Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 17, Issue 6
Alternative Solutions for Addressing ADHD and EB Problems
John Jordan*Received: 01-Aug-2020 Published: 21-Aug-2020, DOI: 10.35248/2090-7214.20.17.360
Abstract
Objective: This article adds to current literature about alternatives to treating ADHD without the administration of pharmaceutical drugs. An estimated 9.4 percent of American children aged 6-17 were diagnosed with ADHD and 62 % of those children were prescribed pharmaceutical drugs to treat behavioral and emotional difficulties, according to a 2016 national parent survey that the CDC released. Today in 2020, about 3 in 4 US children receive treatment of some sort for ADHD, whether medicinal or behavioral (CDC, 2020). Many parents choose to avoid giving their children prescription medicines, leaving their children untreated.
If ADHD or other behavior problems are left unattended, there can be consequences that are irreversible. Current popular treatment methods are suspected by many parents to be dangerous, believing their prescribed youth are being set up for a number of varied consequences later in life. While deemed generally safe, medicines used to treat behavioral and emotional difficulties when misused can produce irreversible long term effects that can otherwise be avoided.
A need for root cause intervention and healthy alternatives to cumulatively toxic medications are needed as alternatives for those parents who opt out of the pharmaceutical route. The understandable choice for natural alternatives will be needed for those parents whose unshakable view of the pharmaceutical salts as “gateway” drugs deter them from altering their children’s brain chemistry, as pharmaceutical salts are aimed to regulate dopamine levels by introducing stimulants into a child’s system such as methylphenidate, amphetamine or atomoxetine, some by themselves and others in combination.
Questions to be considered are: What factors can cause EB problems? What can happen if EB problems are left untreated? What alternatives are there to introducing stimulants into a child’s system?
Keywords
Medicine; Pharmaceutical; Extracurricular activity; Externalizing behavior; Attention-deficit/hyperactivity disorder; Oppositional defiant disorder
Introduction
ADHD during the growing years while a child is developing into adulthood warrants treatment because of the destructive downstream consequences if the condition merely persists. The expression of ADHD during this period may have destructive effects on the entire life course, resulting in fewer friends, school difficulties and dismissals, arrests, unwanted pregnancy, sexually transmitted diseases and abuse of drugs or alcohol [1].
Among the most common treatments are stimulants such as methylphenidate (MPH), amphetamine (AMP) and atomoxetine (ATX).
As parents search for natural alternatives, it is important to introduce options that are grounded in theory and research. Lifestyle changes can provide lifelong remediation and can be brought out through talk therapy or self-differentiating extracurricular activities, effectively providing an environment that encourages self-efficacy and emotion regulation. The positive lifestyle would actively discourage substance abuse and aggressive behaviors, thus reducing emotional and behavior problems [2].
The Factors That Can Cause Eb Problems
Polygenetic biological factors can leave children ill-equipped to manage ordinary tasks of social life. These factors affect behavior and place them at risk for conduct problems, i.e. specific genes (e.g., monoamine oxidase-A, MAOA), may have special relevance in regards to inheritance. Environment will always play a key role in the development of a child, even with an MAOA genetic problem. While genetic issues can be problematic if left unaddressed, they need to be detected before problems emerge so they can be handled with enough care [3]. Genetic problems can be tricky as the occurrence of pleiotropy, where one gene is responsible for the simultaneous emergence of two different characteristics, can lead to the development of both conduct problems and other non-aggressive outcomes, muddying the water when it comes to clear-cut characteristics to diagnose [4].
The behavioral aspect of conduct problems are simple. EB problems indicate a person who is being delayed emotionally and/or socially. The biopsychosocial model outlines biological contributors before analysing the environmental variables. A lack of attention, social problems, aggression, anxious behavior, rule-breaking behavior, depressed behavior, and withdrawn behavior all fall under the same umbrella labeled externalizing behavior (EB) problems. The Fragile Families and Child Wellbeing Study (FFCWS) contains information that indicates the root of many children exhibiting EB problems, Oppositional Defiant Disorders (ODD) and Conduct Disorders (CD) begin with a fragile family.
