Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2023) Volume 7, Issue 3
A Case of Diffuse Alveolar Haemorrhage in a Postoperative Patient with Lower Limb Fractures
Shiraz Assu1* and Deepak Bhasin22Department of Pulmonary Critical Care Medicine, Max Hospital, Mohali, Punjab, India
Received: 03-Aug-2023, Manuscript No. JSA-23-22439; Editor assigned: 07-Aug-2023, Pre QC No. JSA-23-22439 (PQ); Reviewed: 21-Aug-2023, QC No. JSA-23-22439; Revised: 28-Aug-2023, Manuscript No. JSA-23-22439 (R); Published: 04-Sep-2023, DOI: 10.35248/2684-1606.23.07.224
Abstract
Fat embolism syndrome is a life-threatening complication in patients with orthopedic trauma, especially after long bone fractures. It can lead to multi-organ dysfunction with respiratory involvement ranging from mild hypoxia to severe acute respiratory distress syndrome. Here, we report a case of fat embolism in a patient with lower limb long bone fractures, which postoperatively lead to Diffuse Alveolar Haemorrhage (DAH). The diagnosis was made only by a high index of clinical suspicion since DAH is only rarely associated with fat embolism. The patient received supportive management and a short course of intravenous methylprednisolone following which he showed clinical improvement.
Keywords
Trauma, Fat embolism syndrome, Diffuse alveolar haemorrhage, Steroids
Introduction
Fat Embolism Syndrome (FES) affects multiple organ systems following trauma, especially of long bones of the lower extremities. Even though fat emboli develop in many patients with bone fractures, most of them are usually asymptomatic. A minority of patients develop signs and symptoms of organ system dysfunction after an asymptomatic period of 12-72 hours. Its diagnosis is mostly clinical, with laboratory and radiological tests being non-specific and insensitive. Diffuse Alveolar Haemorrhage (DAH) is very rarely reported to be associated with FES. Here we report a case of traumatic fat embolism presenting as DAH, which was diagnosed based only on high clinical suspicion and was treated successfully with steroids and other supportive management.
Case Presentation
A 23-year-old male was brought to the emergency with closed fracture of the shaft of the right femur and open grade 1 fractures of the shaft of right tibia and fibula (Figure 1), following a road traffic accident. An orthopaedic consult was taken and it was planned to surgically fix the fractures. Except for a drop in Hb (Haemoglobin) from 13 g/dL to 11.5 g/dL, his other preoperative investigations, including chest X-ray were normal (Figure 2). General anesthesia was administered and he underwent Closed Reduction and Internal Fixation (CRIF) of the fractures. Intra-operatively the patient was noted to be having hypoxia (PF ratio of 188.4) and tachycardia (with HR of 100-120/min), but it was possible to extubate him postoperatively to 4 l/min of O2, administered via nasal prongs. Despite insignificant intraoperative blood loss, his post-operative Hb dropped further to 8.4 g/ dL, following which 1 unit of Packed Red Blood Cells (PRBC) was transfused. On postoperative day 2, hypoxia persisted (requiring O2 at 2-4 l/min via nasal prongs) and he also started having episodes of haemoptysis with a further drop in Hb to 7.3 gm/dl. During this time he was afebrile and hemodynamically stable, but his chest X-ray showed bilateral diffuse infiltrates (Figure 3). Hence a CT pulmonary angiography was done which showed no evidence of any focal filling defect in pulmonary vessels, but patchy and confluent ground-glass opacification was noted in bilateral lungs s/o Acute Respiratory Distress Syndrome (ARDS) (Figure 4). A provisional clinical diagnosis of DAH associated with FES was made and methyl-prednisolone at 1 mg/ kg/day was started along with transfusion of 1 more unit of packed red blood cells. By postoperative day 7 and after 3 days of starting steroids, he started showing clinical and radiological improvement with O2 being tapered and stopped, no more haemoptysis and clearing of serial chest X-rays (Figure 5). His hemoglobin level was maintained at around 10 gm/dl and he was discharged on post-op day 10 with a tapering dose of steroids.
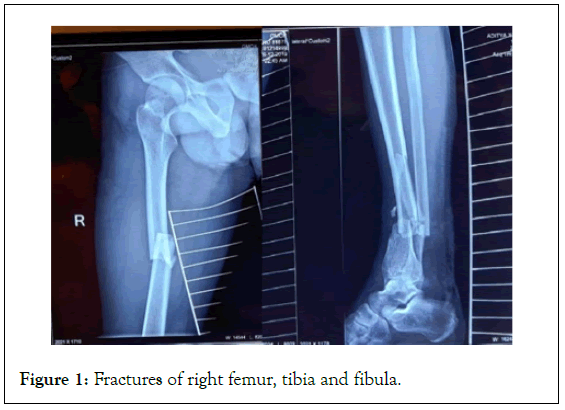
Figure 1: Fractures of right femur, tibia and fibula.
