the risk of infection.
4) Air conditioning and humidity in restaurants
Detailed consideration of air conditioning and humidity in restaurants is required. This is not limited to COVID-19 cases but it also applies to influenza.
5) Hand washing, handling smartphones, and cash while dining.
People use soap and antiseptic solutions to wash their hands while dining, but this is ineffective if they touch the faucet and other surfaces afterwards. The restaurant staff will sanitize surfaces before opening the restaurant, but if a carrier is exposed to them, the surfaces can still be a source of infection. Instead of using restaurant facilities, a compact antiseptic solution is recommended when eating out. Moreover, handling a smartphone with hands that have touched various surfaces should be avoided. Even if all of the above risk countermeasures are followed, if a person touches his coat with their own hands, the risk of infection automatically increases.
Discussion
Symptoms of COVID-19 are now well known, including fever, cough, and fatigue, and they are similar to the initial symptoms of the common cold. In some cases, the symptoms do not appear or are very mild. However, in many cases, the infected person develops pneumonia, conditions rapidly deteriorate, and the infected person dies. According to previous studies, persons with pre-existing medical conditions and the elderly are reported to be at a higher risk of infection and the infection developing into a severe case. There is also a report about asymptomatic infected persons (carriers) spreading infection, constituting a factor that has made prevention difficult.
We developed a t-WFC on the themes of dining in a group and the results have yielded pertinent aspects for further consideration of countermeasures.
1. COVID-19 clusters are related to dining in a group.
The misconception that those who dine within a group are not infected with the virus should be corrected. Dining with others at a work event, for example, is not the same as working with others inside a company building. Conference rooms are typically large, with good infrastructure. Therefore, social distancing can be maintained easily. The humidity of the air conditioning is generally set at approximately 60%. In addition, people do not hold discussions while taking off their masks. For these reasons, infections do not occur easily in the workplace. However, close attention should be paid to work events involving dining with coworkers.
2. Time, distance, and the number of people dining together must be considered.
Health guidelines have established that group meals should be limited to a maximum of five people and should last less than 2 h, but there is no evidence proving that these rules prevent the spread of the virus. Indoor and outdoor cases should be handled differently: in outdoor settings, it is possible to maintain social distancing freely and are thus considered safe.
3. Sterilization of restaurants
Restaurants are typically cleaned before opening up. However, even if the restaurant staff sterilises the tables and doors, if the next person who touches them is a carrier, such cleaning is of no use. Even if a client washes his/her hands, he may get infected by touching the door or other surfaces. Moreover, leaving their belongings on the floor also may result in taking the virus home. Similarly, many people often drop their smartphones, pick them up, and continue to use them. This can also be dangerous.
4. Ventilation and humidity inside a restaurant
Some restaurants leave the entrance door open for ventilation. In spite of this, often there is no good airflow, which again increases the risk of virus transmission. Instead, it is better to ensure good airflow by using a ceiling fan or an air cleaner.
5. Presence of the leader
Neither the president nor the vice-president of the company should participate in group meals at work. If both are infected with COVID-19, the company cannot operate.
6. Familial infection (cluster)
Outside the workplace, the company’s president and other workers also have families who can also be at risk of contracting the COVID-19 infection. It is not typical for people to wear masks while eating with their families.
However, similar to group meals, children too can contract the virus at school or in the park. While one might feel safe with one’s own children, it is better to assume that anyone could be infected, including our own family members. If this is not possible, strict management of body conditions should be exercised. Even if a small change is noticed in one’s body condition (e.g. loss of taste, joint pain, slight fever), isolation from others should take place.
Limitations
The results and countermeasures for COVID-19 clusters may not apply to all cases of eating together. For example, as a countermeasure for COVID-19, how large a table should be considered safe? Since social distancing of 1 m has been recommended, would a table of 1.1 m be sufficient? In addition, although unwoven masks are said to have limitations, and manufacturers are expected to make masks that are more effective in the future, currently there is no accurate method of evaluating this aspect.
As suggested in the discussion, maximum attention must be paid to mask efficacy and social distancing. This is especially important because COVID variants may overpower current countermeasures.
Conclusion
Eating and drinking are essential behaviors in human life, but doing so as a group is not. In order to prevent infections and live a new daily life, the use of more effective masks and when not eating and drinking alone, the three C’s (Closed spaces, Crowded areas, and Close contact settings) should be avoided. In addition, persons who live with their family need to understand the risk of eating and drinking together.
REFERENCES
- Guerrieri V, Lorenzoni G, Straub L, Werning I. Macroeconomic implications of COVID-19: Can negative supply shocks cause demand shortages?. National Bureau of Economic Research. 2020
- Atkeson A. What will be the economic impact of COVID-19 in the US? Rough estimates of disease scenarios. National Bureau of Economic Research.2020
- Tsuchiya H, Kurosaki H, Hiramoto S, Seki M, Moriuchi K, Kawauchi S et al. Analysis of medical accidents using the" Why Analysis"(questions):comparison with conventional analytical techniques. Jpn. J. Radiol. 2005;61(12):1638-44.
- Tsuchiya H. Assisting beginners in root cause analysis operations: analysis and recommendations regarding the spread of COVID-19 in nursing facilities for the elderly. BMJ Open Quality. 2020;9(3):e000960.
- Benson HH. Socratic wisdom: the model of knowledge in Plato's early dialogues. Oxford University Press on Demand; 2000.
- Gregory V. The Socratic Elenchus. Oxford Studies in Ancient Philosophy.1983;1.
- Lyu W, Wehby GL. Community Use Of Face Masks And COVID-19: Evidence From A Natural Experiment Of State Mandates In The US: Study examines impact on COVID-19 growth rates associated with state government mandates requiring face mask use in public. Health affairs. 2020;39(8):1419-25.
- Leffler CT, Ing E, Lykins JD, Hogan MC, McKeown CA, Grzybowski A. Association of country-wide coronavirus mortality with demographics, testing, lockdowns, and public wearing of masks. Am. J. Trop. Med.2020;103(6):2400.
- Wang X, Ferro EG, Zhou G, Hashimoto D, Bhatt DL. Association between universal masking in a health care system and SARS-CoV-2 positivity among health care workers. Jama. 2020;324(7):703-4.
- Kähler CJ, Hain R. Fundamental protective mechanisms of face masks against droplet infections. J. Aerosol Sci.2020;148:105617.
- Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172(9):577-82.
- MacIntyre CR, Seale H, Dung TC, Hien NT, Nga PT, Chughtai AA et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ open. 2015;5(4):e006577.
- https://allabout.co.jp/gm/gc/486341/
- http://business-up286.com/kenkou/masukuura.html/trackback
- Wu Y, Jing W, Liu J, Ma Q, Yuan J, Wang Y et al. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci. Total Environ. 2020;729:139051.
Citation: Tsuchiya H, Anna T, Kato H, Tsugunori IWAI, Saito H, Koike M (2021) Analysing COVID-19 Infection Clusters Formed when Dining Together using a Time-Workflow Chart (Is this Infection Prevention Method Effective for Omicron-Type Corona?). J Pat Care 7:177. doi: 10.35248/2573- 4598.21.7.177.
Copyright: © 2021 Tsuchiya H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