Environmental elements contributing to a fragile family includes a lack of a semblance of support, warmth and tranquility. The FFCWS follows a cohort of nearly 5,000 children born in the U.S. between 1998 and 2000. The study oversampled births to unmarried couples; and, when weighted, the data are representative of births in large U.S. cities at the turn of the century. Empirical research based on this data has shown inverse relationships between affectionate/supportive partners and their children ’ s behavior problems while there are positive relationships between a couple's unstable relationship and their subsequent children’s behavior problems [5].
Arguments are made by uninformed authoritative agents that when a child is acting out in an undesirable way that child requires medical intervention. These uninformed agents may claim that they have tried their best but nothing has worked. They may have overlooked that within a child ’ s immediate interpersonal structures an absent or disruptive agent, who was formerly a part of that child’s N+2 triad system (spouse, relative, friend, or neighbor), breaks down the developmental process system [6]. Consider the following question, “Do interpersonal familial relationships affect the behavior of a young child ’ s future behavior?”.
There is research that suggests that a change in maternity ward practices affecting the relation between mother and newborn can produce emotional effects still detectable five years later; it is safe to say that a broader type of negative caregiving experiences can lead to EB problems later in life [7]. Marital satisfaction paired with social support are both supported by current research and considered key determinators for the kind of positive parenting that has an inverse relationship with childhood EB problems. Decades of research lends support to Belsky ’ s claim that marital support impacts the relationship quality of the parent-child dyad with regard to the results that showed positive parenting could offer a prediction on an absence of childhood EB’s. Opposition to Belsky’s claim that marital support impacts the relationship quality of the parentchild dyad indicates there is no assured correlation to childhood EB’s when the marital support is insufficient [8].
Consequences If Eb Problems are Left Untreated
The bottom line is this: a child who is showing EB signs indicative of ODD ’ s or CD ’ s needs intervention. While medication can produce immediate results, avoidance of long term use of medicines can cause more harm than good [9], especially when the problems stem from social and psychological circumstances.
More serious cases of EB problems like Conduct Disorder, left untreated, can lead to another psychological condition that is considered to be the most severe and dangerous pathological behaviors in adults, known as Antisocial Personality Disorder [10].
Antisocial behaviors in adolescents are a prevalent problem in our society. Homicide is the second leading cause of death for people ages 10-24 years old, with an additional 656,000 people in the same age group being treated in ERs for violent interactions, with almost one out of five reported being bullied (more females (21.2%) than males(18.7%)) and around one out of six carrying a weapon (17.5%) (CDC). This antisocial and deviant behavior stemming from childhood tends to lead into adolescence and adulthood [4].
Elementary school years will offer a broader pool of adults and peers to offer negative treatment and rejection towards children affected by EB’s, thus cultivating an environment where the child affected by EB’s will develop a survival mentality. Along with these negative experiences, this particular phase of life is a turning point as the peers and support groups chosen by these children affected by EB’s will consist of their deviant peers, while avoiding contact with socially accepted peers [4].
This outsider behavior can potentially set the tone for the rest of the affected childrens’ lives. Drug use related to untreated cases of ADHD is one of the looming consequences forcing caregivers to take action in terms of beginning the administration of pharmaceutical drugs. Furthering the arguments made in favor of pharmaceutical drug administration are valid arguments are sets of data showing that personality traits displayed by those diagnosed with dopamine irregularities such as ADHD are related to adherence, beliefs about ADHD and beliefs about ADHD medicines [1].
The most glaring assumption of introducing drugs into a young person's routine is the long term relationship with drug use, a hypothetical consequence that veers many parents away from administering prescription drugs to their children. Fortunately these concerns are not backed up by research, as addiction to the ADHD medicines are not regarded as problematic in most cases (AAC, 2020). As Biosemiotic Entropy would apply to broad drug use in general, the relation of pediatric ADHD prescription adherence to a future of drug abuse could be best understood as a degenerate instance of a string of logic ($πϕ)i [11].