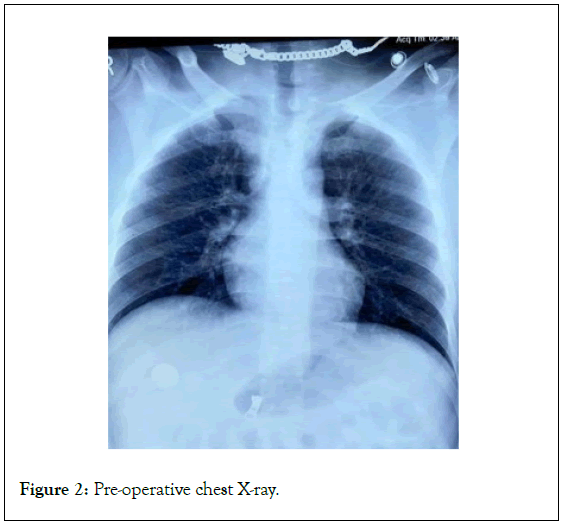
Figure 2: Pre-operative chest X-ray.
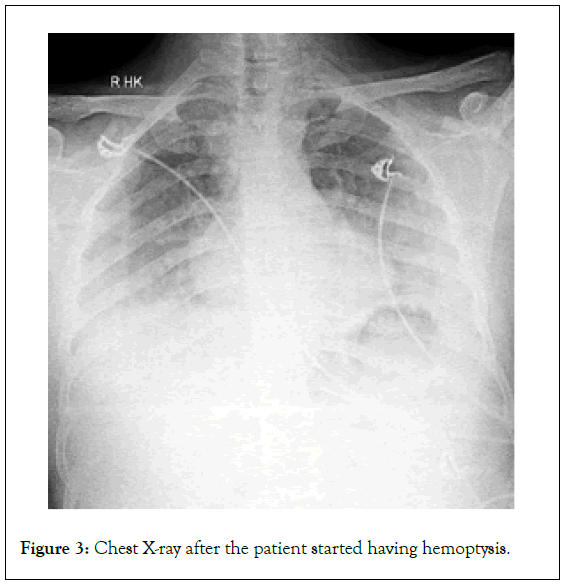
Figure 3: Chest X-ray after the patient started having hemoptysis.
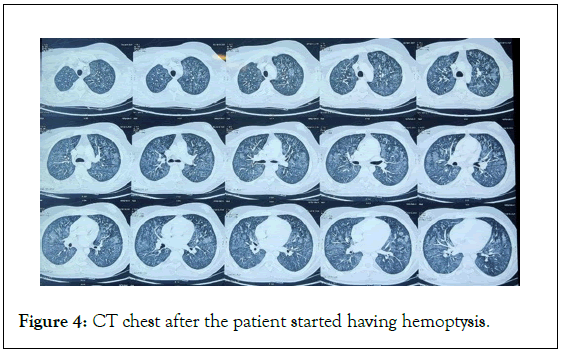
Figure 4: CT chest after the patient started having hemoptysis.
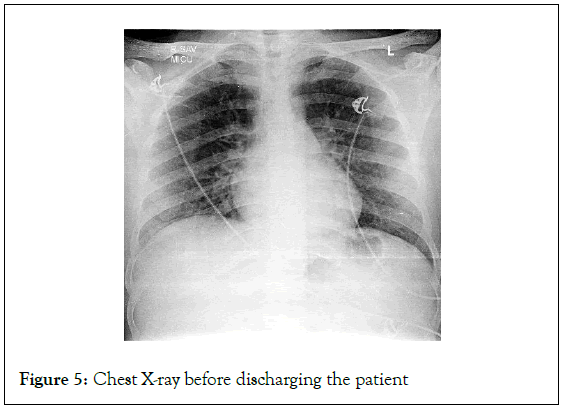
Figure 5: Chest X-ray before discharging the patient
Results and Discussion
Major causes of fat embolism syndrome are skeletal fractures associated with trauma and following surgical manipulations of these fractures. Two main theories are proposed to explain its pathology, the mechanical theory and the biochemical theory [1,2]. FES is characterized by an asymptomatic interval of about 12 to 72 hours after the initial insult, followed by a classical triad of respiratory insufficiency, petechial rash, and neurologic manifestation. In symptomatic, pulmonary manifestations are the earliest and can be seen in 75% of patients, with hypoxia being the most common sign [3]. Neurological manifestations are usually nonspecific and may present as headache, acute confusion, convulsion, or as severe as coma. Petechial rashes are usually distributed in nondependent regions of the body such as conjunctivae, head, neck, anterior thorax, or axillary areas. Other nonspecific symptoms include fever, thrombocytopenia, jaundice, lipuria, haematuria, and retinopathy [4]. In our case also, 48 hours after trauma, the patient started having hypoxia which was followed by haemoptysis. Even though there are many criteria described to diagnose FES, many times presentations are atypical and mild cases of FES may be unnoticed [5,6]. Laboratory findings in FES are usually nonspecific. Our patient had hypoxia, tachycardia and anemia which doesn’t satisfy any clinical criteria for fat embolism, but it’s the clinical context and high index of suspicion that helped us in the diagnosis. The severity of the condition can vary, most cases are self-limiting, but mortality has been reported as high as 5%–15% [7].
DAH is a syndrome caused by injury or inflammation of arterioles, venules or alveolar septal capillaries and is associated with a rare variety of disease processes. The usual presentation is cough, haemoptysis, fever and dyspnoea and in absence of haemoptysis new radiographic opacities (either localized or diffuse), a falling haemoglobin level, and the finding of increasingly haemorrhagic fluid on sequential Bronchoalveolar Lavage (BAL) favor the diagnosis. CT scanning typically shows ground glassing or consolidative opacities that are diffuse and bilateral but may occasionally be unilateral. The association of fat embolism and DAH has rarely been reported [8]. Our patient on postoperative day 2 had cough, haemoptysis, a drop in Hb with diffuse infiltrates in chest x-ray and bilateral diffuse Ground-Glass Opacities (GGO’s) in CT, all of which prompted us to make a clinical diagnosis of DAH.
The mainstay in the management of FES is prevention and supportive care. Early surgical fixation and, decreasing the reaming time can reduce the number of emboli [9]. In patients with suspected DAH, when an underlying cause is identified, specific treatment for the same is done. Otherwise, the treatment is again supportive; including transfusing blood to prevent severe anemia. Since most of the causes leading to DAH are immune-mediated, the mainstay of treatment in most cases are steroids and immunosuppression. Despite a lack of definite evidence for use of steroids in FES or DAH associated with non-immune triggers, our patient improved with low dose steroids (methylprednisolone started at 40 mg twice daily and tapered over 2 weeks) along with fluid resuscitation (crystalloids and blood products) and respiratory support.
Conclusion
To conclude, FES can rarely present as DAH in patients following major orthopaedic trauma or their surgical manipulations. Its diagnosis is essentially clinical and can be missed unless we have a high index of suspicion. Although there are no large scale studies to support the use of steroids in such a condition, we found good results with early use of low dose methylprednisolone.
Conflicts of Interest
There are no conflicts of interest.
References
- Gossling HR, Pellegrini Jr VD. Fat embolism syndrome: A review of the pathophysiology and physiological basis of treatment. Clin Orthop Relat Res. 1982;165:68-82.
[Crossref] [Google Scholar] [PubMed]
- Baker PL, Pazell JA, Peltier LF. Free fatty acids, catecholamines, and arterial hypoxia in patients with fat embolism. J Trauma. 1971;11(12):1026-1030.
[Crossref] [Google Scholar] [PubMed]
- Powers KA, Talbot LA. Fat embolism syndrome after femur fracture with intramedullary nailing: case report. Am J Crit Care. 2011;20(3):267-276.
[Crossref] [Google Scholar] [PubMed]
- Bulger EM, Smith DG, Maier RV, Jurkovich GJ. Fat embolism syndrome: A 10-year review. Arch Surg. 1997;132(4):435-439.
[Crossref] [Google Scholar] [PubMed]
- Gurd AR. Fat embolism: An aid to diagnosis. J Bone Joint Surg Br.1970;52(4):732-737.
[Crossref] [Google Scholar] [PubMed]
- Schonfeld SA, Ploysongsang Y, Dilisio RA, Crissman JD, Miller E, Hammerschmidt DE, et al. Fat embolism prophylaxis with corticosteroids: A prospective study in high-risk patients. Ann Intern Med.1983;99(4):438-443.
[Crossref] [Google Scholar] [PubMed]
- Mellor A, Soni N. Fat embolism. Anaesthesia. 2001;56(2):145-54.
[Crossref] [Google Scholar] [PubMed]
- Alkhazna A, Gohar A, Saeed A, Taha H. Fat embolism syndrome presenting as diffuse alveolar hemorrhage. Chest. 2012;142(4):973A.
- Shaikh N, Parchani A, Bhat V, Kattren MA. Fat embolism syndrome: clinical and imaging considerations: Case report and review of literature. Indian J Crit Care Med. 2008;12(1):32.
[Crossref] [Google Scholar] [PubMed]
Citation: Assu S, Bhasin D (2023) A Case of Diffuse Alveolar Haemorrhage in a Postoperative Patient with Lower Limb Fractures. J Surg Anesth. 7:224.
Copyright: © 2023 Assu S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