Several studies suggest that boys with ADHD, when left untreated, are more likely to develop drug and alcohol problems than boys with ADHD who were treated with stimulants [9]. The development of drug and alcohol problems later in life are symptomatic of psychological obstacles that were either not addressed or intervened upon early enough, as the CDC reports on their website, “ Many children with ADHD have other disorders as well as ADHD, such as behavior or conduct problems, learning disorders, anxiety and depression” [12].
Human biosignaling systems can be disrupted by noxious chemicals in the air we breathe, the water we drink, and the food we eat, it is the medicines swallowed or injected into our bodies that are the most likely to cause harm and even fatalities [11]. Reliance on medications can begin a vicious cycle, as when an adult with a substance abuse problem becomes pregnant, a child in utero is then exposed to a toxic or diseased prenatal environment. The child can be born with a hyper persistent behavior facilitation system, an underactive behavior inhibition system, autonomic nervous system hyperreactivity, cognitive problems in sustaining attention to cues, low cerebrospinal fluid concentrations of serotonin metabolites (5-HIAA, which affects delay of gratification), or a difficult style of temperament [4]. Children born with any single or comorbidity of these conditions will be candidates for more medicinal treatments, possibly for their entire life.
Current knowledge about the overlap of early drug abuse and ADHD is compelling as a 2014 study examined a sample consisting of 124 (13.2%) participants who reported a history of ADHD and 817 (86.8%) who reported no history of ADHD. The study produced evidence that ADHD history indeed accelerated the Gateway Theory of drug use [13]. The study showed that a history of self-reported ADHD was significantly associated with younger ages of experimentation with alcohol, cigarettes, marijuana, and cocaine as well as injection drug use and needle sharing. The abuse of ADHD medicine comes as no surprise as it can be easily distributed and most people display some sort of symptoms of ADHD at some time, such as inattention, restlessness, and fidgeting [9].
The adulthood abuse of these drugs are problematic and can be indicative of substance abuse problems if taken as “club” or “ dance ” drugs, because the stimulants are similar to amphetamines, increasing energy and enhancing mood [9]. Ritalin (MPH) is similar to some illicit street drugs, MPH leads to a more general increase of dopamine in the brain, and while in another category of pharmaceuticals, ATX is also relatable to street drugs as it functions by increasing norepinephrine selectively and dopamine indirectly in the frontal cortex. The methods of prescribing medications that are considered common practice will not take into account the adverse effects of long term use of these commonly prescribed medicines and here it becomes clear that the risks of using medications of this nature without absolute necessity is likely to outweigh the short term benefits of doing so.
This should be reiterated by stating that our bodies rely on communication between our biosignaling systems to function. These biosignaling systems connect everything from the microbes in our intestines to the highest centers in our brains, and it is known that deeply-layered biological signaling systems control the development of our bodies in ways that are shaped from even before conception. These functioning biosignaling systems are prerequisite to not only “ordinary experience”, but foundational towards the avoidance of disorders, diseases, and premature death [11].
There is evidence to suggest a dissociation between activation of the drug Adderall and neurocognition during the temporary medicated state of healthy college students. This is contrary to the supposition that there is an improved state of neurocognition and academic performance while dosed with a safe amount of Adderall [14]. This 2108 study is noted for its need to be reproduced with a larger study group however it illuminates a simple fact that these stimulants are only behavior modifiers and not the cognitive enhancers that the general public believes them to be.
Alternatives to Introducing Medicine Into a Child’s System
Early screening has a strong potential to enable effective intervention. If implemented as public policy, a school ’ s counselors or SLPs can play an active role in identifying children who can benefit from preventative intervention [4]. By investigating root cause scenarios it can be determined that alternatives to medicinal doping can be implemented. The line of thinking that supports giving a child medicine for their behavior is problematic as studies have shown that fragile families and weak support systems are influential on the psychological and social status of a child.
Sending a child to a therapist or counselor would probably seem like one way to avoid medicating the child, however a healing of the entire family unit is necessary, as higher levels of differentiation of self have been associated with positive parent couple relationships [15]. The difficulties arise when one or more persons in the N+2 family system are unwilling or unable to attend and grow from therapeutic sessions, in these cases an extracurricular activity can fill a portion of the family role by providing positivity to children in a fragile family. An extracurricular activity ingrained with a philosophical backbone can use positive reinforcement techniques to influence behaviors that are presently deemed non volitional and incorrigible. It is to be noted that without consistent attendance results may be modest.
In the case of a defective N+2 support structure, a very particular brand of extracurricular activity will need to be chosen, since not every activity or sport is a miraculous one-sizefits- all solution. A scale of measure to ensure that a chosen activity is appropriate for the use as an alternative to medicinal interventions is suggested. A suitable activity would need to teach a mixture of skills for the body and mind(Figure 1).
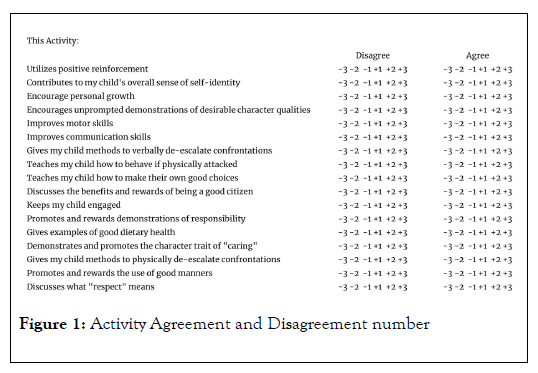
Figure 1: Activity Agreement and Disagreement number
The activity would need to improve active listening skills and strengthen them through games that disguise repetition, to avoid losing a child’s interest. Keeping a child’s interest is paramount for a well designed program. Over the course of a year, items of discussion (pertaining to essential character traits) should shift focus on the varietal meaning and importance of being a morally bound person who follows rules. As an option attendees can be awarded points for following rules that are to be tracked by the caregiver, to be awarded later. The main focus should be teaching traits that will develop both their psychological growth (responsibility, health, and caring) alongside social growth (respect, citizenship, and manners).
The ongoing lesson plan should positively reinforce traits in the child, especially when the child is reportedly engaging in these behaviors in their day to day activities. The eventualization of a child performing these characteristics unprompted is the outright goal. Of course, the system would fall apart without the potential reward of fun and games, so once a child has met an age-determined “game-point score”, they should be rewarded. The children who have succeeded in exhibiting the spectrum of positive traits should be invited to a special day full of fun and games, along with an award that can be attached to a piece of clothing, serving as a literal badge of honor.
The ability to be less affected by external family or social stimuli and retain one ’ s individuality [7] will be instrumental in avoidance of the two subtypes of poorly differentiated people, chameleons and bullies [16]. Differentiation of self is a hallmark of a person who is not easily affected by external familial or social factors, while someone with low self-differentiation will forcefully control others, seek attention/ approval from others by using fear sometimes betraying their own personal authenticity to do so. Verbal skill development will be one expression of self-differentiation, these skills are not only for use against their oppressive peers but for abduction prevention as well. A variety of interpersonal skills to be used to de-escalate delicate situations or to establish boundaries between peers or adults will need to be present in the selected program. The social tools implanted in well-designed programs must include how to effectively set boundaries by using verbal skills.
Beyond interpersonal communication skills there is also a need for discussions on how to physically engage an active aggressor without inflammatory tactics like using punches or kicks, pulling hair, biting, twisting fingers, or using weapons. Proprioceptive natural gymnastic movements should be used, these movements are to be aimed to begin fine tuning gross motor skills into specific musculature synchronizations; these skills are to be found especially beneficial by those with low muscle tone or bradykinesia. Development of gross motor skills will begin to take effect after consistent practice. A suitable activity should empower it ’ s practitioners by utilizing selfacceptance with emphasis on differentiation of self. Each child’s own rate for personal growth will vary, and some children may need special one on one attention without distractions. Discussions and demonstrations would need to outline exactly how to defend against up to three dozen specific physical attacks, how to use minimal force in controlling each unique situation, and the necessary streamlined negotiation skills to be used amidst any physical altercation that is deemed both unavoidable and inevitable.
A third alternative often considered, aside from talk therapy and boundary building self-differentiating extracurricular activities, is a mindful approach to diet. There is considerable satisfaction regarding the administrations of probiotic supplements to modulate the gut microbiota and interact with the immune system when used with minor disorders [17]. When synbiotics, immune stimulants, and omega-3 Polyunsaturated Fatty Acids (PUFAs) are administered by pediatricians to children, depending on age and with minor disorders, a high satisfaction rating of “very satisfied ” was reported by parents in a 2019 Spanish study [18].
While approaches that involve removal of diet items or an addition of supplements may vary, once again, there are methods that address the behavior and not the biology. The use of non-food regulation (appetite self-regulation) as a means to better learn general self-regulation has been noted to be a crucial component to be included under the umbrella of self-regulation skills to be learned in childhood, along with other non-food related criteria [19]. The deciding factors when it comes to choosing a behavior based approach over a diet-based and/or supplement based approach will be determined by the child’s N +2 team.
Setting satisfaction reports aside, when looking into dietary changes to alter all types of undesirable behaviors in children, there is not enough supportive evidence that treating ADHD [20] with diet intervention can succeed, there is certainly little or no evidence that dietary changes are all that may be needed [21]. Indeed there are subgroups of children and adolescents that will benefit from elimination of some food items from their diet. There are also other options to address behavior problems without the use of pharmaceutical drugs [22]. The most effective of these options are more intensive and demanding than simply administering medication to the child [23]. While there are no quick fixes to be found at the moment in terms of dietary replacements for pharmaceutical drugs [24] there is reason to believe improvement is possible and the use of dietary changes are relatively less dangerous than addictive and toxic medications [25].
Conclusion
While more long term studies will be required, the current theory and research suggests that a therapeutic and supportive form of treatment can address undesirable behaviors with long term positive yields. When better understood, proactive treatments and environmental activities will offset many of the social and psychological factors that tend only to perpetuate EB problems.
Streamlined and structured activities that would suffice for a N +2 system designed with philosophies in mind that maintain a presence in the day to day lives of the participants should use positive reinforcement further incentivising progression. The work that has been done so far has been extremely helpful to set the stage for the unprecedented implementation of intelligent methods to circumvent medicinal intervention in early childhood, changing the course of many young people’s lives.
REFERENCES
- Emilsson M, Gustafsson PA, Öhnström G, Marteinsdottir I. Beliefs Regarding Medication and Side Effects Influence Treatment Adherence in Adolescents with Attention Deficit Hyperactivity Disorder. Eur Child Adolesc Psychiatry. 2017;26(5):559-571.
- Nina K, Bürgin D, Clemens V, Jenkel N, Schmid M. Disrupting the Disruption Cycle – A Longitudinal Analysis of Aggression Trajectories, Quality of Life, Psychopathology and Self-Efficacy in Closed Youth Residential Care. Children and Youth Services Review. 2020;112
- Byrd A, Manuck S, Hawes S, Vebares T, Nimgaonkar V, Chowdari K, et al. The interaction between monoamine oxidase A (MAOA) and childhood maltreatment as a predictor of personality pathology in females: Emotional reactivity as a potential mediating mechanism – ERRATUM. Development and Psychopathology. 2019;31(1):393-393.
- Dodge KA, Gregory SP. A Biopsychosocial Model of the Development of Chronic Conduct Problems in Adolescence. Developmental Psychology. 2003;39(2):349-371.
- Lovett, Erin Wallace. Couples’ Relationship Qualities and Child Behavior Problems. LSU Digital Commons. 2020.
- Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Harvard University Press, Cambridge, Massachusetts, United States. 1979.
- Kerr M, Bowen M. Family evaluation: An approach based on Bowen theory. Norton, W. W. & Company, New York, United States. 1988.
- Boric AS, Roscic S, Sedmak M, Sepcevic, A, Kerestes G. Social-contextual determinants of parental behaviour of preschool children’s mothers and fathers. Croatian Journal Educational. 2011;13(3):25-42.
- Stephen AM, Galizio M, Connors GJ. Drug Use and Abuse. 2011.
Citation: Jordan J (2020) Alternative Solutions for Addressing ADHD and EB Problems. Clinics Mother Child Health. 17:360.
Copyright: © 2020 Jordan J This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

